J Korean Med Sci.
2020 Jun;35(25):e232. 10.3346/jkms.2020.35.e232.
Compliance of Antihypertensive Medication and Risk of Coronavirus Disease 2019: a Cohort Study Using Big Data from the Korean National Health Insurance Service
- Affiliations
-
- 1Institute of Artificial Intelligence and Big Data in Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea
- 2Big Data Department, National Health Insurance Service, Wonju, Korea
- 3Department of Internal Medicine, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea
- 4Division of Infectious Diseases, Department of Internal Medicine, Seoul National University College of Medicine, Seoul National University Bundang Hospital, Seongnam, Korea
- 5Department of Social and Preventive Medicine, Sungkyunkwan University School of Medicine, Suwon, Korea
- 6Health Insurance Policy Research Institute, National Health Insurance Service, Wonju, Korea
- 7Department of Preventive Medicine, Hanyang University College of Medicine, Seoul, Korea
- KMID: 2503661
- DOI: http://doi.org/10.3346/jkms.2020.35.e232
Abstract
- Background
There is a controversy whether it is safe to continue renin-angiotensin system blockers in patients with coronavirus disease 2019 (COVID-19). We analyzed big data to investigate whether angiotensin-converting enzyme inhibitors and/or angiotensin II receptor blockers have any significant effect on the risk of COVID-19. Population-based cohort study was conducted based on the prescription data from nationwide health insurance records.
Methods
We investigated the 1,374,381 residents aged ≥ 40 years living in Daegu, the epicenter of the COVID-19 outbreak, between February and March 2020. Prescriptions of antihypertensive medication during the year before the outbreak were extracted from the National Health Insurance Service registry. Medications were categorized by types and stratified by the medication possession ratios (MPRs) of antihypertensive medications after controlling for the potential confounders. The risk of COVID-19 was estimated using a difference in difference analysis.
Results
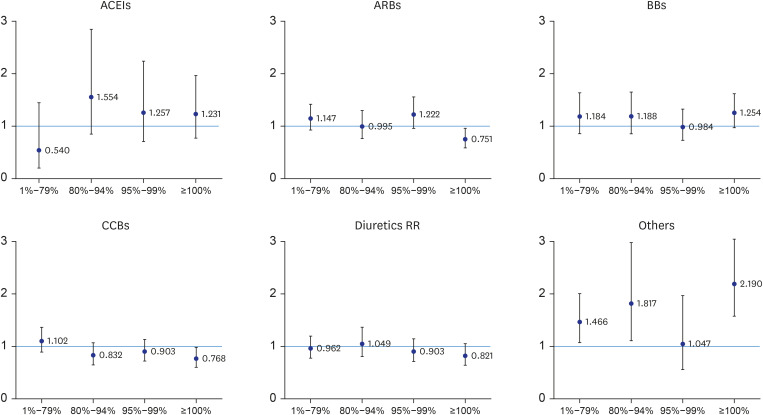
Females, older individuals, low-income earners, and recently hospitalized patients had a higher risk of infection. Patients with higher MPRs of antihypertensive medications had a consistently lower risk of COVID-19 than those with lower MPRs of antihypertensive medications and non-users. Among patients who showed complete compliance, there was a significantly lower risk of COVID-19 for those prescribed angiotensin II receptor blockers (relative risk [RR], 0.751; 95% confidence interval [CI], 0.587–0.960) or calcium channel blockers (RR, 0.768; 95% CI, 0.601–0.980).
Conclusion
Renin-angiotensin system blockers or other antihypertensive medications do not increase the risk of COVID-19. Patients should not stop antihypertensive medications, including renin-angiotensin system blockers, because of concerns of COVID-19.
Keyword
Figure
Cited by 1 articles
-
Soluble ACE2 and TMPRSS2 Levels in the Serum of Asthmatic Patients
Ji-Hyang Lee, Chae Eun Lee, Youngsang Yoo, Eunyong Shin, Jin An, Seo Young Park, Woo-Jung Song, Hyouk-Soo Kwon, You Sook Cho, Hee-Bom Moon, Tae-Bum Kim
J Korean Med Sci. 2022;37(8):e65. doi: 10.3346/jkms.2022.37.e65.
Reference
-
1. Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020; 382(13):1199–1207. PMID: 31995857.2. Mahase E. Covid-19: WHO declares pandemic because of “alarming levels” of spread, severity, and inaction. BMJ. 2020; 368:m1036. PMID: 32165426.
Article3. World Health Organization. Coronavirus Disease 2019 (COVID-19): Situation Report, 126. Geneva: World Health Organization;2020.4. Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020; 395(10229):1054–1062. PMID: 32171076.
Article5. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020; 382(18):1708–1720. PMID: 32109013.6. Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA. 2020; 323(16):1574–1581.
Article7. Li W, Moore MJ, Vasilieva N, Sui J, Wong SK, Berne MA, et al. Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature. 2003; 426(6965):450–454. PMID: 14647384.
