Quantified Self-Using Consumer Wearable Device: Predicting Physical and Mental Health
- Affiliations
-
- 1Computer Science Department, BINUS Graduate Program - Master of Computer Science Program, Bina Nusantara University, Jakarta,
- 2Bioinformatics and Data Science Research Center, Bina Nusantara University, Jakarta,
- 3Computer Science Department, School of Computer Science, Bina Nusantara University, Jakarta,
- KMID: 2501333
- DOI: http://doi.org/10.4258/hir.2020.26.2.83
Abstract
Objectives Recently, wearable device technology has gained more popularity in supporting a healthy lifestyle. Hence, researchers have begun to put significant efforts into studying the direct and indirect benefits of wearable devices for health and wellbeing. This paper summarizes recent studies on the use of consumer wearable devices to improve physical activity, mental health, and health consciousness.
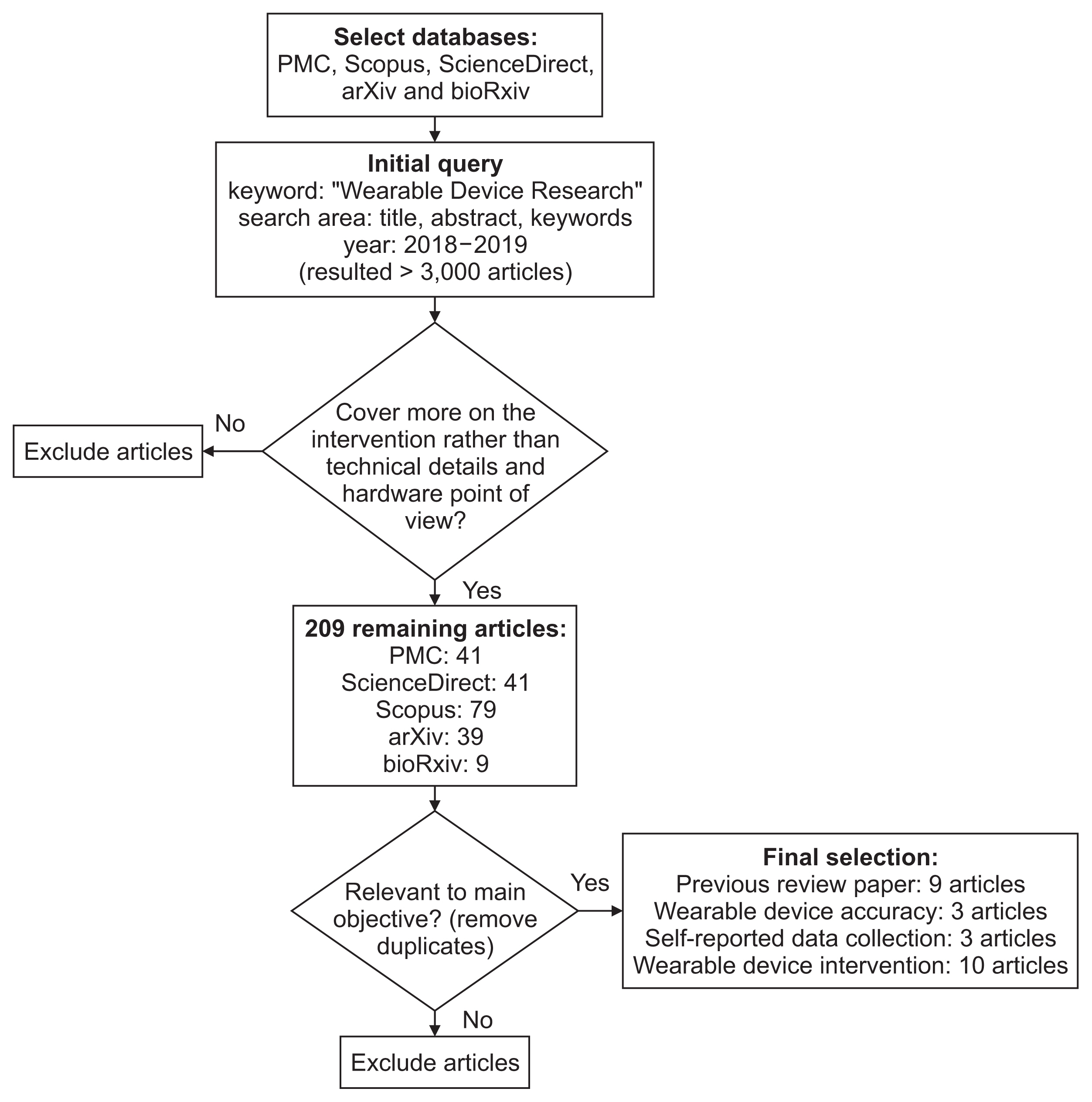
Methods A thorough literature search was performed from several reputable databases, such as PubMed, Scopus, ScienceDirect, arXiv, and bioRxiv mainly using “wearable device research” as a keyword, no earlier than 2018. As a result, 25 of the most recent and relevant papers included in this review cover several topics, such as previous literature reviews (9 papers), wearable device accuracy (3 papers), self-reported data collection tools (3 papers), and wearable device intervention (10 papers).
Results All the chosen studies are discussed based on the wearable device used, complementary data, study design, and data processing method. All these previous studies indicate that wearable devices are used either to validate their benefits for general wellbeing or for more serious medical contexts, such as cardiovascular disorders and post-stroke treatment.
Conclusions Despite their huge potential for adoption in clinical settings, wearable device accuracy and validity remain the key challenge to be met. Some lessons learned and future projections, such as combining traditional study design with statistical and machine learning methods, are highlighted in this paper to provide a useful overview for other researchers carrying out similar research.
