Clin Endosc.
2020 Jan;53(1):82-89. 10.5946/ce.2019.073.
Experience of the Endoscopists Matters in Endoscopic Retrograde Cholangiopancreatography in Billroth II Gastrectomy Patients
- Affiliations
-
- 1Department of Gastroenterology, Kayseri Training and Education Hospital, Kayseri, Turkey
- 2Department of General Surgery, İstinye University, Gaziosmanpasa Medical Park Hospital, Istanbul, Turkey
- 3Department of Gastroenterology, Sakarya University Medical Faculty, Sakarya, Turkey
- 4Department of Gastroenterology, Faculty of Medicine, Bezmialem University, Istanbul, Turkey
- KMID: 2500909
- DOI: http://doi.org/10.5946/ce.2019.073
Abstract
- Background/Aims
Altered anatomy is a challenge in endoscopic retrograde cholangiopancreatography (ERCP) for patients with Billroth II anastomosis. In this study, we investigated the overall success and role of endoscopist experience.
Methods
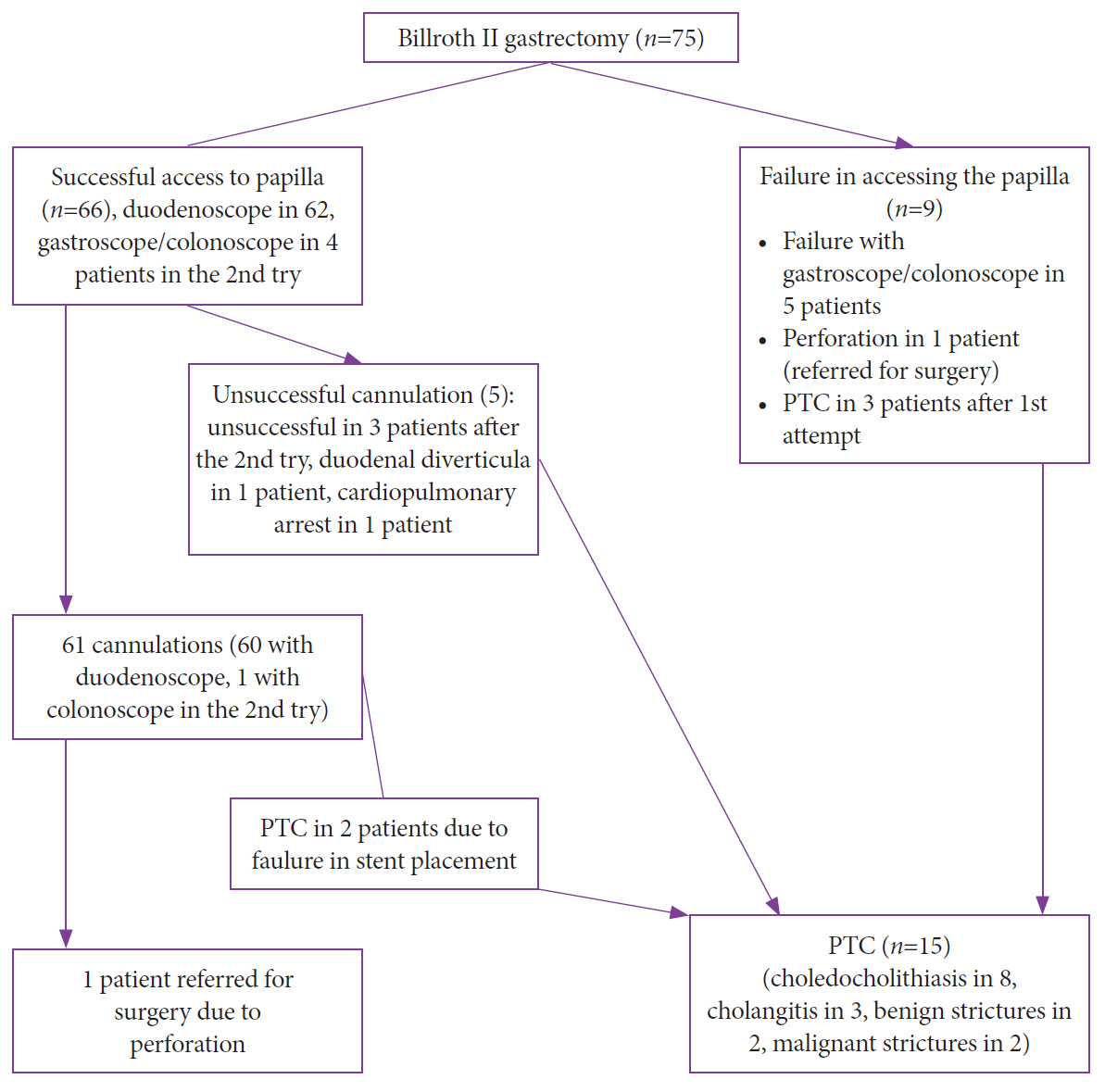
Data of patients who underwent ERCP between 2014 and 2018 after a previous Billroth II operation were retrieved retrospectively from 2 tertiary ERCP centers. The procedures were performed by 2 endoscopists with different levels of experience. Clinical success was defined as extraction of the stone, placement of a stent through a malignant stricture, and clinical and laboratory improvements in patients.
