Acute Crit Care.
2020 May;35(2):87-92. 10.4266/acc.2019.00752.
Effects of the presence of a pediatric intensivist on treatment in the pediatric intensive care unit
- Affiliations
-
- 1Division of Pediatric Cardiology, Kyungpook National University Children’s Hospital and Department of Pediatrics, School of Medicine, Kyungpook National University, Daegu, Korea
- KMID: 2502338
- DOI: http://doi.org/10.4266/acc.2019.00752
Abstract
- Background
There are few studies on the effect of intensivist staffing in pediatric intensive care units (PICUs) in Korea. We aimed to evaluate the effect of pediatric intensivist staffing on treatment outcomes in a Korean hospital PICU.
Methods
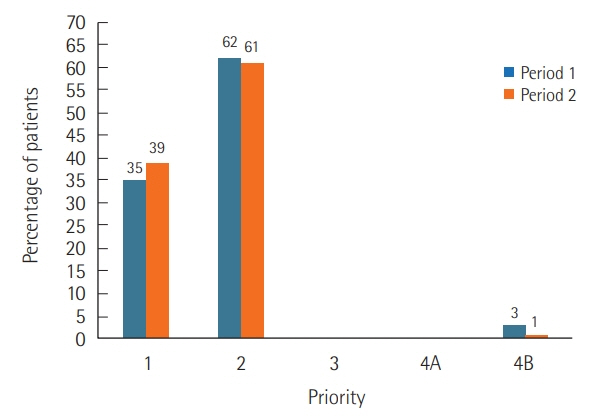
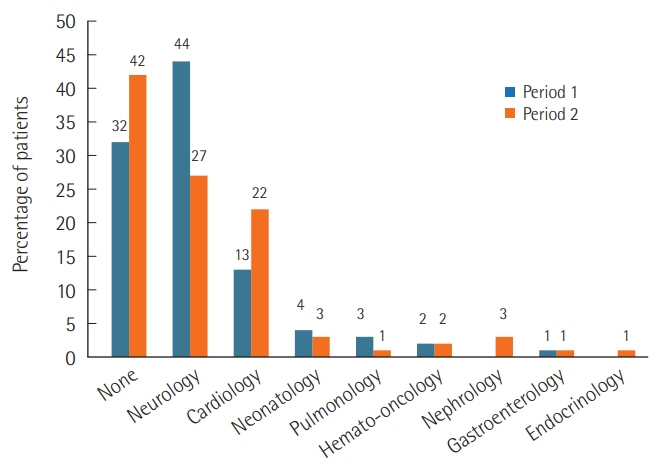
We analyzed two time periods according to pediatric intensivist staffing: period 1, between November 2015 to January 2017 (no intensivist staffing, n=97) and period 2, between February 2017 to February 2018 (intensivists staffing, n=135).
Results
Median age at admission was 5.4 years (range, 0.7–10.3 years) in period 1 and 3.6 years (0.2–5.1 years) in period 2 (P=0.013). The bed occupancy rate decreased in period 2 (75%; 73%–88%) compared to period 1 (89%; 81%–94%; P=0.015). However, the monthly bed turnover rate increased in period 2 (2.2%; 1.9%–2.7%) compared to period 1 (1.5%, 1.1%– 1.7%; P=0.005). In both periods, patients with chronic neurologic illness were the most common. Patients with cardiovascular problems were more prevalent in period 2 than period 1 (P=0.008). Daytime admission occurred more frequently in period 2 than period 1 (63% vs. 39%, P<0.001). The length of PICU stay, parameters related with mechanical ventilation and tracheostomy, and pediatric Sequential Organ Failure Assessment score were not different between periods. Sudden cardiopulmonary resuscitations occurred in two cases during period 1, but no case occurred during period 2.
Conclusions
Pediatric intensivist staffing in the PICU may affect efficient ICU operations.
Figure
Cited by 1 articles
-
Intensivists in the pediatric intensive care unit: conductors for better operational efficiency
June Dong Park
Acute Crit Care. 2020;35(2):115-116. doi: 10.4266/acc.2020.00276.
