Ann Surg Treat Res.
2020 Jul;99(1):18-25. 10.4174/astr.2020.99.1.18.
Preoperative predictive factors of pancreatic fistula after pancreaticoduodenectomy: usefulness of the CONUT score
- Affiliations
-
- 1tment of Surgery, National Hospital Organization, Iwakuni Clinical Center, Yamaguchi, Japan
- KMID: 2503456
- DOI: http://doi.org/10.4174/astr.2020.99.1.18
Abstract
- Purpose
Postoperative pancreatic fistula (POPF) is the most important factor affecting morbidity and mortality after pancreaticoduodenectomy (PD). Patients with a high controlling nutritional status (CONUT) score, which is used to assess nutritional status, are expected to have high morbidity rates. This study aimed to determine the usefulness of the CONUT score.
Methods
Data from 97 consecutive cases of PD performed in the Department of Surgery of Iwakuni Clinical Center, from April 2008 to May 2018, were included. Preoperative patient data, including sex, age, and hypertension, and postoperative complication data were collected to analyze pancreatic fistula occurrence.
Results
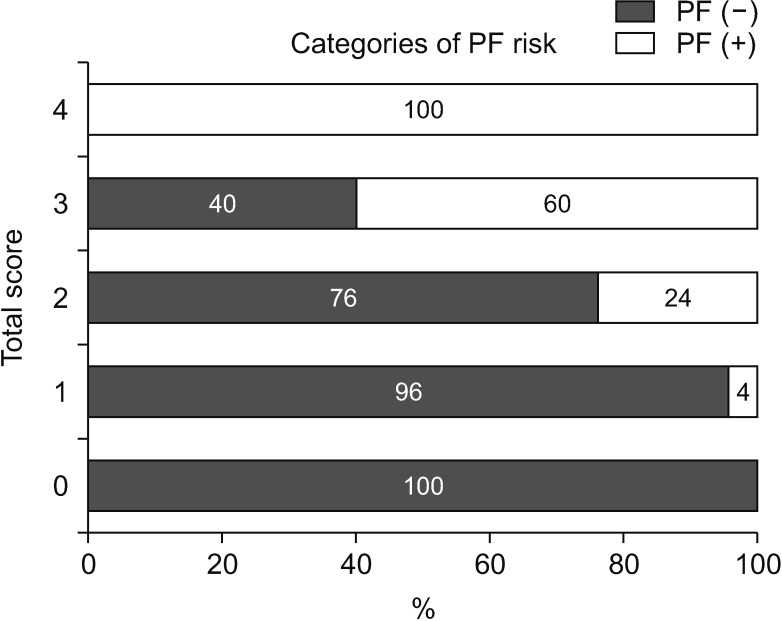
Of the 97 patients, 2 9 patients (29.8%) were diagnosed with POPF ≥ B, with 26 cases (26.8%) classified as grade B and 3 (3.1%) as grade C. The mortality rate was 2.1% (2 of 97). In the univariate analysis, a significant association was observed between POPF and the following factors: body mass index (BMI) ≥ 22 kg/m2, high CONUT score, nonpancreatic carcinoma, and CT attenuation values. In multivariate analysis, BMI ≥ 22 kg/m2 (odds ratio [OR], 6.16; P < 0.001), high CONUT score (OR, 3.77; P = 0.009), nonpancreatic carcinoma (OR, 5.72; P = 0.009), and CT attenuation values (late/early ratio) in the pancreas (OR, 9.07; P = 0.006) were independent risk factors for POPF.
Conclusion
Patients with a high CONUT score are at high risk of POPF. Further study correlating preoperative nutritional intervention with risk of POPF is necessary.
Figure
Cited by 1 articles
-
Unfavorable effect of high postoperative fluid balance on outcome of pancreaticoduodenectomy
Hyun-Jeong Jeon, Hyung-Jun Kwon, Yoon-Jin Hwang, Sang-Geol Kim
Ann Surg Treat Res. 2022;102(3):139-146. doi: 10.4174/astr.2022.102.3.139.
