Ann Hepatobiliary Pancreat Surg.
2020 May;24(2):228-233. 10.14701/ahbps.2020.24.2.228.
Management of intractable pancreatic leak from iatrogenic pancreatic duct injury following resection of choledochal cyst in an adult patient
- Affiliations
-
- 1Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2500811
- DOI: http://doi.org/10.14701/ahbps.2020.24.2.228
Abstract
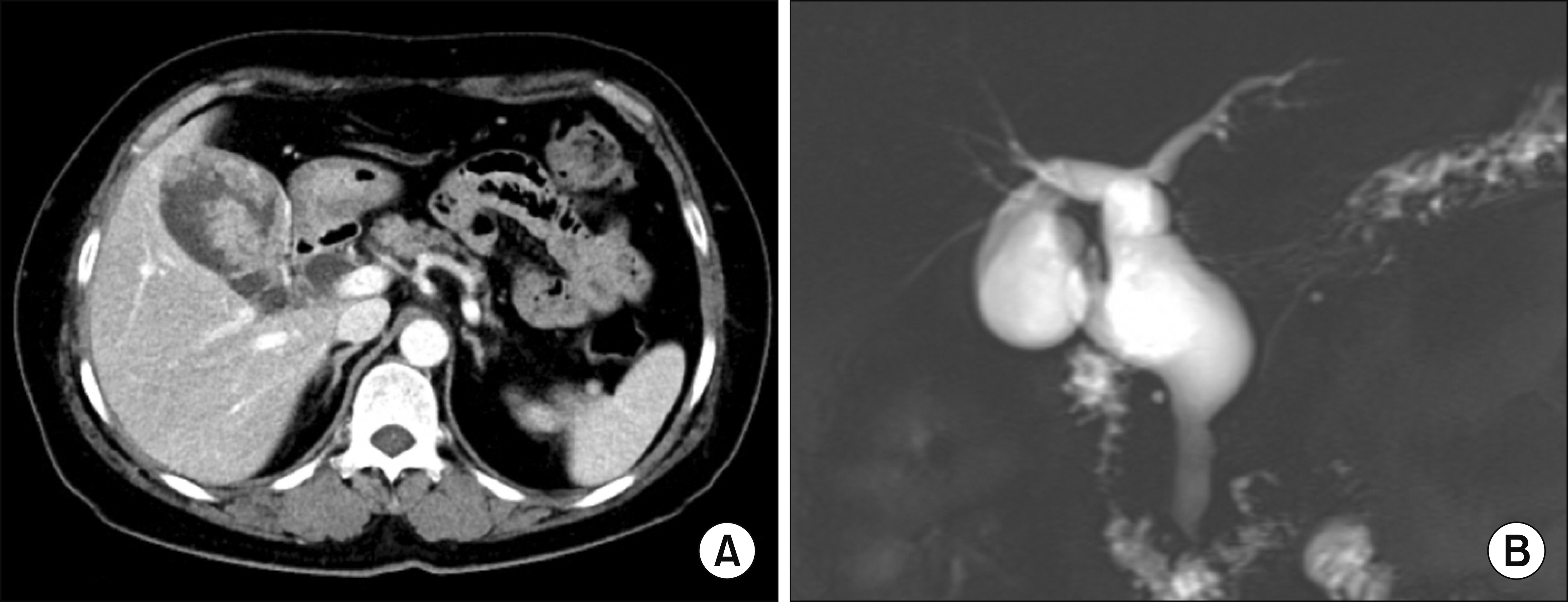
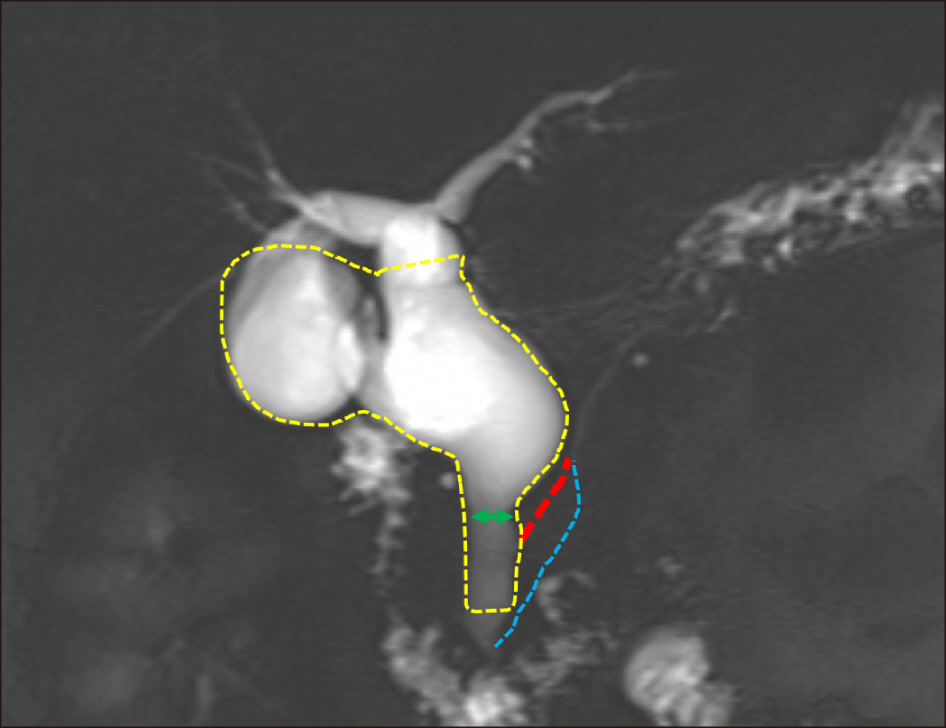
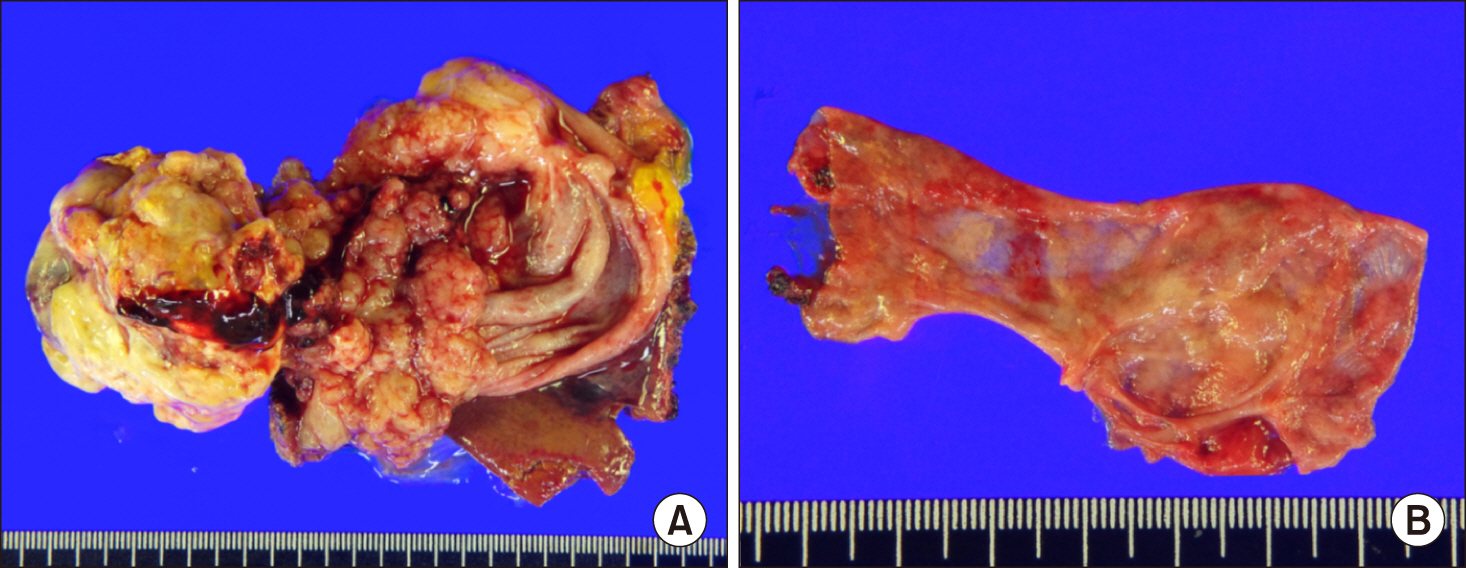
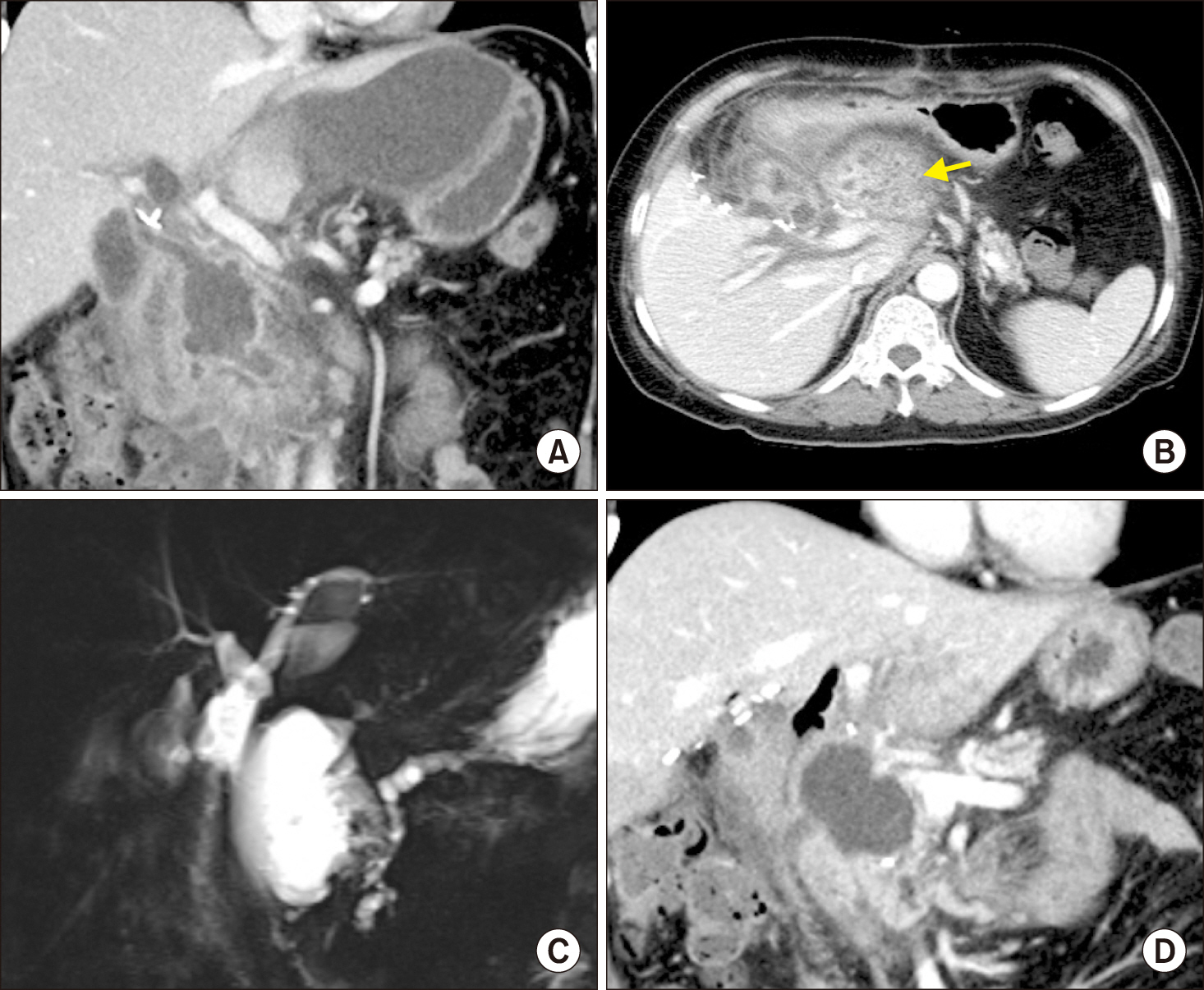
- Iatrogenic pancreatic duct injury can occur during resection of the choledochal cyst (CC). We herein present a case of postoperative pancreatic fistula (POPF) developed after resection of the CC in an adult patient with variant anomalous union of pancreatobiliary duct. The 55-year-old female patient underwent surgery after the