Figure
Reference
-
References
1. IDC. IDC reports strong growth in the worldwide wearables market, led by holiday shipments of smartwatches, wrist bands, and ear-worn devices [Internet]. Framingham (MA): IDC Corporate;2019. [cited at 2020 Apr 15]. Available from: https://www.idc.com/getdoc.jsp?containerId=prUS44901819.2. Wolf G, Kelly K. What is Quantified Self? [Internet]. [place unknown]: Quantified Self;2019. [cited at 2020 Apr 15]. Available from: https://quantifiedself.com/about/what-is-quantified-self/.3. Swan M. The Quantified Self: fundamental disruption in big data science and biological discovery. Big Data. 2013; 1(2):85–99.
Article4. Prince JD. The Quantified Self: operationalizing the quotidien. J Electron Resour Med Libr. 2014; 11(2):91–9.
Article5. Strath SJ, Rowley TW. Wearables for promoting physical activity. Clin Chem. 2018; 64(1):53–63.
Article6. Brickwood KJ, Watson G, O’Brien J, Williams AD. Consumer-based wearable activity trackers increase physical activity participation: systematic review and meta-analysis. JMIR Mhealth Uhealth. 2019; 7(4):e11819.
Article7. Bohm B, Karwiese SD, Bohm H, Oberhoffer R. Effects of mobile health including wearable activity trackers to increase physical activity outcomes among healthy children and adolescents: systematic review. JMIR Mhealth Uhealth. 2019; 7(4):e8298.
Article8. Aroganam G, Manivannan N, Harrison D. Review on wearable technology sensors used in consumer sport applications. Sensors (Basel). 2019; 19(9):1983.
Article9. Khakurel J, Melkas H, Porras J. Tapping into the wearable device revolution in the work environment: a systematic review. Inf Technol People. 2018; 31(3):791–818.
Article10. Taj-Eldin M, Ryan C, O’Flynn B, Galvin P. A review of wearable solutions for physiological and emotional monitoring for use by people with autism spectrum disorder and their caregivers. Sensors (Basel). 2018; 18(12):4271.
Article11. Johansson D, Malmgren K, Alt Murphy M. Wearable sensors for clinical applications in epilepsy, Parkinson’s disease, and stroke: a mixed-methods systematic review. J Neurol. 2018; 265(8):1740–52.
