Ann Rehabil Med.
2020 Apr;44(2):151-157. 10.5535/arm.2020.44.2.151.
Frequency of and Reasons for Unplanned Transfers From the Inpatient Rehabilitation Facility in a Tertiary Hospital
- Affiliations
-
- 1Department of Rehabilitation Medicine, Chungnam National University Hospital, Daejeon, Korea
- KMID: 2501059
- DOI: http://doi.org/10.5535/arm.2020.44.2.151
Abstract
Objective
To characterize the patients in the inpatient rehabilitation facility who were transferred to acute care facilities and identify the frequency of and reasons for the unplanned transfer.
Methods
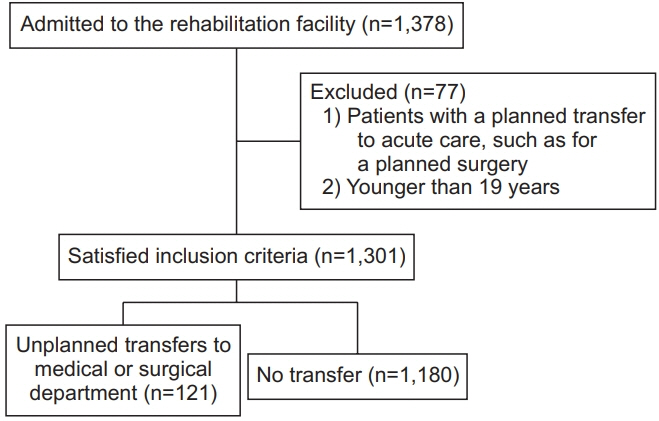
Medical records of patients admitted to the inpatient rehabilitation facility from October 2017 to December 2018 were reviewed. Patients were categorized according to their diagnoses. The included patients were divided into the unplanned transfer and control groups based on whether they required to transfer to another department for acute care before completing an uninterrupted rehabilitation course. The groups were compared in terms of sex, age, length of stay, admission sources, and disease groups. The reasons for unplanned transfers were classified based on medical or surgical conditions.
Results
Of the 1,378 patients were admitted to the inpatient rehabilitation facility, 1,301 satisfied inclusion criteria. Among them, 121 (9.3%) were unexpectedly transferred to the medical or surgical department. The unplanned transfer group had a higher age (69.54±12.53 vs. 64.39±15.32 years; p=0.001) and longer length of stay (85.69±66.08 vs. 37.81±31.13 days; p<0.001) than the control group. The top 3 reasons for unplanned transfers were infectious disease, cardiopulmonary disease, and orthopedic problem.
Conclusion
The unplanned transfer group had a significantly higher age and longer length of stay. The most common reason for the unplanned transfer was infectious disease. However, the proportions of those with orthopedic and neurological problems were relatively high. Therefore, further studies of these patient populations may help organize systematic strategies that are needed to reduce unplanned transfers to acute facilities for patients in rehabilitation facilities.
Figure
Reference
-
1. Stucki G, Reinhardt JD, Grimby G. Organizing human functioning and rehabilitation research into distinct scientific fields. Part II: Conceptual descriptions and domains for research. J Rehabil Med. 2007; 39:299–307.2. Gutenbrunner C, Ward AB, Chamberlain MA. White book on physical and rehabilitation medicine in Europe. Eura Medicophys. 2006; 42:295–332.3. Johnston MV, Wood KD, Fiedler R. Characteristics of effective and efficient rehabilitation programs. Arch Phys Med Rehabil. 2003; 84:410–8.
Article4. Vonlanthen R, Slankamenac K, Breitenstein S, Puhan MA, Muller MK, Hahnloser D, et al. The impact of complications on costs of major surgical procedures: a cost analysis of 1200 patients. Ann Surg. 2011; 254:907–13.5. White AC, Joseph B, Perrotta BA, Grandfield J, Muraldihar N, O’Connor HH, et al. Unplanned transfers following admission to a long-term acute care hospital: a quality issue. Chron Respir Dis. 2011; 8:245–52.6. Tator CH, Duncan EG, Edmonds VE, Lapczak LI, Andrews DF. Complications and costs of management of acute spinal cord injury. Paraplegia. 1993; 31:700–14.
