J Educ Eval Health Prof.
2019;16:31. 10.3352/jeehp.2019.16.31.
Application of an objective structured clinical examination to evaluate and monitor interns’ proficiency in hand hygiene and personal protective equipment use in the United States
- Affiliations
-
- 1Division of General Internal Medicine, Department of Medicine, University of Florida, Gainesville, FL, USA
- 2College of Medicine Educational Affairs, University of Florida, Gainesville, FL, USA
- 3Graudate of Medical Education, College of Medicine, University of Florida, Gainesville, FL, USA
- 4Division of Infectious Diseases, Department of Medicine, University of Florida, Gainesville, FL, USA
- 5Division of Hematology and Oncology, Department of Medicine, University of Florida, Gainesville, FL, USA
- 6Department of Neurosurgery, University of Florida, Gainesville, FL, USA
- KMID: 2502168
- DOI: http://doi.org/10.3352/jeehp.2019.16.31
Abstract
- Purpose
This study was conducted to determine whether an objective structured clinical examination (OSCE) could be used to evaluate and monitor hand hygiene and personal protective equipment (PPE) proficiency among medical interns in the United States.
Methods
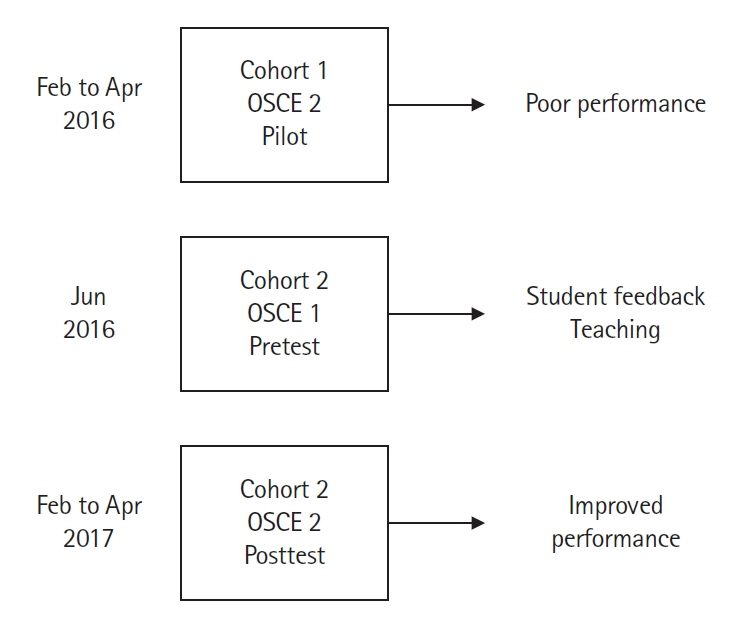
Interns in July 2015 (N=123, cohort 1) with no experience of OSCE-based contact precaution evaluation and teaching were evaluated in early 2016 using an OSCE for hand hygiene and PPE proficiency. They performed poorly. Therefore, the new interns entering in July 2016 (N=151, cohort 2) were immediately tested at the same OSCE stations as cohort 1, and were provided with feedback and teaching. Cohort 2 was then retested at the OSCE station in early 2017. The Mann-Whitney U-test was used to compare the performance of cohort 1 and cohort 2 on checklist items. In cohort 2, performance differences between the beginning and end of the intern year were compared using the McNemar chi-square test for paired nominal data.
Results
Checklist items were scored, summed, and reported as percent correct. In cohort 2, the mean percent correct was higher on the posttest than on the pretest (92% vs. 77%, P<0.0001), and the passing rate (100% correct) was also significantly higher on the posttest (55% vs. 16%). At the end of intern year, the mean percent correct was higher in cohort 2 than in cohort 1 (95% vs. 90%, P<0.0001), and 55% of cohort 2 passed (a perfect score) compared to 24% in cohort 1 (P<0.0001).
Conclusion
An OSCE can be utilized to evaluate and monitor hand hygiene and PPE proficiency among interns in the United States.
Figure
Cited by 1 articles
-
Empirical analysis comparing the tele-objective structured clinical examination and the in-person assessment in Australia
Jonathan Zachary Felthun, Silas Taylor, Boaz Shulruf, Digby Wigram Allen, Sun Huh
J Educ Eval Health Prof. 2021;18:23. doi: 10.3352/jeehp.2021.18.23.
