Intest Res.
2020 Jan;18(1):11-17. 10.5217/ir.2019.09144.
Pediatric to adult inflammatory bowel disease transition: the Asian experience
- Affiliations
-
- 1Division of Gastroenterology and Hepatology, National University Hospital, Singapore
- KMID: 2501363
- DOI: http://doi.org/10.5217/ir.2019.09144
Abstract
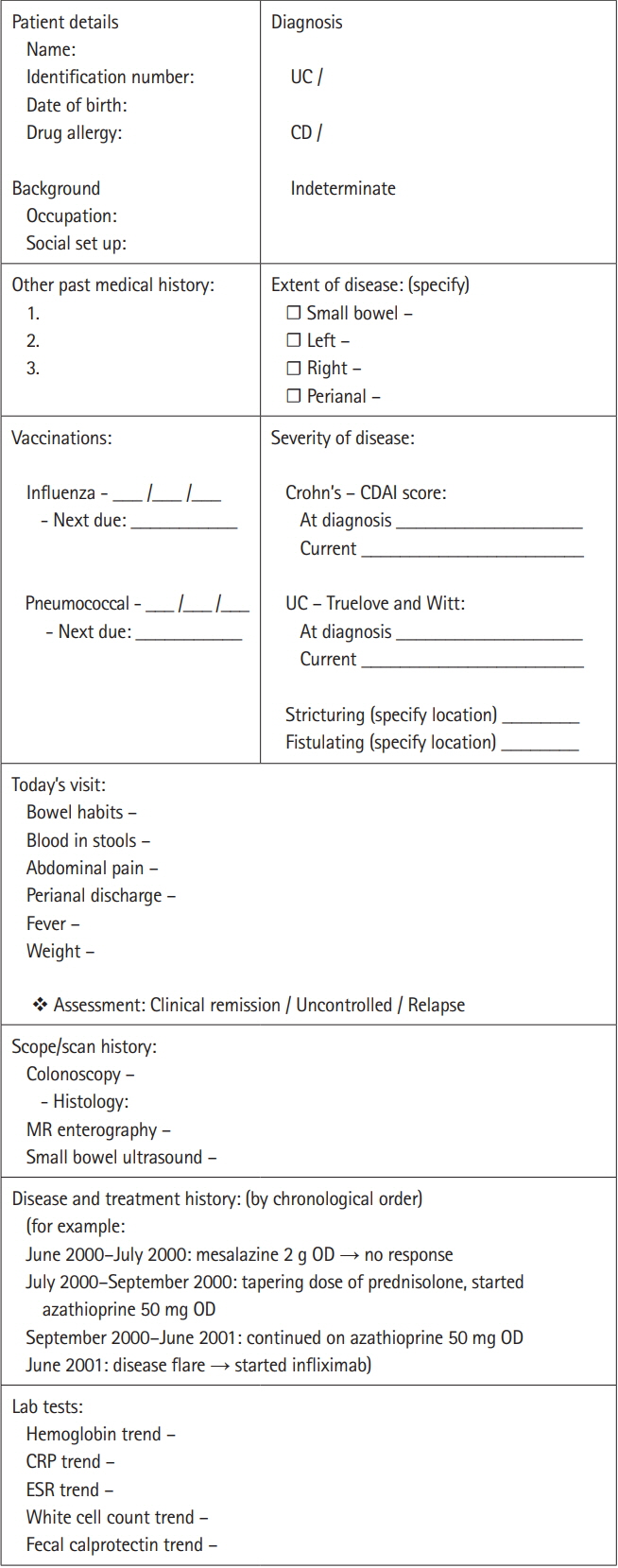
- Many tertiary inflammatory bowel disease (IBD) centers recognize that a structured transition program is fundamental for an IBD unit. However, the path to ensuring a seamless transition for all stakeholders is often fraught with challenges. In this review, we go through current evidence, identify the requirementsof a successful transition program, and the barriers to seamless transfer. We also aim to shed light on differences in needs between the Western and Asian adolescent IBD populations. Majority of healthcare providers viewed having a structured transition program to be very important. The lack of a standard protocol led us to come up with a list of requirements ofa successful program. These include: multidisciplinary team meetings, alternating visits between the adultand pediatric clinics, proper documentation of records, and determining the ideal timing for transfer. The difficulties forthe Asian adolescent IBD population may be attributed to the reliance on parental support to make decisions regarding medicaltreatment. Lastly, there are various physician, patient and disease factors which are barriers to seamless transition. These includethe lack of proper documentation, and lack of patient self-efficacy. We also propose a standardized template for documentation of medical records for IBD patients.