Article12. Feehan LM, Geldman J, Sayre EC, Park C, Ezzat AM, Yoo JY, et al. Accuracy of Fitbit devices: systematic review and narrative syntheses of quantitative data. JMIR Mhealth Uhealth. 2018; 6(8):e10527.
Article13. Farrahi V, Niemela M, Kangas M, Korpelainen R, Jamsa T. Calibration and validation of accelerometer-based activity monitors: a systematic review of machine-learning approaches. Gait Posture. 2019; 68:285–99.
Article14. Bloss R. Wearable sensors bring new benefits to continuous medical monitoring, real time physical activity assessment, baby monitoring and industrial applications. Sens Rev. 2015; 35(2):141–5.
Article15. Nelson BW, Allen NB. Accuracy of consumer wearable heart rate measurement during an ecologically valid 24-hour period: intraindividual validation study. JMIR Mhealth Uhealth. 2019; 7(3):e10828.
Article16. Witte AK, Blankenhagel KJ, Korbel JJ, Zarnekow R. How accurate is accurate enough? An evaluation of commercial fitness trackers for individual health management. In : Proceedings of the Americas Conference on Information Systems (AMCIS2019); 2019 Aug 15–17; Cancun, Mexico.17. Kwon SB, Ahn JW, Lee SM, Lee J, Lee D, Hong J, et al. Estimating maximal oxygen uptake from daily activity data measured by a watch-type fitness tracker: cross-sectional study. JMIR Mhealth Uhealth. 2019; 7(6):e13327.
Article18. Dutta-Bergman MJ. Primary sources of health information: comparisons in the domain of health attitudes, health cognitions, and health behaviors. Health Commun. 2004; 16(3):273–88.
Article19. Holzinger A, Dorner S, Fodinger M, Valdez AC, Ziefle M. Chances of increasing youth health awareness through mobile wellness applications. Leitner G, Hitz M, Holzinger A, editors. HCI in work and learning, life and leisure. Heidelberg: Springer;2010. p. 71–81.
Article20. Grifantini K. How’s my sleep?: personal sleep trackers are gaining in popularity, but their accuracy is still open to debate. IEEE Pulse. 2014; 5(5):14–8.
Article21. Etkin J. The hidden cost of personal quantification. Journal of Consumer Research. 2016; 42(6):967–84.
Article22. Jang IY, Kim HR, Lee E, Jung HW, Park H, Cheon SH, et al. Impact of a wearable device-based walking programs in rural older adults on physical activity and health outcomes: cohort study. JMIR Mhealth Uhealth. 2018; 6(11):e11335.
Article23. Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003; 35(8):1381–95.
Article24. Rabin R, Gudex C, Selai C, Herdman M. From translation to version management: a history and review of methods for the cultural adaptation of the EuroQol five-dimensional questionnaire. Value Health. 2014; 17(1):70–6.
Article25. Butler J, Kern ML. The PERMA-Profiler: a brief multidimensional measure of flourishing. Intl J Wellbeing. 2016; 6(3):1–48.
Article26. Stiglbauer B, Weber S, Batinic B. Does your health really benefit from using a self-tracking device? Evidence from a longitudinal randomized control trial. Comput Human Behav. 2019; 94:131–9.
Article27. Sano A, Taylor S, McHill AW, Phillips AJ, Barger LK, Klerman E, et al. Identifying objective physiological markers and modifiable behaviors for self-reported stress and mental health status using wearable sensors and mobile phones: observational study. J Med Internet Res. 2018; 20(6):e210.
Article28. Horne JA, Ostberg O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int J Chronobiol. 1976; 4(2):97–110.29. Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989; 28(2):193–213.
Article30. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983; 24(4):385–96.
