Ann Hepatobiliary Pancreat Surg.
2020 May;24(2):144-149. 10.14701/ahbps.2020.24.2.144.
Technical refinement of prosthetic vascular graft anastomosis to recipient inferior vena cava for secure middle hepatic vein reconstruction in living donor liver transplantation
- Affiliations
-
- 1Division of Hepatobiliary Surgery and Liver Transplantation, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2500774
- DOI: http://doi.org/10.14701/ahbps.2020.24.2.144
Abstract
- Backgrounds/Aims
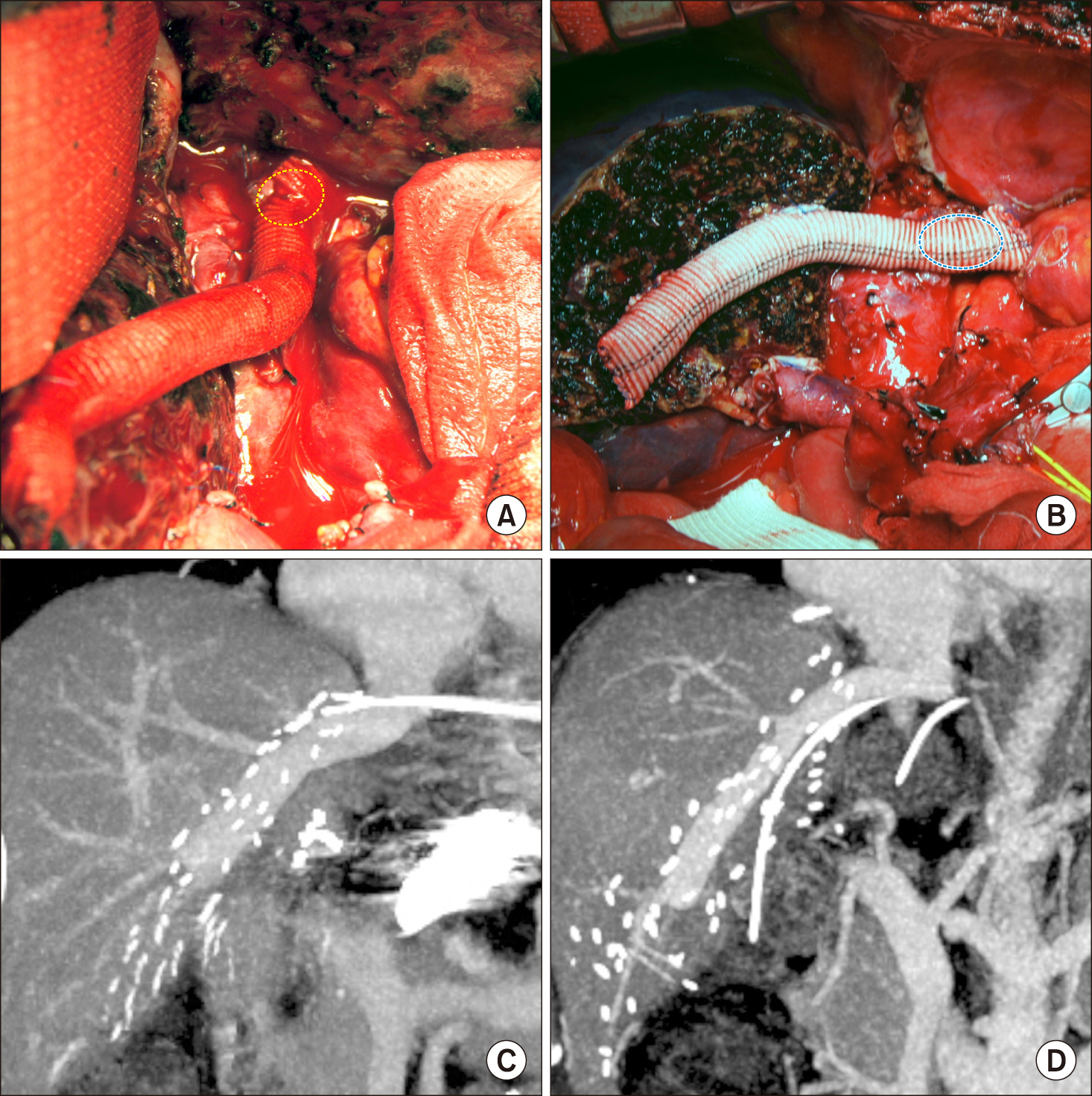
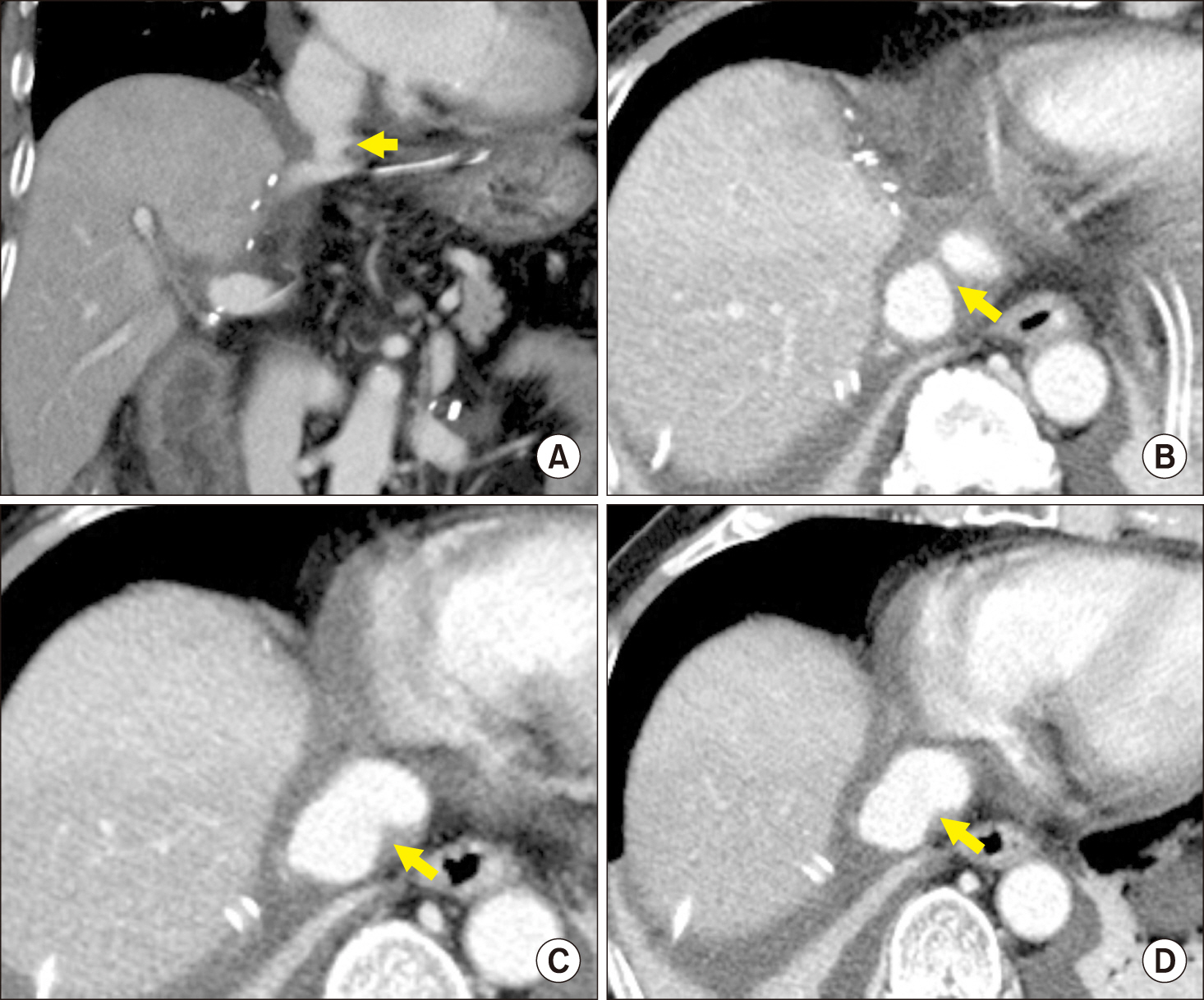
Hemashield vascular grafts has been used for middle hepatic vein (MHV) reconstruction during living donor liver transplantation (LDLT). We occasionally encounter outflow disturbance of MHV conduit at the anastomotic stump of the middle-left hepatic vein (MLHV) trunk. To mitigate the disturbance, we carried out a series of studies regarding hemodynamics-compliant MHV reconstruction.
