Korean J Adult Nurs.
2020 Feb;32(1):1-9. 10.7475/kjan.2020.32.1.1.
Noise Level by Type in Adult Intensive Care Units of a Tertiary Teaching Hospital in Korea
- Affiliations
-
- 1Unit Manager, Neurological Intensive Care Unit, Seoul ST. Mary's Hospital, The Catholic University of Korea, Seoul, Korea.
- 2Unit Manager, Surgical Intensive Care Unit, Seoul ST. Mary's Hospital, The Catholic University of Korea, Seoul, Korea.
- 3Unit Manager, Cardiac Care Unit, Seoul ST. Mary's Hospital, The Catholic University of Korea, Seoul, Korea.
- 4Critical Care Team Leader, Nursing Department, Seoul ST. Mary's Hospital, The Catholic University of Korea, Seoul, Korea.
- 5Professor, College of Nursing, The Catholic University of Korea, Seoul, Korea. ysyoo@catholic.ac.kr
- KMID: 2471024
- DOI: http://doi.org/10.7475/kjan.2020.32.1.1
Abstract
- PURPOSE
This study aimed to investigate the actual noise conditions in adult Intensive Care Units (ICUs) according to type, time, day of the week, and area.
METHODS
This study was conducted from February to March 2018. ICU noise levels were examined using a noise meter with a microphone an amplifier, auditory correction circuit, and indicator meter capable of directly reading A-weighted decibels (dBA). Noise was measured for 24 hours for seven days and the average dBA, maximum dBA, and minimum dBA were recorded.
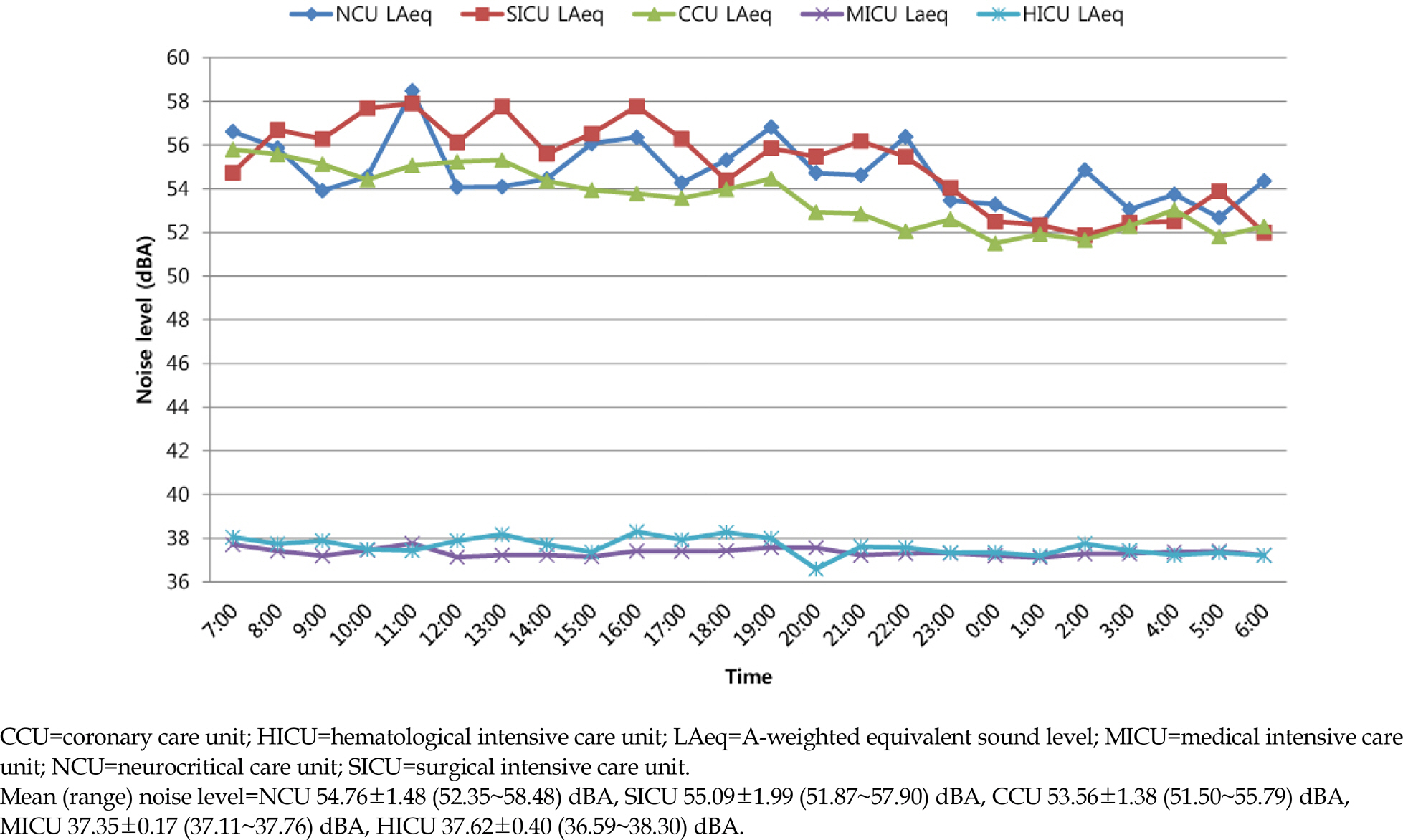
RESULTS
The highest mean noise level was 58.48 dBA (range of 57.62~65.27), while lowest was 51.65 dBA (range of 51.36~52.86). Average noise levels on weekdays and weekends were over 50 dBA(the open zone was measured at 56.61 dBA, while the isolation zone was measured at 52.45 dBA. Further, daytime, evening work-times and weekdays were measured above 60 dBA, while nighttime noise levels were below 60 dBA. Finally, average noise levels during turnarounds, shift changes, and rounding times were above 60 dBA; open zone had higher average noise levels than the isolation zone.