Figure
Cited by 1 articles
-
How Can We Do Transition Successfully from Pediatric to Adult Clinics in Inflammatory Bowel Disease?
Mi Jin Kim, Sung Noh Hong, Young-Ho Kim, Yon Ho Choe
Korean J Gastroenterol. 2021;77(5):227-230. doi: 10.4166/kjg.2021.065.
Reference
-
1. Sawczenko A, Sandhu BK, Logan RF, et al. Prospective survey of childhood inflammatory bowel disease in the British Isles. Lancet. 2001; 357:1093–1094.
Article2. Lehtinen P, Ashorn M, Iltanen S, et al. Incidence trends of pediatric inflammatory bowel disease in Finland, 1987-2003, a nationwide study. Inflamm Bowel Dis. 2011; 17:1778–1783.
Article3. Goodhand J, Dawson R, Hefferon M, et al. Inflammatory bowel disease in young people: the case for transitional clinics. Inflamm Bowel Dis. 2010; 16:947–952.4. Blum RW, Garell D, Hodgman CH, et al. Transition from childcentered to adult health-care systems for adolescents with chronic conditions: a position paper of the Society for Adolescent Medicine. J Adolesc Health. 1993; 14:570–576.
Article5. Al-Jahdali E, Mosli M, Saadah O. A cross-sectional survey of Saudi gastroenterologists: transition strategies for adolescents with inflammatory bowel disease. Saudi J Gastroenterol. 2017; 23:233–237.6. Zijlstra M, De Bie C, Breij L, et al. Self-efficacy in adolescents with inflammatory bowel disease: a pilot study of the “IBDyourself”, a disease-specific questionnaire. J Crohns Colitis. 2013; 7:e375–e385.
Article7. Van Rheenen PF, Aloi M, Biron IA, et al. European Crohn’s and Colitis Organisation topical review on transitional care in inflammatory bowel disease. J Crohns Colitis. 2017; 11:1032–1038.
Article8. Leung Y, Heyman MB, Mahadevan U. Transitioning the adolescent inflammatory bowel disease patient: guidelines for the adult and pediatric gastroenterologist. Inflamm Bowel Dis. 2011; 17:2169–2173.
Article9. De Silva PS, Fishman LN. Transition of the patient with IBD from pediatric to adult care: an assessment of current evidence. Inflamm Bowel Dis. 2014; 20:1458–1464.
Article10. Nohara Y, Lee J. More adults kept from leaving parents’ nests in Asia by harsh economic realities. The Japantimes. https://www.japantimes.co.jp/news/2016/12/02/national/adults-kept-leaving-parents-nests-asia-harsh-economic-realities/#.11. Kumagai H, Kudo T, Uchida K, et al. Adult gastroenterologists’ views on transitional care: results from a survey. Pediatr Int. 2019; 61:817–822.
Article12. Huang JS, Tobin A, Tompane T. Clinicians poorly assess health literacy-related readiness for transition to adult care in adolescents with inflammatory bowel disease. Clin Gastroenterol Hepatol. 2012; 10:626–632.
Article13. Parker RM, Baker DW, Williams MV, Nurss JR. The test of functional health literacy in adults: a new instrument for measuring patients’ literacy skills. J Gen Intern Med. 1995; 10:537–541.14. Eaden JA, Abrams K, Mayberry JF. The Crohn’s and Colitis Knowledge Score: a test for measuring patient knowledge in inflammatory bowel disease. Am J Gastroenterol. 1999; 94:3560–3566.
Article15. Sawicki GS, Lukens-Bull K, Yin X, et al. Measuring the transition readiness of youth with special healthcare needs: validation of the TRAQ: Transition Readiness Assessment Questionnaire. J Pediatr Psychol. 2011; 36:160–171.
Article16. Gray WN, Resmini AR, Baker KD, et al. Concerns, barriers, and recommendations to improve transition from pediatric to adult IBD care: perspectives of patients, parents, and health professionals. Inflamm Bowel Dis. 2015; 21:1641–1651.
Article17. Kumagai H, Akiyama T, Abukawa D, et al. Guidelines for autonomy support of patients with IBD in the transitional period. Jpn J Pediatr Gastroenterol Hepatol Nutr. 2018; 32:15–27.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- How Can We Do Transition Successfully from Pediatric to Adult Clinics in Inflammatory Bowel Disease?
- Successful Transition from Pediatric to Adult Care in Inflammatory Bowel Disease: What is the Key?
- Successful transition from pediatric to adult care in inflammatory bowel disease: what is the key?
- Characteristics and Treatment Outcomes of Transition among Patients with Inflammatory Bowel Disease
- Inflammatory Bowel Disease in Pediatric Age