Results
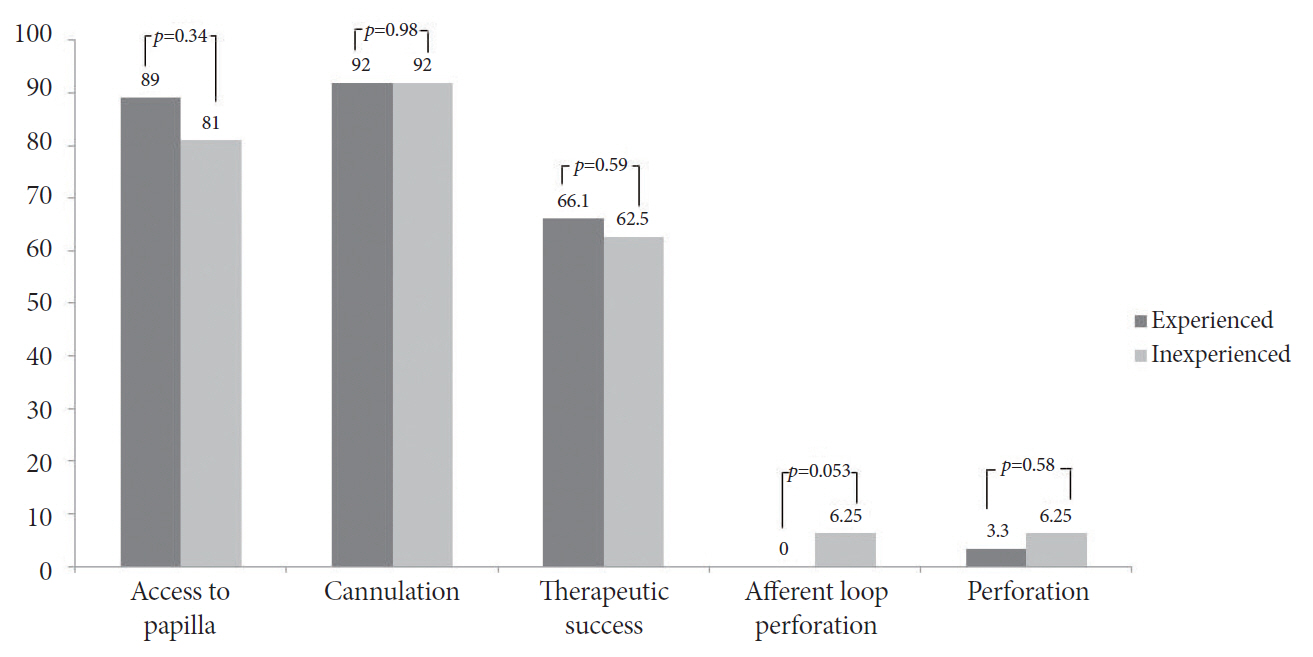
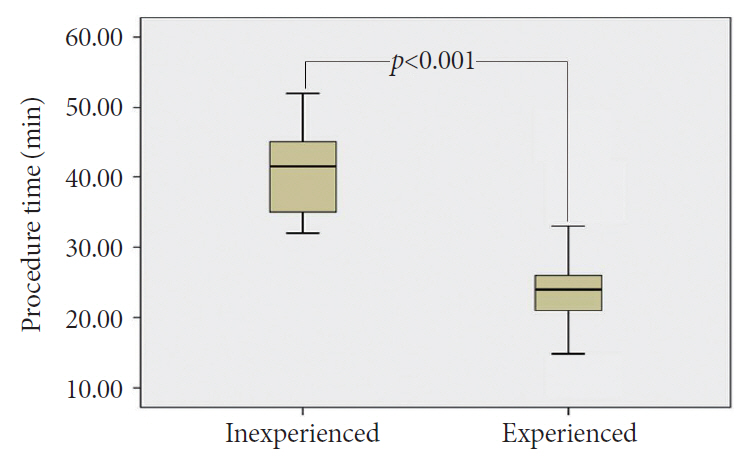
Seventy-five patients were included. The technical success rate was 83% for the experienced endoscopist and 75% for the inexperienced endoscopist (p=0.46). The mean (±standard deviation) procedure time was 23.8±5.7 min for the experienced endoscopist and 40.68±6.07 min for the inexperienced endoscopist (p<0.001). In total, 3 perforations (4%) were found. The rate of afferent loop perforation was 6.25% (1/16) for the inexperienced endoscopist and 0% (0/59) for the experienced endoscopist (p=0.053).
