Ann Rehabil Med.
2020 Apr;44(2):165-170. 10.5535/arm.2020.44.2.165.
Precise Pulmonary Function Evaluation and Management of a Patient With Freeman-Sheldon Syndrome Associated With Recurrent Pneumonia and Chronic Respiratory Insufficiency
- Affiliations
-
- 1Department of Rehabilitation Medicine and Rehabilitation Institute of Neuromuscular Disease, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 2Pulmonary Rehabilitation Center, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2501061
- DOI: http://doi.org/10.5535/arm.2020.44.2.165
Abstract
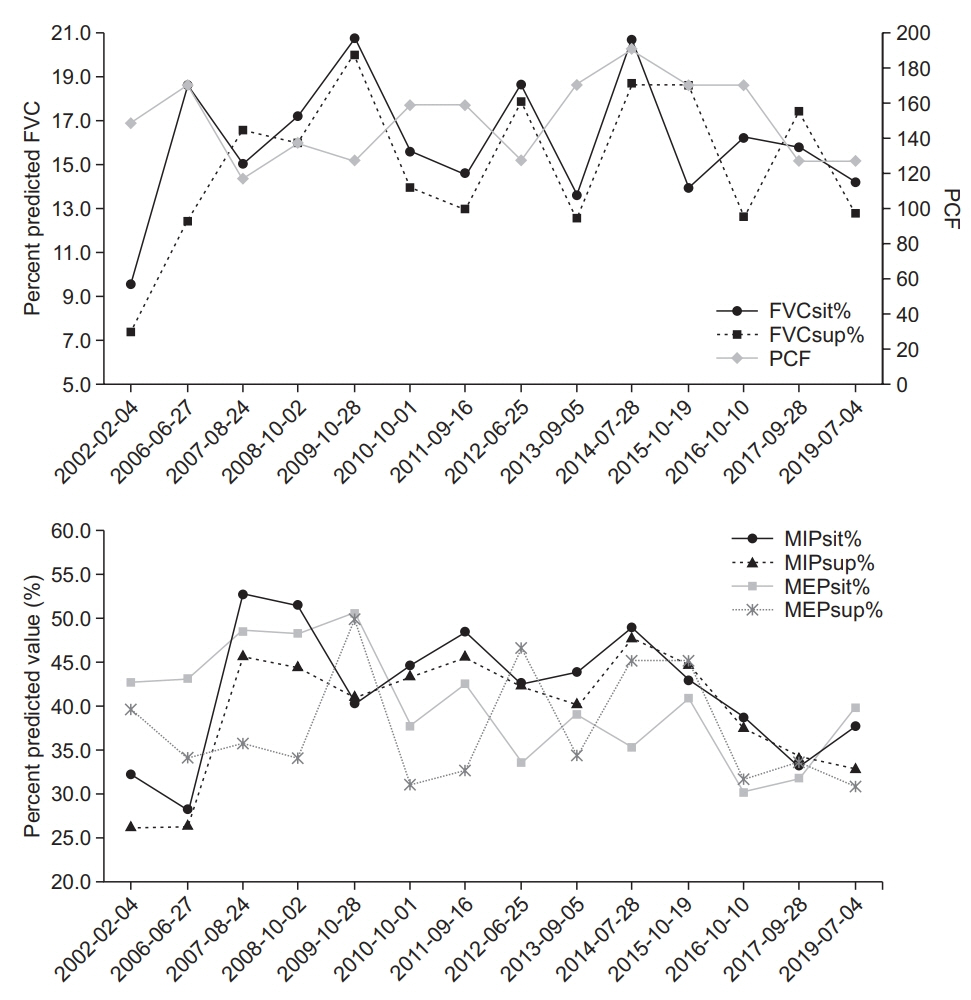
- Freeman-Sheldon syndrome (FSS) is a rare distal arthrogryposis syndrome. There are few reports on the respiratory insufficiency of FSS. Additionally, there is no detailed information on pulmonary functional evaluation. A 17-year-old male patient with FSS developed respiratory failure, leading him to be admitted to hospital several times for evaluation and treatment. Of those times he was admitted, two were due to pneumonia. His pulmonary functions were indicative of a restrictive lung disease potentially caused by severe scoliosis. After a non-invasive ventilatorwas applied correctly to the patient, pulmonary hypertension was normalized. His pulmonary function has been maintained for 13 years. Since receiving proper respiratory care, which includes assisted coughing methods, the patient has not developed pneumonia. It is important to properly evaluate the pulmonary function of patients who have FSS and scoliosis to eliminate the risk of long-term respiratory complications.