CONCLUSION
This study showed that ICU noise levels exceeded those recommended by the World Health Organization regardless of type of noise, day of the week, or time. Therefore, studies are proposed to identify the need or importance of noise management by ICU personnel to reduce noise in ICUs. It also proposes studies to develop and apply noise reduction strategies that can be easily used in practice, reflecting the various characteristics of noise in ICUs.
MeSH Terms
Figure
Reference
-
1. Konkani A, Oakley B. Noise in hospital intensive care units-A critical review of a critical topic. Journal of Critical Care. 2012; 27(5):522. .e1-9.https://doi.org/10.1016/j.jcrc.2011.09.003.
Article2. Joo HJ. Intensive care unit noise is higher than WHO standard, and patients complain of sleep disturbance and stress[Internet]. N. ursing Newspaper: Korean Nurses Association;2015. [cited 2015 December 24]. Available from:. http://www.nursenews.co.kr/main/ArticleDetailView.asp?sSection=75&idx=11087&intPage=1.3. Darbyshire JL, Young JD. An investigation of sound levels on intensive care units with reference to the WHO guidelines. Critical Care. 2013; 17(5):R187. https://doi.org/10.1186/cc12870.
Article4. Park M, Kohlrausch A, de Bruijn W, de Jager P, Simons K. Analysis of the soundscape in an intensive care unit based on the annotation of an audio recording. The Journal of the Acous-tical Society of America. 2014; 135(4):1875–86. https://doi.org/10.1121/1.4868367.
Article5. Akansel N, Kaymakci S. Effects of intensive care unit noise on patients: a study on coronary artery bypass graft surgery patients. Journal of Clinical Nursing. 2008; 17(12):1581–90. https://doi.org/10.1111/j.1365-2702.2007.02144.x.
Article6. Xie H, Kang J, Mills GH. Clinical review: the impact of noise on patients' sleep and the effectiveness of noise reduction strategies in intensive care units. Critical Care. 2009; 13(2):208. https://doi.org/10.1186/cc7154.
Article7. Krueger C, Schue S, Parker L. Neonatal intensive care unit sound levels before and after structural reconstruction. MCN, American Journal of Maternal Child Nursing. 2007; 32(6):358–62.
Article8. Litton E, Carnegie V, Elliott R, Webb SA. The efficacy of ear-plugs as a sleep hygiene strategy for reducing delirium in the ICU: a systematic review and metaanalysis. Critical Care Medicine. 2016; 44(5):992–9. https://doi.org/10.1097/CCM.0000000000001557.9. Kamdar BB, Needham DM, Collop NA. Sleep deprivation in critical illness: its role in physical and psychological recovery. Journal of Intensive Care Medicine. 2012; 27(2):97–111. https://doi.org/10.1177/0885066610394322.10. Berglund B, Lindvall T, Schwela DH. Guidelines for community noise. http://www.who.int/docstore/peh/noise/guidelines2.html. (accessed Mar/16/2011).11. Son YJ. The relationship between noise and sleep patterns in intensive care units. The Journal of Korean Academic Society of Adult Nursing. 2001; 13(2):209–22.12. MacKenzie D, Galbrun L. Noise levels and noise sources in acute care hospital wards. Building Service Engineering. 2007; 28(2):117–31. https://doi.org/10.1177/0143624406074468.
Article13. Darbyshire JL, Müller-Trapet M, Cheer J, Fazi FM, Young JD. Mapping sources of noise in an intensive care unit. Anaes-thesia. 2019; 74(8):1018–25. https://doi.org/10.1111/anae.14690.
Article14. Simons KS, Verweij E, Lemmens PMC, Jelfs S, Park M, Spronk PE, et al. Noise in the intensive care unit and its influence on sleep quality: a multicenter observational study in Dutch intensive care units. Critical Care. 2018; 22(1):250. https://doi.org/10.1186/s13054-018-2182-y.