Reference
-
References
1. Simmons BP, Larson EL. Multiple drug resistant organisms in healthcare: the failure of contact precautions. J Infect Prev. 2015; 16:178–181. https://doi.org/10.1177/1757177415570104.
Article2. Cohen SH, Gerding DN, Johnson S, Kelly CP, Loo VG, McDonald LC, Pepin J. Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by the society for healthcare epidemiology of America (SHEA) and the infectious diseases society of America (IDSA). Infect Control Hosp Epidemiol. 2010; 31:431–455. https://doi.org/10.1086/651706.
Article3. Oughton MT, Loo VG, Dendukuri N, Fenn S, Libman MD. Hand hygiene with soap and water is superior to alcohol rub and antiseptic wipes for removal of Clostridium difficile. Infect Control Hosp Epidemiol. 2009; 30:939–944. https://doi.org/10.1086/605322.
Article4. Dhar S, Marchaim D, Tansek R, Chopra T, Yousuf A, Bhargava A, Martin ET, Talbot TR, Johnson LE, Hingwe A, Zuckerman JM, Bono BR, Shuman EK, Poblete J, Tran M, Kulhanek G, Thyagarajan R, Nagappan V, Herzke C, Perl TM, Kaye KS. Contact precautions: more is not necessarily better. Infect Control Hosp Epidemiol. 2014; 35:213–221. https://doi.org/10.1086/675294.
Article5. Stalvey C, Close J, Markham MJ, Meyer L, Nagoshi Y, Cooper LA. The Intern Handover: the gap between expectations and performance. Med Sci Educ. 2016; 26:771–776. https://doi.org/10.1007/s40670-016-0312-1.
Article6. United States Centers for Diseases Control. Sequence for donning and removing personal protective equipment [Internet]. Washington (DC): United States Centers for Diseases Control;2016. [cited 2019 Jul 19]. Available from: https://www.cdc.gov/hai/pdfs/ppe/ppe-sequence.pdf.7. Tomas ME, Kundrapu S, Thota P, Sunkesula VC, Cadnum JL, Mana TS, Jencson A, O’Donnell M, Zabarsky TF, Hecker MT, Ray AJ, Wilson BM, Donskey CJ. Contamination of health care personnel during removal of personal protective equipment. JAMA Intern Med. 2015; 175:1904–1910. https://doi.org/10.1001/jamainternmed.2015.4535.
Article8. Landelle C, Verachten M, Legrand P, Girou E, Barbut F, Brun-Buisson C. Contamination of healthcare workers’ hands with Clostridium difficile spores after caring for patients with C. difficile infection. Infect Control Hosp Epidemiol. 2014; 35:10–15. https://doi.org/10.1086/674396.
Article9. Midturi JK, Narasimhan A, Barnett T, Sodek J, Schreier W, Barnett J, Wheeler C, Barton L, Stock EM, Arroliga AC. A successful multifaceted strategy to improve hand hygiene compliance rates. Am J Infect Control. 2015; 43:533–536. https://doi.org/10.1016/j.ajic.2015.01.024.
Article10. John A, Tomas ME, Hari A, Wilson BM, Donskey CJ. Do medical students receive training in correct use of personal protective equipment? Med Educ Online. 2017; 22:1264125. https://doi.org/10.1080/10872981.2017.1264125.
Article11. John A, Tomas ME, Cadnum JL, Mana TS, Jencson A, Shaikh A, Zabarsky TF, Wilson BM, Donskey CJ. Are health care personnel trained in correct use of personal protective equipment? Am J Infect Control 2016;44:840-842. Am J Infect Control. 2016; 44:840–842. https://doi.org/10.1016/j.ajic.2016.03.031.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Can incoming United States pediatric interns be entrusted with the essential communication skills of informed consent?
- Awareness of occupational hazards and personal protective equipment use among dental hygienists
- Status and Strategies for Safety Management of Antineoplastic Drugs among Oncology Nurses
- Current status of occupational radiation exposure and protection among medical interns and residents
- Emergency Department Workers' Perceptions of Effectiveness and Reported Compliance of Infection Control Measures after Middle East Respiratory Syndrome Outbreaks