diagnosis of CC-associated gallbladder cancer. During surgery, the CC mass was accidentally pulled out, by which the intrapancreatic CC portion was torn out from the main pancreatic duct. Since the pancreatic duct stump was not identified due to its small size, repair was not possible. The excavated defect at the pancreas head was closed securely combined with insertion of multiple drains. Postoperative POPF and peripancreatic fluid collection developed and the patient had to be fasted for 4 weeks. She was first discharged at 6 weeks after surgery. At 10 weeks, she was readmitted due to progression of peripancreatic fluid collection, which was controlled by percutaneous drain insertion. At 6 months, she was readmitted again due to repeated progression of peripancreatic fluid collection, which were controlled by endoscopic transmural duodenocystostomy. It took 8 months to resolve the pancreatic duct injury-associated pancreatitis. The experience in this case suggests that iatrogenic pancreatic duct injury during resection of CC can induce catastrophic complications, thus special attention should be paid to prevent pancreatic duct injury.
Figure
Cited by 1 articles
-
Development of intrahepatic cholangiocarcinoma at the remnant intrahepatic cyst portion 10 years after resection of type IV choledochal cyst
Suhyeon Ha, Shin Hwang, Lee Na Ryu
Ann Hepatobiliary Pancreat Surg. 2020;24(3):366-372. doi: 10.14701/ahbps.2020.24.3.366.
Reference
-
1. Fan F, Xu DP, Xiong ZX, Li HJ, Xin HB, Zhao H, et al. 2018; Clinical significance of intrapancreatic choledochal cyst excision in surgical management of type I choledochal cyst. J Int Med Res. 46:1221–1229. DOI: 10.1177/0300060517728598. PMID: 29322850. PMCID: PMC5972235.