Article31. Ware J Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996; 34(3):220–33.32. John OP, Srivastava S. The Big Five trait taxonomy: history, measurement, and theoretical perspectives. Pervin LA, John OP, editors. Handbook of personality: theory and research. 2nd ed. New York (NY): The Guilford Press;1999. p. 102–38.33. Compagnat M, Batcho CS, David R, Vuillerme N, Salle JY, Daviet JC, et al. Validity of the walked distance estimated by wearable devices in stroke individuals. Sensors (Basel). 2019; 19(11):2497.
Article34. Cheong IY, An SY, Cha WC, Rha MY, Kim ST, Chang DK, et al. Efficacy of mobile health care application and wearable device in improvement of physical performance in colorectal cancer patients undergoing chemotherapy. Clin Colorectal Cancer. 2018; 17(2):e353–e362.
Article35. Lim WK, Davila S, Teo JX, Yang C, Pua CJ, Blocker C, et al. Beyond fitness tracking: the use of consumer-grade wearable data from normal volunteers in cardiovascular and lipidomics research. PLoS Biol. 2018; 16(2):e2004285.
Article36. Buchele Harris H, Chen W. Technology-enhanced classroom activity breaks impacting children’s physical activity and fitness. J Clin Med. 2018; 7(7):165.
Article37. Reddy RK, Pooni R, Zaharieva DP, Senf B, El Youssef J, Dassau E, et al. Accuracy of wrist-worn activity monitors during common daily physical activities and types of structured exercise: evaluation study. JMIR Mhealth Uhealth. 2018; 6(12):e10338.
Article38. Vandelanotte C, Duncan MJ, Maher CA, Schoeppe S, Rebar AL, Power DA, et al. The effectiveness of a web-based computer-tailored physical activity intervention using Fitbit activity trackers: randomized trial. J Med Internet Res. 2018; 20(12):e11321.
Article39. Jones D, Crossley K, Dascombe B, Hart HF, Kemp J. Validity and reliability of the Fitbit Flex and ActiGraph GT3X+ at jogging and running speeds. Int J Sports Phys Ther. 2018; 13(5):860–70.
Article40. Redenius N, Kim Y, Byun W. Concurrent validity of the Fitbit for assessing sedentary behavior and moderate-to-vigorous physical activity. BMC Med Res Methodol. 2019; 19(1):29.
Article41. Collins JE, Yang HY, Trentadue TP, Gong Y, Losina E. Validation of the Fitbit Charge 2 compared to the Acti-Graph GT3X+ in older adults with knee osteoarthritis in free-living conditions. PLoS One. 2019; 14(1):e0211231.
Article42. Ravi D, Wong C, Lo B, Yang GZ. A deep learning approach to on-node sensor data analytics for mobile or wearable devices. IEEE J Biomed Health Inform. 2017; 21(1):56–64.
Article43. Bai J, Sun Y, Schrack JA, Crainiceanu CM, Wang MC. A two-stage model for wearable device data. Biometrics. 2018; 74(2):744–52.
Article44. de Quadros T, Lazzaretti AE, Schneider FK. A movement decomposition and machine learning-based fall detection system using wrist wearable device. IEEE Sens J. 2018; 18(12):5082–9.
Article45. Shashikumar SP, Shah AJ, Li Q, Clifford GD, Nemati S. A deep learning approach to monitoring and detecting atrial fibrillation using wearable technology. In : Proceedings of 2017 IEEE EMBS International Conference on Biomedical & Health Informatics (BHI); 2017 Feb 16–19. Orlando, FL; p. 141–4.
Article46. Varatharajan R, Manogaran G, Priyan MK, Sundarasekar R. Wearable sensor devices for early detection of Alzheimer disease using dynamic time warping algorithm. Cluster Comput. 2018; 21(1):681–90.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Can Fitness Trackers Track Sleep?
- Machine Learning Models to Identify Individuals With Imminent Suicide Risk Using a Wearable Device: A Pilot Study
- The Effectiveness of a mHealth Program Using Wearable Devices and Health Coaching among Bus Drivers for Promoting Physical Activity
- An Update on the Use of Wearable Devices in Men’s Health
- Digital health care and arrhythmia: a case of WPW syndrome in South Korea, 2020