Conclusions
ERCP in patients who had undergone Billroth II gastrectomy was time consuming for the inexperienced endoscopist who should beware of the unique adverse events related to ERCP in patients with altered anatomy.
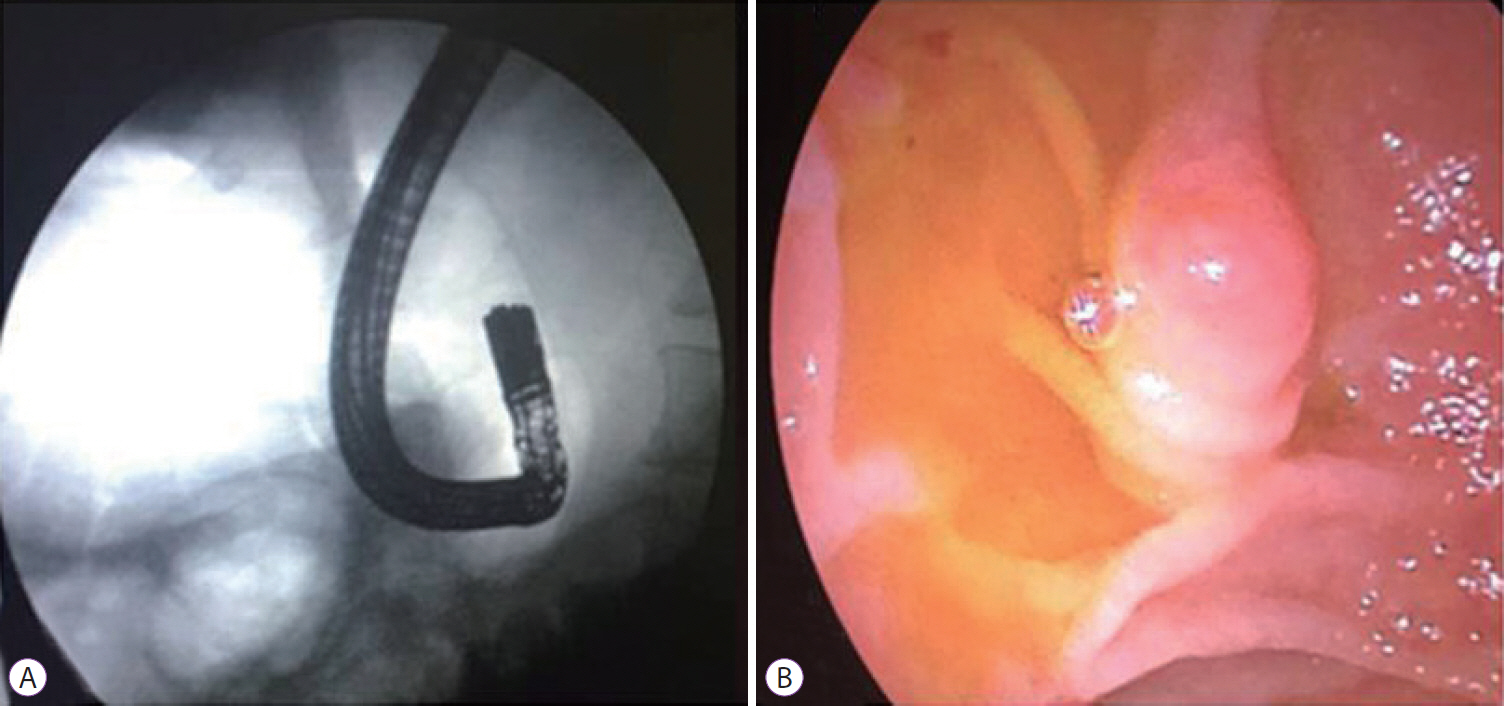
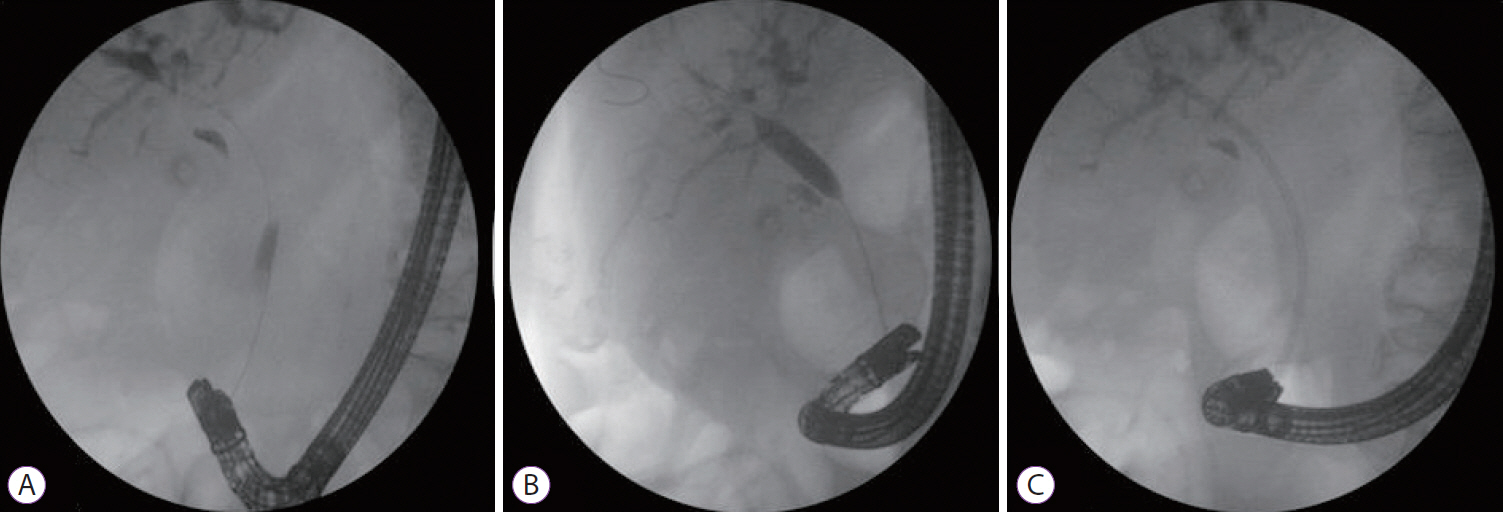
Figure
Cited by 1 articles
-
Experience of Endoscopists in Endoscopic Retrograde Cholangiopancreatography in Surgically Altered Anatomy Patients
Chang-Hwan Park
Clin Endosc. 2020;53(1):7-8. doi: 10.5946/ce.2020.008.
Reference
-
1. Nakahara K, Horaguchi J, Fujita N, et al. Therapeutic endoscopic retrograde cholangiopancreatography using an anterior oblique-viewing endoscope for bile duct stones in patients with prior Billroth II gastrectomy. J Gastroenterol. 2009; 44:212–217.
Article2. Prat F, Fritsch J, Choury AD, Meduri B, Pelletier G, Buffet C. Endoscopic sphincteroclasy: a useful therapeutic tool for biliary endoscopy in Billroth II gastrectomy patients. Endoscopy. 1997; 29:79–81.
Article3. Park TY, Kang JS, Song TJ, et al. Outcomes of ERCP in Billroth II gastrectomy patients. Gastrointest Endosc. 2016; 83:1193–1201.
Article4. Lin LF, Siauw CP, Ho KS, Tung JC. ERCP in post-Billroth II gastrectomy patients: emphasis on technique. Am J Gastroenterol. 1999; 94:144–148.
Article5. Kim MH, Lee SK, Lee MH, et al. Endoscopic retrograde cholangiopancreatography and needle-knife sphincterotomy in patients with Billroth II gastrectomy: a comparative study of the forward-viewing endoscope and the side-viewing duodenoscope. Endoscopy. 1997; 29:82–85.
Article6. Wu WG, Mei JW, Zhao MN, et al. Use of the conventional side-viewing duodenoscope for successful endoscopic retrograde cholangiopancreatography in postgastrectomy patients. J Clin Gastroenterol. 2016; 50:244–251.
