J Educ Eval Health Prof.
2020;17:1. 10.3352/jeehp.2020.17.1.
Effects of virtual reality training on decreasing the rates of needlestick or sharp injury in new-coming medical and nursing interns in Taiwan
- Affiliations
-
- 1Department of Surgery, Taipei Veterans General Hospital, Taipei, Taiwan
- 2Division of Clinical Skills Training, Department of Medical Education, Taipei Veterans General Hospital, Taipei, Taiwan
- 3School of Medicine, National Yang-Ming University, Taipei, Taiwan
- 4Bali Psychiatric Center, Ministry of Health and Welfare, New Taipei City, Taiwan
- 5Office of Medical Education, University of New South Wales Australia, Sydney, Australia
- 6Taipei Veterans General Hospital, Taipei, Taiwan
- KMID: 2502187
- DOI: http://doi.org/10.3352/jeehp.2020.17.1
Abstract
- Purpose
Senior nursing and medical interns’ lack of familiarity and confidence with respect to practicing universal precaution for the prevention of occupational needlestick or sharp injuries may harm themselves. Trainees’ self-reported needlestick or sharp injury rate was known to be especially high during the first 2 months of internship in Taiwan. This prospective cohort study aimed to assess the effect of newly developed virtual reality (VR) game, which uses Gagne’s learning model to improve universal precaution for needlestick or sharp injury prevention and decrease the rates of needle stick or sharp injuries in new-coming medical and nursing interns in Taiwan.
Methods
From 2017 to 2019, the VR system was developed and applied in training of 59 new-coming nursing and 50 medical interns. Occupational needlestick or sharp injury prevention was sought to be achieved through a game of right and wrong choices for safe or unsafe universal precaution behaviors.
Results
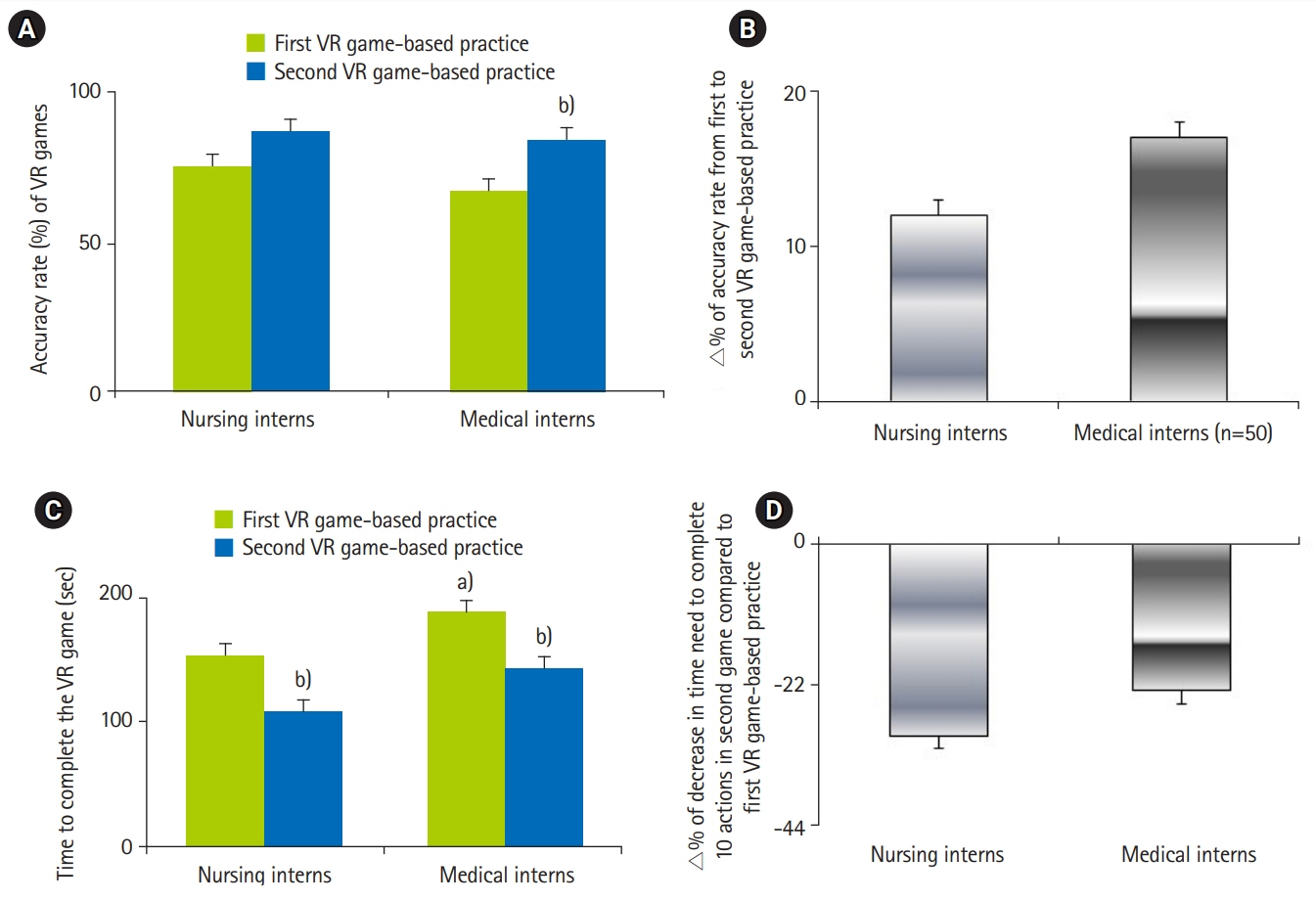
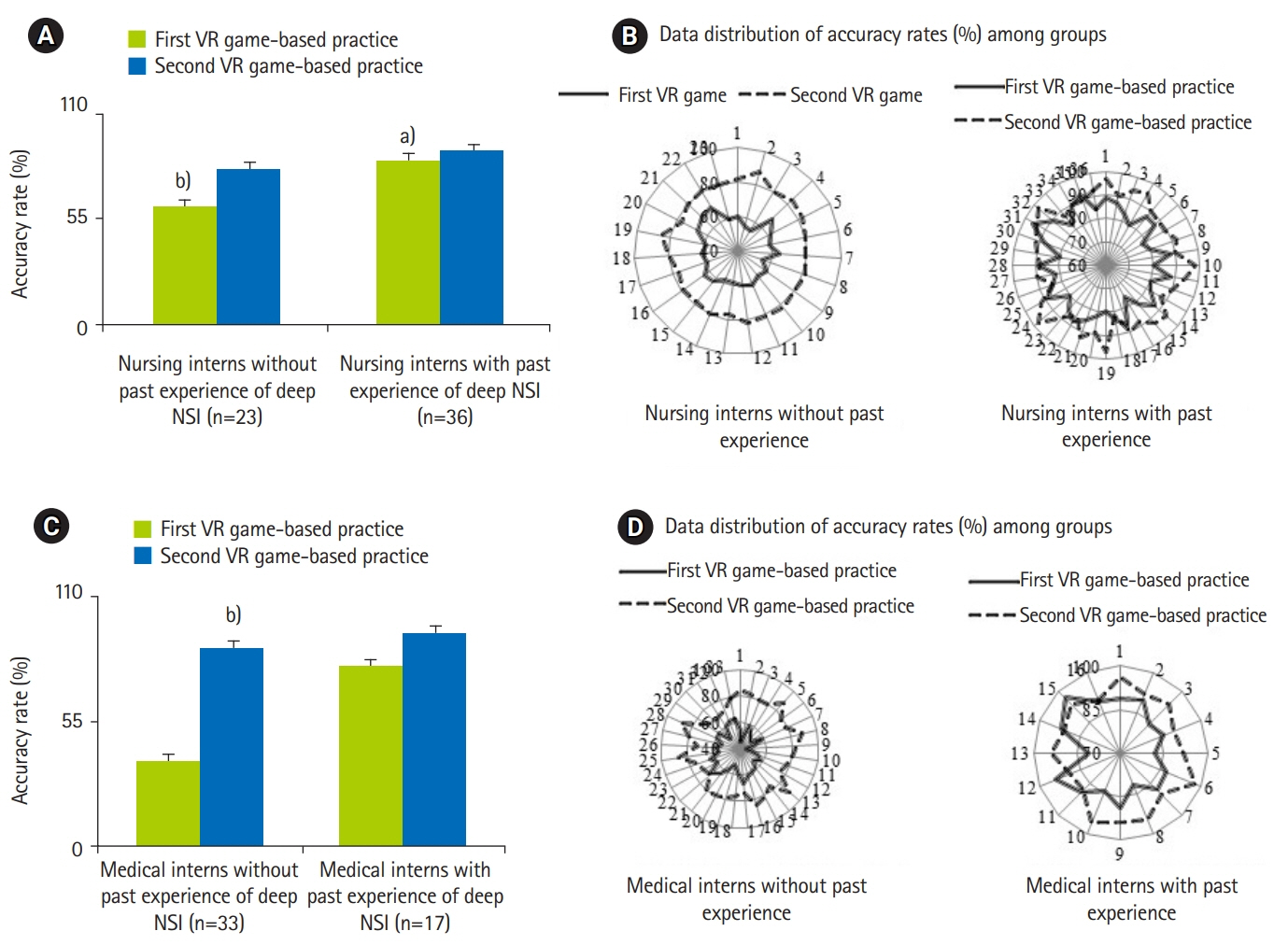
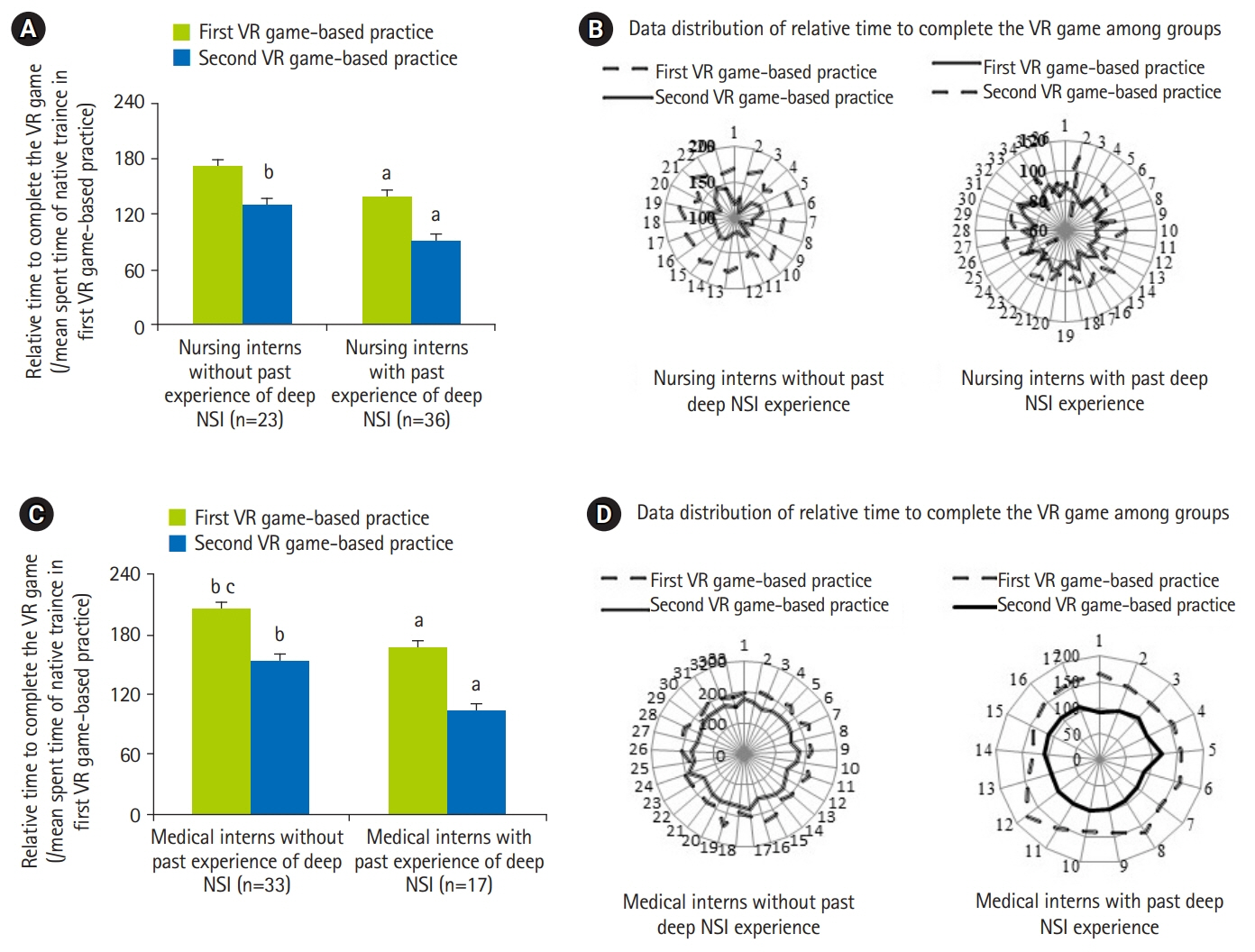
In comparison with medical interns, a higher proportion of nursing interns had past experiences of deep occupational needlestick or sharp injury. Before VR training, the