Figure
Cited by 2 articles
-
Letter: Precise Pulmonary Function Evaluation and Management of a Patient With Freeman-Sheldon Syndrome Associated With Recurrent Pneumonia and Chronic Respiratory Insufficiency (
Ann Rehabil Med 2020;44:165-70)
Mikaela I. Poling, Craig R. Dufresne
Ann Rehabil Med. 2020;44(5):409-410. doi: 10.5535/arm.20110.Response: Precise Pulmonary Function Evaluation and Management of a Patient With Freeman-Sheldon Syndrome Associated With Recurrent Pneumonia and Chronic Respiratory Insufficiency (
Ann Rehabil Med 2020;44:165-70)
Jihyun Park, Seong-Woong Kang, Won Ah Choi, Yewon Lee, Han Eol Cho
Ann Rehabil Med. 2020;44(5):411-413. doi: 10.5535/arm.20110.R.
Reference
-
1. Toydemir RM, Rutherford A, Whitby FG, Jorde LB, Carey JC, Bamshad MJ. Mutations in embryonic myosin heavy chain (MYH3) cause Freeman-Sheldon syndrome and Sheldon-Hall syndrome. Nat Genet. 2006; 38:561–5.
Article2. Attia A, Suleman M, Al aziz Al Nwasser A. Freeman–Sheldon syndrome with respiratory failure: a case report. Respir Med CME. 2008; 1:274–77.
Article3. Ferrari D, Bettuzzi C, Donzelli O. Freeman-Sheldon syndrome: a case report and review of the literature. Chir Organi Mov. 2008; 92:127–31.
Article4. Koumbourlis AC. Scoliosis and the respiratory system. Paediatr Respir Rev. 2006; 7:152–60.
Article5. Stevenson DA, Carey JC, Palumbos J, Rutherford A, Dolcourt J, Bamshad MJ. Clinical characteristics and natural history of Freeman-Sheldon syndrome. Pediatrics. 2006; 117:754–62.
Article6. Vanek J, Janda J, Amblerova V, Losan F. Freeman-Sheldon syndrome: a disorder of congenital myopathic origin? J Med Genet. 1986; 23:231–6.
Article7. Madi-Jebara S, El-Hajj C, Jawish D, Ayoub E, Kharrat K, Antakly MC. Anesthetic management of a patient with Freeman-Sheldon syndrome: case report. J Clin Anesth. 2007; 19:460–2.
Article8. Munro HM, Butler PJ, Washington EJ. FreemanSheldon (whistling face) syndrome: anaesthetic and airway management. Paediatr Anaesth. 1997; 7:345–8.
Article9. Miske LJ, Hickey EM, Kolb SM, Weiner DJ, Panitch HB. Use of the mechanical in-exsufflator in pediatric patients with neuromuscular disease and impaired cough. Chest. 2004; 125:1406–12.
Article10. Lee JW, Won YH, Kim DH, Choi WA, Bach JR, Kim DJ, et al. Pulmonary rehabilitation to decrease perioperative risks of spinal fusion for patients with neuromuscular scoliosis and low vital capacity. Eur J Phys Rehabil Med. 2016; 52:28–35.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Letter: Precise Pulmonary Function Evaluation and Management of a Patient With Freeman-Sheldon Syndrome Associated With Recurrent Pneumonia and Chronic Respiratory Insufficiency (Ann Rehabil Med 2020;44:165-70)
- Response: Precise Pulmonary Function Evaluation and Management of a Patient With Freeman-Sheldon Syndrome Associated With Recurrent Pneumonia and Chronic Respiratory Insufficiency (Ann Rehabil Med 2020;44:165-70)
- Freeman-Sheldon Syndrome: Report of Two Cases in a Family
- A Case of Freeman-Sheldon Syndrome
- A Case of Freeman-Sheldon Syndrome in Father and Son