Article7. Baysal B, Akin H, Masri O, Ince AT, Senturk H. A novel round insulated tip papillotome as an alternative to the classic needle-knife for precut sphincterotomy in endoscopic retrograde cholangiopancreatography. Gastroenterol Res Pract. 2015; 2015:972041.
Article8. Cotton PB, Lehman G, Vennes J, et al. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991; 37:383–393.
Article9. Bove V, Tringali A, Familiari P, et al. ERCP in patients with prior Billroth II gastrectomy: report of 30 years’ experience. Endoscopy. 2015; 47:611–616.
Article10. Wang F, Xu B, Li Q, et al. Endoscopic retrograde cholangiopancreatography in patients with surgically altered anatomy: one single center’s experience. Medicine (Baltimore). 2016; 95:e5743.11. Ciçek B, Parlak E, Dişibeyaz S, Koksal AS, Sahin B. Endoscopic retrograde cholangiopancreatography in patients with Billroth II gastroenterostomy. J Gastroenterol Hepatol. 2007; 22:1210–1213.
Article12. Byun JW, Kim JW, Sung SY, et al. Usefulness of forward-viewing endoscope for endoscopic retrograde cholangiopancreatography in patients with Billroth II gastrectomy. Clin Endosc. 2012; 45:397–403.
Article13. Nakahara K, Okuse C, Suetani K, et al. Endoscopic retrograde cholangiography using an anterior oblique-viewing endoscope in patients with altered gastrointestinal anatomy. Dig Dis Sci. 2015; 60:944–950.
Article14. Swarnkar K, Stamatakis JD, Young WT. Diagnostic and therapeutic endoscopic retrograde cholangiopancreaticography after Billroth II gastrectomy--safe provision in a district general hospital. Ann R Coll Surg Engl. 2005; 87:274–276.15. Forbes A, Cotton PB. ERCP and sphincterotomy after Billroth II gastrectomy. Gut. 1984; 25:971–974.
Article16. Moreels TG. Endoscopic retrograde cholangiopancreatography in patients with altered anatomy: how to deal with the challenges? World J Gastrointest Endosc. 2014; 6:345–351.
Article17. Safrany L, Neuhaus B, Portocarrero G, Krause S. Endoscopic sphincterotomy in patients with Billroth II gastrectomy. Endoscopy. 1980; 12:16–22.
Article18. Nakai Y, Kogure H, Yamada A, Isayama H, Koike K. Endoscopic management of bile duct stones in patients with surgically altered anatomy. Dig Endosc. 2018; 30 Suppl 1:67–74.
Article19. Mehta PP, Sanaka MR, Parsi MA, et al. Association of procedure length on outcomes and adverse events of endoscopic retrograde cholangiopancreatography. Gastroenterol Rep (Oxf). 2014; 2:140–144.
Article20. Faylona JM, Qadir A, Chan AC, Lau JY, Chung SC. Small-bowel perforations related to endoscopic retrograde cholangiopancreatography (ERCP) in patients with Billroth II gastrectomy. Endoscopy. 1999; 31:546–549.
Article21. Bergman JJ, van Berkel AM, Bruno MJ, et al. A randomized trial of endoscopic balloon dilation and endoscopic sphincterotomy for removal of bile duct stones in patients with a prior Billroth II gastrectomy. Gastrointest Endosc. 2001; 53:19–26.
Article22. Andriulli A, Loperfido S, Napolitano G, et al. Incidence rates of post-ERCP complications: a systematic survey of prospective studies. Am J Gastroenterol. 2007; 102:1781–1788.
Article23. Wang AY, Strand DS, Shami VM. Prevention of post-endoscopic retrograde cholangiopancreatography pancreatitis: medications and techniques. Clin Gastroenterol Hepatol. 2016; 14:1521–1532. e3.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Retrograde Cholangiopancreatography in Post Gastrectomy Patients
- Endoscopic Retrograde Cholangiopancreatography and Endoscopic Sphincterotomy in Patients with a Previous Billroth-II Resection
- Endoscopic Large-Diameter Balloon Dilation after Fistulotomy for the Removal of Bile Duct Stones in a Patient with Billroth II Gastrectomy
- Tips for Successful Endoscopic Retrograde Cholangiopancreatography in Patients with Billroth II Gastrectomy
- Therapeutic Endoscopic Retrograde Cholangiography in Patients with a Billroth II Gastrectomy: 2 cases of ERBD & 1 case of endoscopic stone retrievial