Reference
-
1. Pronovost PJ, Angus DC, Dorman T, Robinson KA, Dremsizov TT, Young TL. Physician staffing patterns and clinical outcomes in critically ill patients: a systematic review. JAMA. 2002; 288:2151–62.2. Wilcox ME, Chong CA, Niven DJ, Rubenfeld GD, Rowan KM, Wunsch H, et al. Do intensivist staffing patterns influence hospital mortality following ICU admission? A systematic review and meta-analyses. Crit Care Med. 2013; 41:2253–74.
Article3. Milstein A, Galvin RS, Delbanco SF, Salber P, Buck CR Jr. Improving the safety of health care: the leapfrog initiative. Eff Clin Pract. 2000; 3:313–6.4. Gajic O, Afessa B. Physician staffing models and patient safety in the ICU. Chest. 2009; 135:1038–44.
Article5. Haupt MT, Bekes CE, Brilli RJ, Carl LC, Gray AW, Jastremski MS, et al. Guidelines on critical care services and personnel: recommendations based on a system of categorization of three levels of care. Crit Care Med. 2003; 31:2677–83.
Article6. Park S, Suh GY. Intensivist physician staffing in intensive care units. Korean J Crit Care Med. 2013; 28:1–9.
Article7. Goh AY, Lum LC, Abdel-Latif ME. Impact of 24 hour critical care physician staffing on case-mix adjusted mortality in paediatric intensive care. Lancet. 2001; 357:445–6.
Article8. Yoon JS, Jhang WK, Choi YH, Lee B, Kim YH, Cho HJ, et al. Current status of pediatric critical care in Korea: results of 2015 national survey. J Korean Med Sci. 2018; 33:e308.
Article9. Nates JL, Nunnally M, Kleinpell R, Blosser S, Goldner J, Birriel B, et al. ICU admission, discharge, and triage guidelines: a framework to enhance clinical operations, development of institutional policies, and further research. Crit Care Med. 2016; 44:1553–602.10. Matics TJ, Sanchez-Pinto LN. Adaptation and validation of a pediatric Sequential Organ Failure Assessment Score and Evaluation of the Sepsis-3 definitions in critically ill children. JAMA Pediatr. 2017; 171:e172352.
Article11. Tripathi CB, Kumar R, Sharma RC, Agarwal R. Assessment of performance of services in a tertiary care Neuropsychiatric Institute using Pabon Lasso Model. Asian J Med Sci. 2016; 7:69–74.
Article12. Manthous CA, Amoateng-Adjepong Y, al-Kharrat T, Jacob B, Alnuaimat HM, Chatila W, et al. Effects of a medical intensivist on patient care in a community teaching hospital. Mayo Clin Proc. 1997; 72:391–9.
Article13. Hanson CW 3rd, Deutschman CS, Anderson HL 3rd, Reilly PM, Behringer EC, Schwab CW, et al. Effects of an organized critical care service on outcomes and resource utilization: a cohort study. Crit Care Med. 1999; 27:270–4.14. Blunt MC, Burchett KR. Out-of-hours consultant cover and case-mix-adjusted mortality in intensive care. Lancet. 2000; 356:735–6.
Article15. Wise KR, Akopov VA, Williams BR Jr, Ido MS, Leeper KV Jr, Dressler DD. Hospitalists and intensivists in the medical ICU: a prospective observational study comparing mortality and length of stay between two staffing models. J Hosp Med. 2012; 7:183–9.
Article16. Wallace DJ, Angus DC, Barnato AE, Kramer AA, Kahn JM. Nighttime intensivist staffing and mortality among critically ill patients. N Engl J Med. 2012; 366:2093–101.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intensivist Physician Staffing in Intensive Care Units
- Critical emergency medicine and the resuscitative care unit
- The Impact of an Attending Intensivist on the Clinical Outcomes of Patients Admitted to the Cardiac Surgical Intensive Care Unit after Coronary Artery Bypass Grafting
- Impact of a surgical intensivist on the clinical outcomes of patients admitted to a surgical intensive care unit
- Tachycardia in Intensive Care Unit