Clin Exp Otorhinolaryngol.
2020 May;13(2):203-208. 10.21053/ceo.2019.01207.
Feasibility of Brachial Plexus Schwannoma Enucleation With Intraoperative Neuromonitoring
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, SMG-SNU Boramae Medical Center, Seoul, Korea
- 2Department of Otorhinolaryngology-Head and Neck Surgery, Seoul National University Bundang Hospital, Seongnam, Korea
- KMID: 2500294
- DOI: http://doi.org/10.21053/ceo.2019.01207
Abstract
Objectives
. To evaluate the feasibility of brachial plexus schwannoma enucleation under intraoperative neuromonitoring.
Methods
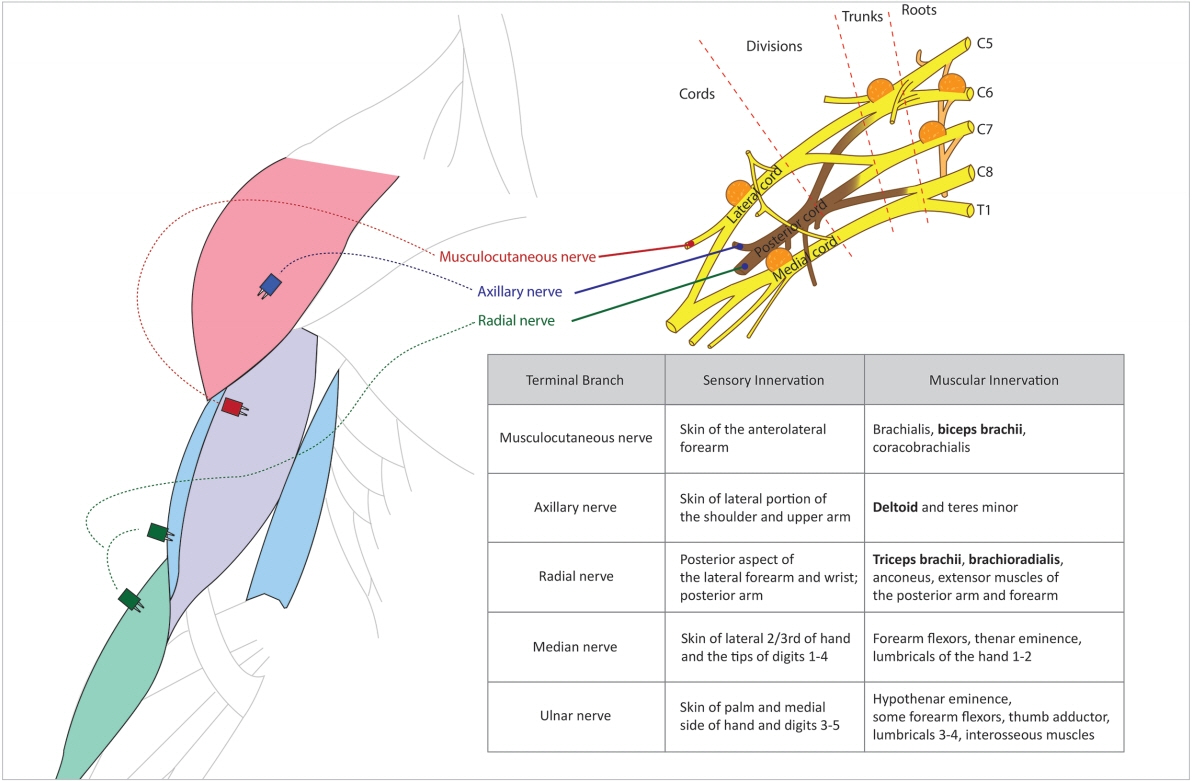
. Five patients who were treated for brachial plexus schwannoma under intraoperative neuromonitoring from 2008 to 2018 were included in this retrospective review. Neuromonitoring was performed with a 100-μV event threshold of the neuromonitoring system (NIM-2 or 3) at the deltoid, biceps brachii, triceps brachii, and brachioradialis muscles. Patient characteristics, tumor size and location, intraoperative neuromonitoring findings, and postoperative function were evaluated.
Results
. The intraoperative neuromonitoring findings were in accordance with the preoperative assessment of the included nerve root. Three patients had no postoperative morbidity, one patient had temporary paresthesia of the forearm for 2 months, and one patient mild loss of grip strength for 1 month.
Conclusion
. Intraoperative neuromonitoring of the arm and forearm muscles during enucleation of brachial plexus schwannoma promoted confident and successful surgery with minimal postoperative morbidity.
Figure
Reference
-
1. Biswas D, Marnane CN, Mal R, Baldwin D. Extracranial head and neck schwannomas: a 10-year review. Auris Nasus Larynx. 2007; Sep. 34(3):353–9.2. Moukarbel RV, Sabri AN. Current management of head and neck schwannomas. Curr Opin Otolaryngol Head Neck Surg. 2005; 13(2):117–22.