Methods
This study comprised of three parts: Part 1: Determining the causes of outflow disturbance; Part 2: Computational simulative analysis; and, Part 3: Clinical application of our refined technique. The types of Hemashield conduit-MLHV stump reconstruction were end-to-end anastomosis (type 1), side-toend anastomosis (type 2), and oblique cutting of the conduit end and patch plasty (type 3).
Results
In Part 1 study, the reconstruction types were type 1 in 23, type 2 in 25, and type 3 in 2. Significant anastomotic stenosis was identified in 7 (30.4%) in type 1, 6 (24.0%) in type 2, and none (0%) in type 3. The size of MLHV stump was the most important factor for anastomotic stenosis. Through Part 2 study, technical knacks were developed as follows: the conduit end was cut in a dumb-bell shape and a vessel patch attached; and then sutured bidirectionally from the 9 o’clock direction. In Part 3 study, these knacks were applied to 5 patients and none of them experienced noticeable anastomotic stenosis.
Conclusions
Our refined technique to perform conduit-MLHV stump anastomosis appears to reduce the risk of anastomotic outflow disturbance for relatively small MLHV stump.
Keyword
Figure
Cited by 1 articles
-
Patency of Hemashield grafts versus ringed Gore-Tex grafts in middle hepatic vein reconstruction for living donor liver transplantation
Sang Hoon Kim, Shin Hwang, Minjae Kim, Tae-Yong Ha, Gi-Won Song, Dong-Hwan Jung, Chul-Soo Ahn, Deok-Bog Moon, Ki-Hun Kim, Gil-Chun Park, Sung-Gyu Lee
Ann Hepatobiliary Pancreat Surg. 2021;25(1):46-53. doi: 10.14701/ahbps.2021.25.1.46.
Reference
-
1. Hwang S, Lee SG, Lee YJ, Sung KB, Park KM, Kim KH, et al. 2006; Lessons learned from 1,000 living donor liver transplantations in a single center: how to make living donations safe. Liver Transpl. 12:920–927. DOI: 10.1002/lt.20734. PMID: 16721780.
Article2. Hwang S, Lee SG, Ahn CS, Park KM, Kim KH, Moon DB, et al. 2005; Cryopreserved iliac artery is indispensable interposition graft material for middle hepatic vein reconstruction of right liver grafts. Liver Transpl. 11:644–649. DOI: 10.1002/lt.20430. PMID: 15915499.
Article3. Sugawara Y, Makuuchi M, Akamatsu N, Kishi Y, Niiya T, Kaneko J, et al. 2004; Refinement of venous reconstruction using cryopreserved veins in right liver grafts. Liver Transpl. 10:541–547. DOI: 10.1002/lt.20129. PMID: 15048798.
Article4. Hwang S, Lee SG, Song GW, Lee HJ, Park JI, Ryu JH. 2007; Use of endarterectomized atherosclerotic artery allograft for hepatic vein reconstruction of living donor right lobe graft. Liver Transpl. 13:306–308. DOI: 10.1002/lt.21045. PMID: 17256786.
Article5. Hwang S, Jung DH, Ha TY, Ahn CS, Moon DB, Kim KH, et al. 2012; Usability of ringed polytetrafluoroethylene grafts for middle hepatic vein reconstruction during living donor liver transplantation. Liver Transpl. 18:955–965. DOI: 10.1002/lt.23456. PMID: 22511404.
Article6. Park GC, Hwang S, Ha TY, Song GW, Jung DH, Ahn CS, et al. 2019; Hemashield vascular graft is a preferable prosthetic graft for middle hepatic vein reconstruction in living donor liver transplantation. Ann Transplant. 24:639–646. DOI: 10.12659/AOT.919780. PMID: 31844037. PMCID: PMC6936210.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Tailored techniques of graft outflow vein reconstruction in pediatric liver transplantation at Asan Medical Center
- Quilt unification venoplasty of the right hepatic veins enabling double inferior vena cava anastomosis in living donor liver transplantation using a right liver graft
- Technical refinement of inferior vena cava replacement using a synthetic vascular graft in living donor liver transplantation
- Technical refinement of prosthetic vascular graft anastomosis to recipient inferior vena cava for secure middle hepatic vein reconstruction in living donor liver transplantation
- Standardized surgical techniques for adult living donor liver transplantation using a modified right lobe graft: a video presentation from bench to reperfusion