Article15. Tegnestedt C, Günther A, Reichard A, Bjurström R, Alvarsson J, Martling CR, et al. Levels and sources of sound in the intensive care unit - an observational study of three room types. Acta Anaesthesiologica Scandinavica. 2013; 57(8):1041–50. https://doi.org/10.1111/aas.12138.
Article16. Kim MY, Park UJ. Noise levels in intensive care units and patient's perception. Journal of Korean Critical Care Nursing. 2015; 8(1):41–9.17. Berglund B, Lindvall T, Schwela DH. Guidelines for community noise. Paper presented at: WHO- expert task force meeting. 1999. April; London, UK.18. Matook SA, Sullivan MC, Salisbury A. Variations of NICU sound by location and time of day. Neonatal Network. 2010; 29(2):87–95.
Article19. Noh WJ, Sohng KY, Lee YM. Sleep Patterns of ICU Patients, Characteristics and Factors Related to Sleep Disturbance. The Korean Journal of Fundamentals of Nursing. 2005; 12(2):247–54.20. Dennis CM, Lee R, Woodard EK, Szalaj JJ, Walker CA. Benefits of quiet time for neuro-intensive care patients. Journal of Neu-roscience Nursing. 2010; 42(4):217–24. https://doi.org/10.1097/JNN.0b013e3181e26c20.
Article21. Watson J, Kinstler A, Vidonish WP, Wagner M, Lin L, Davis KG, et al. Impact of noise on nurses in pediatric intensive care units. American Journal of Critical Care. 2015; 24(5):377–84. https://doi.org/10.4037/ajcc2015260.
Article22. Li SY, Wang TJ, Vivienne Wu SF, Liang SY, Tung HH. Efficacy of controlling nighttime noise and activities to improve patients' sleep quality in a surgical intensive care unit. Journal of Clinical Nursing. 2011; 20(3-4):396–407. https://doi.org/10.1111/j.1365-2702.2010.03507.x.
Article23. Crawford KJ, Barnes LA, Peters TM, Falk J, Gehlbach BK. Iden-tifying determinants of noise in a medical intensive care unit. Journal of Occupational and Environmental Hygiene. 2018; 15(12):810–7. https://doi.org/10.1080/15459624.2018.1515491.
Article24. Cordova AC, Logishetty K, Fauerbach J, Price LA, Gibson BR, Milner SM. Noise levels in a burn intensive care unit. Burns. 2013; 39(1):44–8. https://doi.org/10.1016/j.burns.2012.02.033.
Article25. Garrido Galindo AP, Camargo Caicedo Y, Vélez-Pereira AM. Noise level in intensive care units of a public university hospital in Santa Marta (Colombia). Medicina Intensiva. 2016; 40(7):403–10. https://doi.org/10.1016/j.medin.2015.11.011.
Article26. Disher TC, Benoit B, Inglis D, Burgess SA, Ellsmere B, Hewitt BE, et al. Striving for optimum noise-decreasing strategies in critical care: initial measurements and observations. Journal of Perinatal and Neonatal Nursing. 2017; 31(1):58–66. https://doi.org/10.1097/JPN.0000000000000229.27. Jung HW. Comparison between noise levels of hospital wards and the nurses efforts for noise management in selected general hospital. Korean Journal of Occupational Health Nursing. 2001; 10(2):174–82.28. Johansson L, Knutsson S, Bergbom I, Lindahl B. Noise in the ICU patient room - Staff knowledge and clinical improvements. Intensive and Critical Care Nursing. 2016; 35:1–9. https://doi.org/10.1016/j.iccn.2016.02.005.
Article29. Kol E, Demircan A, Erdoğ an A, Gencer Z, Erengin H. The effectiveness of measures aimed at noise reduction in an intensive care unit. Workplace Health & Safety. 2015; 63(12):539–45. https://doi.org/10.1177/2165079915607494.
Article30. Qutub HO, El-Said KF. Assessment of ambient noise levels in the intensive care unit of a university hospital. Journal of Fa-mily and Community Medicine. 2009; 16(2):53–7.31. Stafford A, Haverland A, Bridges E. Noise in the ICU. American Journal of Nursing. 2014; 114(5):57–63. https://doi.org/10.1097/01.NAJ.0000446780.99522.90.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Development and Application of an Intervention for Noise Reduction in Intensive Care Units
- Changes in Nurse Staffing Grades in General Wards and Adult and Neonatal Intensive Care Units
- Rehabilitation in Intensive Care Unit
- Noise Level and Frequency Experienced by Premature Infants Receiving Incubator Care in the Neonatal Intensive Care Unit
- Noise and Room Acoustic Conditions in a Tertiary Referral Hospital, Seoul National University Hospital