Reference
-
1. Brown EG, Yang A, Canter RJ, Bold RJ. Outcomes of pancreaticoduodenectomy: where should we focus our efforts on improving outcomes? JAMA Surg. 2014; 149:694–699. PMID: 24849180.2. Kimura W, Miyata H, Gotoh M, Hirai I, Kenjo A, Kitagawa Y, et al. A pancreaticoduodenectomy risk model derived from 8575 cases from a national single-race population (Japanese) using a web-based data entry system: the 30-day and in-hospital mortality rates for pancreaticoduodenectomy. Ann Surg. 2014; 259:773–780. PMID: 24253151.3. Fang Y, Gurusamy KS, Wang Q, Davidson BR, Lin H, Xie X, et al. Pre-operative biliary drainage for obstructive jaundice. Cochrane Database Syst Rev. 2012; 9:CD005444.4. Winter JM, Cameron JL, Yeo CJ, Alao B, Lillemoe KD, Campbell KA, et al. Biochemical markers predict morbidity and mortality after pancreaticoduodenectomy. J Am Coll Surg. 2007; 204:1029–1036. PMID: 17481534.5. Sugimoto M, Takahashi S, Gotohda N, Kato Y, Kinoshita T, Shibasaki H, et al. Schematic pancreatic configuration: a risk assessment for postoperative pancreatic fistula after pancreaticoduodenectomy. J Gastrointest Surg. 2013; 17:1744–1751. PMID: 23975030.6. Liu QY, Zhang WZ, Xia HT, Leng JJ, Wan T, Liang B, et al. Analysis of risk factors for postoperative pancreatic fistula following pancreaticoduodenectomy. World J Gastroenterol. 2014; 20:17491–17497. PMID: 25516663.7. Reid-Lombardo KM, Farnell MB, Crippa S, Barnett M, Maupin G, Bassi C, et al. Pancreatic anastomotic leakage after pancreaticoduodenectomy in 1,507 patients: a report from the Pancreatic Anastomotic Leak Study Group. J Gastrointest Surg. 2007; 11:1451–1458. PMID: 17710506.8. Jang JY, Shin YC, Han Y, Park JS, Han HS, Hwang HK, et al. Effect of polyglycolic acid mesh for prevention of pancreatic fistula following distal pancreatectomy: a randomized clinical trial. JAMA Surg. 2017; 152:150–155. PMID: 27784046.9. Kwon HJ, Ha HT, Choi YY, Kim SG. The effects of the end-to-side inverted mattress pancreaticojejunostomy on postoperative pancreatic fistula: a single surgeon's experience. Ann Surg Treat Res. 2015; 89:61–67. PMID: 26236694.10. Ignacio de Ulíbarri J, González-Madroño A, de Villar NG, González P, González B, Mancha A, et al. CONUT: a tool for controlling nutritional status. First validation in a hospital population. Nutr Hosp. 2005; 20:38–45.11. Ueno T, Hirayama S, Ito M, Nishioka E, Fukushima Y, Satoh T, et al. Albumin concentrat ion determined by the modified bromocresol purple method is superior to that by the bromocresol green method for assessing nutritional status in malnourished patients with inflammation. Ann Clin Biochem. 2013; 50(Pt 6):576–584. PMID: 23897106.12. Nakagomi A, Kohashi K, Morisawa T, Kosugi M, Endoh I, Kusama Y, et al. Nutritional status is associated with inf lammation and predicts a poor outcome in patients with chronic heart failure. J Atheroscler Thromb. 2016; 23:713–727. PMID: 26782970.13. Takagi K, Yagi T, Umeda Y, Shinoura S, Yoshida R, Nobuoka D, et al. Preoperative controlling nutritional status (CONUT) score for assessment of prognosis following hepatectomy for hepatocellular carcinoma. World J Surg. 2017; 41:2353–2360. PMID: 28389736.14. Iseki Y, Shibutani M, Maeda K, Nagahara H, Ohtani H, Sugano K, et al. Impact of the preoperative controlling nutritional status (CONUT) score on the survival after curative surgery for colorectal cancer. PLoS One. 2015; 10:e0132488. PMID: 26147805.15. Yoshida N, Harada K, Baba Y, Kosumi K, Iwatsuki M, Kinoshita K, et al. Preoperative controlling nutritional status (CONUT) is useful to estimate the prognosis after esophagectomy for esophageal cancer. Langenbecks Arch Surg. 2017; 402:333–341. PMID: 28138759.16. Lin JW, Cameron JL, Yeo CJ, Riall TS, Lillemoe KD. Risk Factors and Outcomes in Postpancreaticoduodenectomy Pancreaticocutaneous Fistula. J Gastrointest Surg. 2004; 8:951–959. PMID: 15585382.17. Hashimoto Y, Sclabas GM, Takahashi N, Kirihara Y, Smyrk TC, Huebner M, et al. Dual-phase computed tomography for assessment of pancreatic fibrosis and anastomotic failure risk following pancreatoduodenectomy. J Gastrointest Surg. 2011; 15:2193–2204. PMID: 21948179.18. Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, et al. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005; 138:8–13. PMID: 16003309.19. Pratt WB, Callery MP, Vollmer CM Jr. The latent presentation of pancreatic fistulas. Br J Surg. 2009; 96:641–649. PMID: 19434658.20. Fu SJ, Shen SL, Li SQ, Hu WJ, Hua YP, Kuang M, et al. Risk factors and outcomes of postoperative pancreatic fistula after pancreatico-duodenectomy: an audit of 532 consecutive cases. BMC Surg. 2015; 15:34. PMID: 25887526.21. Callery MP, Pratt WB, Kent TS, Chaikof EL, Vollmer CM Jr. A Prospectively Validated Clinical Risk Score Accurately Predicts Pancreatic Fistula After Pancreatoduodenectomy. J Am Coll Surg. 2013; 216:1–14. PMID: 23122535.22. Afaneh C, Gerszberg D, Slattery E, Seres DS, Chabot JA, Kluger MD. Pancreatic cancer surgery and nutrition management: a review of the current literature. Hepatobiliary Surg Nutr. 2015; 4:59–71. PMID: 25713805.23. Arezzo di Trifiletti A, Misino P, Giannantoni P, Giannantoni B, Cascino A, Fazi L, et al. Comparison of the performance of four different tools in diagnosing disease-associated anorexia and their relationship with nutritional, functional and clinical outcome measures in hospitalized patients. Clin Nutr. 2013; 32:527–532. PMID: 23218121.24. Kim JH, Lee H, Choi HH, Min SK, Lee HK. Nutritional risk factors are associated with postoperative complications after pancreaticoduodenectomy. Ann Surg Treat Res. 2019; 96:201–207. PMID: 30941324.25. Fukuda Y, Yamamoto K, Hirao M, Nishikawa K, Maeda S, Haraguchi N, et al. Prevalence of malnutrition among gastric cancer patients undergoing gastrectomy and optimal preoperative nutritional support for preventing surgical site infections. Ann Surg Oncol. 2015; 22 Suppl 3:S778–S785. PMID: 26286199.26. Aida T, Furukawa K, Suzuki D, Shimizu H, Yoshidome H, Ohtsuka M, et al. Preoperative Immunonutrition Decreases Postoperative Complications by Modulating Prostaglandin E2 Production and T-cell Differentiation in Patients Undergoing Pancreatoduodenectomy. Surgery. 2014; 155:124–133. PMID: 24589090.27. Hughes MJ, McNally S, Wigmore SJ. Enhanced recovery following liver surgery: a systematic review and metaanalysis. HPB (Oxford). 2014; 16:699–706. PMID: 24661306.28. Kehlet H, Wilmore DW. Evidence-based surgical care and the evolution of fast-track surgery. Ann Surg. 2008; 248:189–198. PMID: 18650627.29. Hu BY, Wan T, Zhang WZ, Dong JH. Risk factors for postoperative pancreatic fistula: Analysis of 539 successive cases of pancreaticoduodenectomy. World J Gastroenterol. 2016; 22:7797–7805. PMID: 27678363.30. Aoki S, Miyata H, Konno H, Gotoh M, Motoi F, Kumamaru H, et al. Risk factors of serious postoperative complications after pancreaticoduodenectomy and risk calculators for predicting postoperative complications: a nationwide study of 17,564 patients in Japan. J Hepatobiliary Pancreat Sci. 2017; 24:243–251. PMID: 28196308.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Predictive Values of Pretreatment Controlling Nutritional Status (CONUT) Score in Estimating Shortand Long-term Outcomes for Patients with Gastric Cancer Treated with Neoadjuvant Chemotherapy and Curative Gastrectomy
- Prognostic Significance of Preoperative Controlling Nutritional Status Score in Patients Who Underwent Hepatic Resection for Hepatocellular Carcinoma
- Factors Influencing the Pancreatic Leakage after Pancreaticoduodenectomy
- A model for predicting pancreatic leakage after pancreaticoduodenectomy based on the international study group of pancreatic surgery classification
- The Efficacy of the Prophylactic Use of Octreotide after a Pancreaticoduodenectomy