Article8. Patel AB, Verma A. COVID-19 and angiotensin-converting enzyme inhibitors and angiotensin receptor blockers: what is the evidence? JAMA. Forthcoming. 2020; DOI: 10.1001/jama.2020.4812.
Article9. Vaduganathan M, Vardeny O, Michel T, McMurray JJ, Pfeffer MA, Solomon SD. Renin-angiotensin-aldosterone system inhibitors in patients with COVID-19. N Engl J Med. 2020; 382(17):1653–1659. PMID: 32227760.
Article10. Wang K, Gheblawi M, Oudit GY. Angiotensin converting enzyme 2: a double-edged sword. Circulation. Forthcoming. 2020; DOI: 10.1161/CIRCULATIONAHA.120.047049.11. Central Disaster Management Headquarters of Ministry of Health and Welfare of Korea. Case definitions. Updated 2020. Accessed April 2, 2020. http://ncov.mohw.go.kr/en/baroView.do?brdId=11&brdGubun=112&dataGubun=&ncvContSeq=&contSeq=&board_id=&gubun=.12. Korean Society of Infectious Diseases. Korea Centers for Disease Control and Prevention. Analysis on 54 mortality cases of coronavirus disease 2019 in the Republic of Korea from January 19 to March 10, 2020. J Korean Med Sci. 2020; 35(12):e132. PMID: 32233161.13. Fang L, Karakiulakis G, Roth M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir Med. 2020; 8(4):e21. PMID: 32171062.
Article14. Onder G, Rezza G, Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA. Forthcoming. 2020; DOI: 10.1001/jama.2020.4683.
Article15. Diaz JH. Hypothesis: angiotensin-converting enzyme inhibitors and angiotensin receptor blockers may increase the risk of severe COVID-19. J Travel Med. 2020; 27(3):taaa041. PMID: 32186711.
Article16. Zheng YY, Ma YT, Zhang JY, Xie X. COVID-19 and the cardiovascular system. Nat Rev Cardiol. 2020; 17(5):259–260. PMID: 32139904.
Article17. Kuster GM, Pfister O, Burkard T, Zhou Q, Twerenbold R, Haaf P, et al. SARS-CoV2: should inhibitors of the renin-angiotensin system be withdrawn in patients with COVID-19? Eur Heart J. 2020; 41(19):1801–1803. PMID: 32196087.
Article18. Danser AHJ, Epstein M, Batlle D. Renin-angiotensin system blockers and the COVID-19 pandemic: at present there is no evidence to abandon renin-angiotensin system blockers. Hypertension. 2020; 75(6):1382–1385. PMID: 32208987.19. Zhang L, Sun Y, Zeng H-L, Peng Y, Jiang X, Shang W-J, et al. Calcium channel blocker amlodipine besylate is associated with reduced case fatality rate of COVID-19 patients with hypertension. Updated 2020. Accessed April 2, 2020. https://www.medrxiv.org/content/10.1101/2020.04.08.20047134v1.20. de Miguel-Díez J, Jiménez-García R, Hernández-Barrera V, Maestu LP, Aparicio IJ, Ramos AO, et al. Clustering of unhealthy lifestyle behaviors is associated with a low adherence to recommended preventive practices among COPD patients in Spain. COPD. 2014; 11(4):459–467. PMID: 24568374.
Article21. Li J, Wang X, Chen J, Zhang H, Deng A. Association of renin-angiotensin system inhibitors with severity or risk of death in patients with hypertension hospitalized for coronavirus disease 2019 (COVID-19) infection in Wuhan, China. JAMA Cardiol. Forthcoming. 2020; DOI: 10.1001/jamacardio.2020.1624.
Article22. Zhang P, Zhu L, Cai J, Lei F, Qin JJ, Xie J, et al. Association of inpatient use of angiotensin converting enzyme inhibitors and angiotensin II receptor blockers with mortality among patients with hypertension hospitalized with COVID-19. Circ Res. 2020; 2020; 126(12):1671–1681. PMID: 32302265.23. Mizumoto K, Kagaya K, Zarebski A, Chowell G. Estimating the asymptomatic proportion of coronavirus disease 2019 (COVID-19) cases on board the Diamond Princess cruise ship, Yokohama, Japan, 2020. Euro Surveill. 2020; 25(10):2000180.
Article24. Oran DP, Topol EJ. Prevalence of asymptomatic SARS-CoV-2 infection: a narrative review. Ann Intern Med. 2020; M20–3012.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Introducing big data analysis using data from National Health Insurance Service
- Pediatric Cancer Research using Healthcare Big Data
- The risk of stroke according to statin medication compliance in older people with chronic periodontitis: an analysis using the Korea National Health Insurance Service-Senior Cohort Database
- A comparison of methods for the measurement of adherence to antihypertensive multidrug therapy and the clinical consequences: a retrospective cohort study using the Korean nationwide claims database
- Methodology for Big Data Analysis Using Data from National Health Insurance Service: Preliminary Methodologic Study and Review about the Relationship between Sinus Surgery and Asthma