Article7. Civelek GM, Atalay A, Turhan N. Medical complications experienced by first-time ischemic stroke patients during inpatient, tertiary level stroke rehabilitation. J Phys Ther Sci. 2016; 28:382–91.
Article8. Pinto SM, Galang G. Venous thromboembolism as predictor of acute care hospital transfer and inpatient rehabilitation length of stay. Am J Phys Med Rehabil. 2017; 96:367–73.
Article9. Formisano R, Azicnuda E, Sefid MK, Zampolini M, Scarponi F, Avesani R. Early rehabilitation: benefits in patients with severe acquired brain injury. Neurol Sci. 2017; 38:181–4.
Article10. Soop M, Fryksmark U, Koster M, Haglund B. The incidence of adverse events in Swedish hospitals: a retrospective medical record review study. Int J Qual Health Care. 2009; 21:285–91.
Article11. Carney ML, Ullrich P, Esselman P. Early unplanned transfers from inpatient rehabilitation. Am J Phys Med Rehabil. 2006; 85:453–60.
Article12. Faulk CE, Cooper NR, Staneata JA, Bunch MP, Galang E, Fang X, et al. Rate of return to acute care hospital based on day and time of rehabilitation admission. PM R. 2013; 5:757–62.
Article13. Siegler EL, Stineman MG, Maislin G. Development of complications during rehabilitation. Arch Intern Med. 1994; 154:2185–90.
Article14. Hammond FM, Horn SD, Smout RJ, Beaulieu CL, Barrett RS, Ryser DK, et al. Readmission to an acute care hospital during inpatient rehabilitation for traumatic brain injury. Arch Phys Med Rehabil. 2015; 96(8 Suppl):S293–303. e1.
Article15. Alam E, Wilson RD, Vargo MM. Inpatient cancer rehabilitation: a retrospective comparison of transfer back to acute care between patients with neoplasm and other rehabilitation patients. Arch Phys Med Rehabil. 2008; 89:1284–9.
Article16. Leape LL, Brennan TA, Laird N, Lawthers AG, Localio AR, Barnes BA, et al. The nature of adverse events in hospitalized patients: results of the Harvard Medical Practice Study II. N Engl J Med. 1991; 324:377–84.17. Ingeman A, Andersen G, Hundborg HH, Svendsen ML, Johnsen SP. In-hospital medical complications, length of stay, and mortality among stroke unit patients. Stroke. 2011; 42:3214–8.
Article18. Holloway RG, Witter DM Jr, Lawton KB, Lipscomb J, Samsa G. Inpatient costs of specific cerebrovascular events at five academic medical centers. Neurology. 1996; 46:854–60.19. Jorgensen HS, Nakayama H, Raaschou HO, Olsen TS. Acute stroke care and rehabilitation: an analysis of the direct cost and its clinical and social determinants. Stroke. 1997; 28:1138–41.
Article20. Mamoli A, Censori B, Casto L, Sileo C, Cesana B, Camerlingo M. An analysis of the costs of ischemic stroke in an Italian stroke unit. Neurology. 1999; 53:112–6.
Article21. Kim JM, Park ES, Jeong JS, Kim KM, Kim JM, Oh HS, et al. Multicenter surveillance study for nosocomial infections in major hospitals in Korea. Am J Infect Control. 2000; 28:454–8.
Article22. Divo MJ, Martinez CH, Mannino DM. Ageing and the epidemiology of multimorbidity. Eur Respir J. 2014; 44:1055–68.
Article23. Be’ery-Lipperman M, Gefen A. Contribution of muscular weakness to osteoporosis: computational and animal models. Clin Biomech (Bristol, Avon). 2005; 20:984–97.
Article24. Jordan KM, Cooper C. Epidemiology of osteoporosis. Best Pract Res Clin Rheumatol. 2002; 16:795–806.
Article25. Davis P, Lay-Yee R, Briant R, Ali W, Scott A, Schug S. Adverse events in New Zealand public hospitals I: occurrence and impact. N Z Med J. 2002; 115:U271.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Launching of the accreditation system for rehabilitation facility in Korea
- Requests for Interhospital Transfer Received by An 1339 Emergency Medical Information Center
- Experience of Discharge from Rehabilitation Facility
- A coordination project for improvement of osteoporosis medication use among patients who sustained an osteoporotic fracture: The Israeli experience
- The Discharge Destination of Rehabilitation Inpatients in a Tertiary Hospital