Clin Endosc.
2020 Jan;53(1):97-100. 10.5946/ce.2019.032.
A Rare Fatal Bile Peritonitis after Malposition of Endoscopic Ultrasound-Guided 5-Fr Naso-Gallbladder Drainage
- Affiliations
-
- 1Department of Internal Medicine, SAM Anyang Hospital, Anyang, Korea
- KMID: 2500912
- DOI: http://doi.org/10.5946/ce.2019.032
Abstract
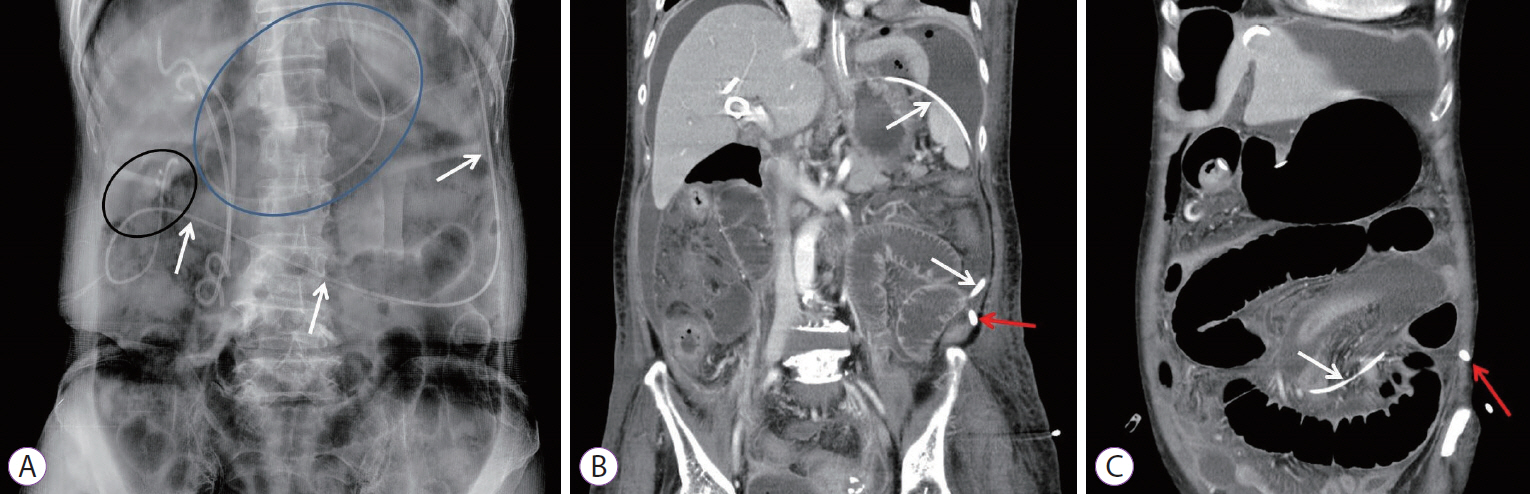
- Endoscopic ultrasound (EUS)-guided gallbladder (GB) drainage has recently emerged as a more feasible treatment than percutaneous transhepatic GB drainage for acute cholecystitis. In EUS-guided cholecystostomies in patients with distended GBs without pericholecystic inflammation or prominent wall thickening, a needle puncture with tract dilatation is often difficult. Guidewires may slip during the insertion of thin and flexible drainage catheters, which can also cause the body portion of the catheter to be unexpectedly situated and prolonged between the GB and intestines because the non-inflamed distended GB is fluctuant. Upon fluoroscopic examination during the procedure, the position of the abnormally coiled catheter may appear to be correct in patients with a distended stomach. We experienced such an adverse event with fatal bile peritonitis in a patient with GB distension suggestive of malignant bile duct stricture. Fatal bile peritonitis then occurred. Therefore, the endoscopist should confirm the indications for cholecystostomy and determine whether a distended GB is a secondary change or acute cholecystitis.