Article3. Shrikrishna BH, Jyothi AC, Kulkarni NH, Mazhar MS. Extracranial head and neck schwannomas: our experience. Indian J Otolaryngol Head Neck Surg. 2016; Jun. 68(2):241–7.
Article4. Zhang H, Cai C, Wang S, Liu H, Ye Y, Chen X. Extracranial head and neck schwannomas: a clinical analysis of 33 patients. Laryngoscope. 2007; Feb. 117(2):278–81.
Article5. Liu HL, Yu SY, Li GK, Wei WI. Extracranial head and neck Schwannomas: a study of the nerve of origin. Eur Arch Otorhinolaryngol. 2011; Sep. 268(9):1343–7.
Article6. Yasumatsu R, Nakashima T, Miyazaki R, Segawa Y, Komune S. Diagnosis and management of extracranial head and neck schwannomas: a review of 27 cases. Int J Otolaryngol. 2013; 2013:973045.
Article7. Jia X, Yang J, Chen L, Yu C, Kondo T. Primary Brachial plexus tumors: clinical experiences of 143 cases. Clin Neurol Neurosurg. 2016; Sep. 148:91–5.
Article8. Valentino J, Boggess MA, Ellis JL, Hester TO, Jones RO. Expected neurologic outcomes for surgical treatment of cervical neurilemomas. Laryngoscope. 1998; Jul. 108(7):1009–13.
Article9. Ganju A, Roosen N, Kline DG, Tiel RL. Outcomes in a consecutive series of 111 surgically treated plexal tumors: a review of the experience at the Louisiana State University Health Sciences Center. J Neurosurg. 2001; Jul. 95(1):51–60.
Article10. Kehoe NJ, Reid RP, Semple JC. Solitary benign peripheral-nerve tumours: review of 32 years’ experience. J Bone Joint Surg Br. 1995; May. 77(3):497–500.
Article11. Adani R, Baccarani A, Guidi E, Tarallo L. Schwannomas of the upper extremity: diagnosis and treatment. Chir Organi Mov. 2008; Sep. 92(2):85–8.
Article12. Park MJ, Seo KN, Kang HJ. Neurological deficit after surgical enucleation of schwannomas of the upper limb. J Bone Joint Surg Br. 2009; Nov. 91(11):1482–6.
Article13. Russell SM. Preserve the nerve: microsurgical resection of peripheral nerve sheath tumors. Neurosurgery. 2007; Sep. 61(3 Suppl):113–7.
Article14. Lee HJ, Kim JH, Rhee SH, Gong HS, Baek GH. Is surgery for brachial plexus schwannomas safe and effective. Clin Orthop Relat Res. 2014; Jun. 472(6):1893–8.
Article15. Huang JH, Zaghloul K, Zager EL. Surgical management of brachial plexus region tumors. Surg Neurol. 2004; Apr. 61(4):372–8.
Article16. Sood AJ, Houlton JJ, Nguyen SA, Gillespie MB. Facial nerve monitoring during parotidectomy: a systematic review and meta-analysis. Otolaryngol Head Neck Surg. 2015; Apr. 152(4):631–7.
Article17. Hu J, Fleck TR, Xu J, Hsu JV, Xu HX. Contemporary changes with the use of facial nerve monitoring in chronic ear surgery. Otolaryngol Head Neck Surg. 2014; Sep. 151(3):473–7.
Article18. Bacuzzi A, Dralle H, Randolph GW, Chiang FY, Kim HY, Barczynski M, et al. Safety of continuous intraoperative neuromonitoring (C-IONM) in thyroid surgery. World J Surg. 2016; Mar. 40(3):768–9.
Article19. Grosheva M, Klussmann JP, Grimminger C, Wittekindt C, Beutner D, Pantel M, et al. Electromyographic facial nerve monitoring during parotidectomy for benign lesions does not improve the outcome of postoperative facial nerve function: a prospective two-center trial. Laryngoscope. 2009; Dec. 119(12):2299–305.
Article20. Eisele DW, Wang SJ, Orloff LA. Electrophysiologic facial nerve monitoring during parotidectomy. Head Neck. 2010; Mar. 32(3):399–405.
Article21. Lowry TR, Gal TJ, Brennan JA. Patterns of use of facial nerve monitoring during parotid gland surgery. Otolaryngol Head Neck Surg. 2005; Sep. 133(3):313–8.
Article22. Chung TK, Rosenthal EL, Porterfield JR, Carroll WR, Richman J, Hawn MT. Examining national outcomes after thyroidectomy with nerve monitoring. J Am Coll Surg. 2014; Oct. 219(4):765–70.
Article23. Baek SK, Lee K, Oh D, Kang SH, Kwon SY, Woo JS, et al. Efficiency of intraoperative neuromonitoring on voice outcomes after thyroid surgery. Auris Nasus Larynx. 2017; Oct. 44(5):583–59.
Article