Article2. Cho MJ, Hwang S, Lee YJ, Kim KH, Ahn CS, Moon DB, et al. 2011; Surgical experience of 204 cases of adult choledochal cyst disease over 14 years. World J Surg. 35:1094–1102. DOI: 10.1007/s00268-011-1009-7. PMID: 21360306.
Article3. Ando H, Kaneko K, Ito T, Watanabe Y, Seo T, Harada T, et al. 1996; Complete excision of the intrapancreatic portion of choledochal cysts. J Am Coll Surg. 183:317–321. PMID: 8843259.4. Oh SY, Kwon JH, Hwang S. 2019; Development of adenocarcinoma at the remnant intrapancreatic cyst 16 years after resection of the choledochal cyst. Ann Hepatobiliary Pancreat Surg. 23:192–196. DOI: 10.14701/ahbps.2019.23.2.192. PMID: 31225424. PMCID: PMC6558127.
Article5. Ng DW, Chiow AK, Poh WT, Tan SS. 2016; Metachronous cholangiocarcinoma 13 years post resection of choledochal cyst-is long-term follow-up useful? a case study and review of the literature. Surg Case Rep. 2:60. DOI: 10.1186/s40792-016-0187-9. PMID: 27307284. PMCID: PMC4909682.
Article6. Shimamura K, Kurosaki I, Sato D, Takano K, Yokoyama N, Sato Y, et al. 2009; Intrahepatic cholangiocarcinoma arising 34 years after excision of a type IV-A congenital choledochal cyst: report of a case. Surg Today. 39:247–251. DOI: 10.1007/s00595-008-3825-4. PMID: 19280286.
Article7. Kumamoto T, Tanaka K, Takeda K, Nojiri K, Mori R, Taniguchi K, et al. 2014; Intrahepatic cholangiocarcinoma arising 28 years after excision of a type IV-A congenital choledochal cyst: report of a case. Surg Today. 44:354–358. DOI: 10.1007/s00595-012-0387-2. PMID: 23090140. PMCID: PMC3898144.8. Nishiyama R, Shinoda M, Tanabe M, Masugi Y, Ueno A, Hibi T, et al. 2011; Intrahepatic cholangiocarcinoma arising 33 years after excision of a choledochal cyst: report of a case. Int Surg. 96:320–325. DOI: 10.9738/CC82.1. PMID: 22808614.9. Ohashi T, Wakai T, Kubota M, Matsuda Y, Arai Y, Ohyama T, et al. 2013; Risk of subsequent biliary malignancy in patients undergoing cyst excision for congenital choledochal cysts. J Gastroenterol Hepatol. 28:243–247. DOI: 10.1111/j.1440-1746.2012.07260.x. PMID: 22989043. PMCID: PMC3816325.
Article10. Koike M, Yasui K, Shimizu Y, Kodera Y, Hirai T, Morimoto T, et al. 2002; Carcinoma of the hepatic hilus developing 21 years after biliary diversion for choledochal cyst: a case report. Hepatogastroenterology. 49:1216–1220. PMID: 12239908.11. Suzuki S, Amao K, Harada N, Tanaka S, Hayashi T, Suzuki M, et al. 2004; A case of intrahepatic cholangiocarcinoma arising 26 years after excision of congenital biliary dilatation. Jpn J Gastroenterol Surg. 37:416–421. DOI: 10.5833/jjgs.37.416.
Article12. Ono S, Sakai K, Kimura O, Iwai N. 2008; Development of bile duct cancer in a 26-year-old man after resection of infantile choledochal cyst. J Pediatr Surg. 43:E17–E19. DOI: 10.1016/j.jpedsurg.2008.01.073. PMID: 18558159.
Article13. Yoon JH. 2011; Magnetic resonance cholangiopancreatography diagnosis of choledochal cyst involving the cystic duct: report of three cases. Br J Radiol. 84:e18–e22. DOI: 10.1259/bjr/77844300. PMID: 21172959. PMCID: PMC3473806.
Article14. Shimizu T, Suzuki R, Yamashiro Y, Segawa O, Yamataka A, Kuwatsuru R. 2001; Magnetic resonance cholangiopancreatography in assessing the cause of acute pancreatitis in children. Pancreas. 22:196–199. DOI: 10.1097/00006676-200103000-00014. PMID: 11249076.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pancreas Divisum, Choledochal Cyst and Pancreatic Stones in a 50-year-old Man
- Preemptive resection of choledochal cyst during redo resection of gallbladder cancer following laparoscopic cholecystectomy
- A Choledochal Cyst Combined with a Hilar Cholangiocarcinoma
- An Acquired Choledochal Cyst from Anomalous Pancreatobiliary Duct Union
- Cholangiopancreatographic Findings of Choledochal Cyst: Emphasis on the Pancreatobiliary Union