Figure
Reference
-
1. Saumoy M, Novikov A, Kahaleh M. Long-term outcomes after EUS-guided gallbladder drainage. Endosc Ultrasound. 2018; 7:97–101.2. Ahmed O, Rogers AC, Bolger JC, et al. Meta-analysis of outcomes of endoscopic ultrasound-guided gallbladder drainage versus percutaneous cholecystostomy for the management of acute cholecystitis. Surg Endosc. 2018; 32:1627–1635.
Article3. Tyberg A, Saumoy M, Sequeiros EV, et al. EUS-guided versus percutaneous gallbladder drainage: isn’t it time to convert? J Clin Gastroenterol. 2018; 52:79–84.4. Choi JH, Lee SS. Endoscopic ultrasonography-guided gallbladder drainage for acute cholecystitis: from evidence to practice. Dig Endosc. 2015; 27:1–7.
Article5. Ahmed O, Ogura T, Eldahrouty A, et al. Endoscopic ultrasound-guided gallbladder drainage: results of long-term follow-up. Saudi J Gastroenterol. 2018; 24:183–188.
Article6. Choi JH, Lee SS, Choi JH, et al. Long-term outcomes after endoscopic ultrasonography-guided gallbladder drainage for acute cholecystitis. Endoscopy. 2014; 46:656–661.
Article7. Jang JW, Lee SS, Park DH, Seo DW, Lee SK, Kim MH. Feasibility and safety of EUS-guided transgastric/transduodenal gallbladder drainage with single-step placement of a modified covered self-expandable metal stent in patients unsuitable for cholecystectomy. Gastrointest Endosc. 2011; 74:176–181.
Article8. Moon JH, Choi HJ, Kim DC, et al. A newly designed fully covered metal stent for lumen apposition in EUS-guided drainage and access: a feasibility study (with videos). Gastrointest Endosc. 2014; 79:990–995.
Article9. Chan JHY, Teoh AYB. Current status of endoscopic gallbladder drainage. Clin Endosc. 2018; 51:150–155.
Article10. Jang JW, Lee SS, Song TJ, et al. Endoscopic ultrasound-guided transmural and percutaneous transhepatic gallbladder drainage are comparable for acute cholecystitis. Gastroenterology. 2012; 142:805–811.
Article11. Kwan V, Eisendrath P, Antaki F, Le Moine O, Devière J. EUS-guided cholecystenterostomy: a new technique (with videos). Gastrointest Endosc. 2007; 66:582–586.12. Lee SS, Park DH, Hwang CY, et al. EUS-guided transmural cholecystostomy as rescue management for acute cholecystitis in elderly or high-risk patients: a prospective feasibility study. Gastrointest Endosc. 2007; 66:1008–1012.13. Song TJ, Park DH, Eum JB, et al. EUS-guided cholecystoenterostomy with single-step placement of a 7F double-pigtail plastic stent in patients who are unsuitable for cholecystectomy: a pilot study (with video). Gastrointest Endosc. 2010; 71:634–640.
Article14. Kjaer DW, Kruse A, Funch-Jensen P. Endoscopic gallbladder drainage of patients with acute cholecystitis. Endoscopy. 2007; 39:304–308.
Article15. Mutignani M, Iacopini F, Perri V, et al. Endoscopic gallbladder drainage for acute cholecystitis: technical and clinical results. Endoscopy. 2009; 41:539–546.
Article16. Pannala R, Petersen BT, Gostout CJ, Topazian MD, Levy MJ, Baron TH. Endoscopic transpapillary gallbladder drainage: 10-year single center experience. Minerva Gastroenterol Dietol. 2008; 54:107–113.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Ultrasound-guided Drainage in Pancreatobiliary Diseases
- Single-pigtail plastic stent made from endoscopic nasobiliary drainage tubes in endoscopic ultrasound-guided gallbladder drainage: a retrospective case series
- Stent occlusion in endoscopic ultrasound-guided gallbladder drainage from bleeding mitigated by double pigtail plastic stent deployment within lumen apposing metal stent
- Endoscopic Transpapillary Gallbladder Stenting for Acute Cholecystitis in a Patient with Metastatic Pancreatic Cancer
- Recent development of endoscopic ultrasound-guided biliary drainage