familiarity and confidence for needlestick or sharp injury prevention were higher among nursing interns than medical interns. Trainees with past experiences of deep needlestick or sharp injury exhibited better performance on the accuracy rate and time needed to complete 20 decisions than those without past experiences in VR practice. All trainees showed an improved performance after VR training. A high proportion of trainees reported that the VR-based training significantly decreased their anxiety about needlestick or sharp injury prevention.
Conclusion
This self-developed VR game system using Gagne’s flow improved universal precaution for needlestick or sharp injury prevention and reduced the needlestick or sharp injury rates in the first 2 months of nursing and medical internship.
Keyword
Figure
Cited by 2 articles
-
How to train health personnel to protect themselves from SARS-CoV-2 (novel coronavirus) infection when caring for a patient or suspected case
Sun Huh, A Ra Cho
J Educ Eval Health Prof. 2020;17:10. doi: 10.3352/jeehp.2020.17.10.No difference in learning outcomes and usability between using controllers and hand tracking during a virtual reality endotracheal intubation training for medical students in Thailand
Chaowanan Khundam, Naparat Sukkriang, Frédéric Noël, Sun Huh
J Educ Eval Health Prof. 2021;18:22. doi: 10.3352/jeehp.2021.18.22.
Reference
-
References
1. Ghasemzadeh I, Kazerooni M, Davoodian P, Hamedi Y, Sadeghi P. Sharp injuries among medical students. Glob J Health Sci. 2015; 7:320–325. https://doi.org/10.5539/gjhs.v7n5p320.
Article2. Sharma R, Rasania S, Verma A, Singh S. Study of prevalence and response to needle stick injuries among health care workers in a tertiary care hospital in Delhi, India. Indian J Community Med. 2010; 35:74–77. https://doi.org/10.4103/0970-0218.62565.
Article3. Markovic-Denic LN, Mihajlovic B, Cemerlic-Adjic N, Pavlovic K, Nicin S. The effect of training program to reduce needlestick injuries. BMC Proc. 2011; 5(Suppl 6):P217. https://doi.org/10.1186/1753-6561-5-S6-P217.
Article4. Gao X, Hu B, Suo Y, Lu Q, Chen B, Hou T, Qin J, Huang W, Zong Z. A large-scale survey on sharp injuries among hospital-based healthcare workers in China. Sci Rep. 2017; 7:42620. https://doi.org/10.1038/srep42620.
Article5. Padilha JM, Machado PP, Ribeiro A, Ramos J, Costa P. Clinical virtual simulation in nursing education: randomized controlled trial. J Med Internet Res. 2019; 21:e11529. https://doi.org/10.2196/11529.
Article6. Makransky G, Bonde MT, Wulff JS, Wandall J, Hood M, Creed PA, Bache I, Silahtaroglu A, Norremolle A. Simulation based virtual learning environment in medical genetics counseling: an example of bridging the gap between theory and practice in medical education. BMC Med Educ. 2016; 16:98. https://doi.org/10.1186/s12909-016-0620-6.
Article7. Gentry SV, Gauthier A, L’Estrade Ehrstrom B, Wortley D, Lilienthal A, Tudor Car L, Dauwels-Okutsu S, Nikolaou CK, Zary N, Campbell J, Car J. Serious gaming and gamification education in health professions: systematic review. J Med Internet Res. 2019; 21:e12994. https://doi.org/10.2196/12994.
Article8. Buscombe C. Using Gagne’s theory to teach procedural skills. Clin Teach. 2013; 10:302–307. https://doi.org/10.1111/tct.12051.
Article9. Yasin J, Fisseha R, Mekonnen F, Yirdaw K. Occupational exposure to blood and body fluids and associated factors among health care workers at the University of Gondar Hospital, Northwest Ethiopia. Environ Health Prev Med. 2019; 24:18. https://doi.org/10.1186/s12199-019-0769-9.
Article10. Seng M, Lim JW, Sng J, Kong WY, Koh D. Incidence of needlestick injuries among medical students after implementation of preventive training. Singapore Med J. 2013; 54:496–500. https://doi.org/10.11622/smedj.2013171.
Article11. Taylor DC, Hamdy H. Adult learning theories: implications for learning and teaching in medical education: AMEE guide no. 83. Med Teach. 2013; 35:e1561–e1572. https://doi.org/10.3109/0142159X.2013.828153.
Article12. Lakbala P, Sobhani G, Lakbala M, Inaloo KD, Mahmoodi H. Sharps injuries in the operating room. Environ Health Prev Med. 2014; 19:348–353. https://doi.org/10.1007/s12199-014-0401-y.
Article13. Kinlin LM, Mittleman MA, Harris AD, Rubin MA, Fisman DN. Use of gloves and reduction of risk of injury caused by needles or sharp medical devices in healthcare workers: results from a case-crossover study. Infect Control Hosp Epidemiol. 2010; 31:908–917. https://doi.org/10.1086/655839.
Article14. Kaweti G, Abegaz T. Prevalence of percutaneous injuries and associated factors among health care workers in Hawassa referral and adare District hospitals, Hawassa, Ethiopia, January 2014. BMC Public Health. 2016; 16:8. https://doi.org/10.1186/s12889-015-2642-0.
Article15. Naghavi SH, Shabestari O, Alcolado J. Post-traumatic stress disorder in trainee doctors with previous needlestick injuries. Occup Med. 2013; 63:260–265. https://doi.org/10.1093/occmed/kqt027.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The digital literacy, awareness, and educational needs of virtual reality among nursing students
- Virtual Reality Technology Trends in Aeromedical Field
- Clinical application of virtual reality for vestibular rehabilitation
- The effects of maternal-child nursing clinical practicum using virtual reality on nursing students’ competencies: a systematic review
- Effects of a Virtual Reality Simulation and a Blended Simulation of Care for Pediatric Patient with Asthma