Yonsei Med J.
2020 Mar;61(3):218-228. 10.3349/ymj.2020.61.3.218.
Leisure Time Physical Activity to Reduce Metabolic Syndrome Risk: A 10-Year Community-Based Prospective Study in Korea
- Affiliations
-
- 1Department of Medical Science, Yonsei University Graduate School, Seoul, Korea.
- 2Department of Preventive Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea. kohhj@yonsei.ac.kr
- 3Department of Cardiology, Yonsei University Wonju College of Medicine, Wonju, Korea.
- 4Institute of Genomic Cohort, Yonsei University Wonju College of Medicine, Wonju, Korea.
- 5Department of Occupational Therapy, Yonsei University College of Health Science, Wonju, Korea.
- 6Institute of Occupational & Environmental Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea.
- KMID: 2470918
- DOI: http://doi.org/10.3349/ymj.2020.61.3.218
Abstract
- PURPOSE
Metabolic syndrome (MetS) is a major public health problem related to increased risks of cardiovascular disease and type 2 diabetes. We investigated whether recommended levels of leisure time physical activity (LTPA) decrease the risk of MetS in a community-based prospective cohort study (Ansung and Ansan cohort).
MATERIALS AND METHODS
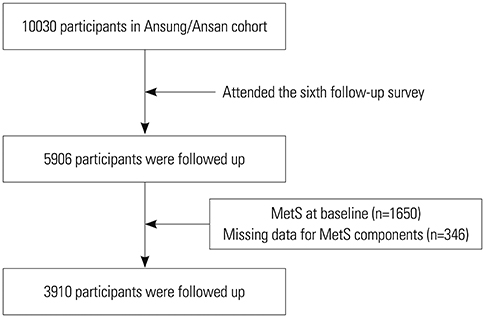
A total of 3910 adults (1890 men, 2020 women) without MetS examined in 2001-2002 (baseline) were included in this study and followed up from 2013 to 2014. We measured LTPA energy expenditure using the standard metabolic equivalent value [metabolic equivalent of task (MET)-h/wk]. Individuals were categorized into five groups (physically inactive, 0.1 to <7.5, 7.5 to <15.0, 15.0 to <22.5, 22.5 to <40.0, and ≥40.0 MET-h/wk).
RESULTS
The mean follow-up period was 11.8 years. Among the cohort, 482 men (25.5%) and 541 women (26.8%) were diagnosed with newly developed MetS. Multivariate logistic analysis revealed a 4.4% lower MetS risk among those performing two to three times the recommended minimum of 7.5 MET-h/wk [multivariate relative risk (RR), 0.956; 95% confidence interval (CI), 0.654-1.398] and a 21.9% lower risk among those performing three to four times the physical activity minimum (multivariate RR, 0.781; 95% CI, 0.574-1.063). This association was only significant in females performing three to four times the minimum (crude RR, 0.655; 95% CI, 0.432-0.994).
CONCLUSION
We noted that physical activity at more than 2 times the recommended minimum prevents MetS. Healthcare professionals should encourage inactive adults to be physically active during their leisure time to take advantage of its health benefits.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Accelerometer and Self-reported Sedentary Time Related to Metabolic Syndrome
Jungjun Lim, Hoyong Sung, Joon-Sik Kim, Geonhui Kim, Jungwoon Kim, Yeonsoo Kim
Korean J Sports Med. 2022;40(3):189-196. doi: 10.5763/kjsm.2022.40.3.189.
Reference
-
1. Saklayen MG. The global epidemic of the metabolic syndrome. Curr Hypertens Rep. 2018; 20:12.
Article2. Grundy SM. Metabolic syndrome: a multiplex cardiovascular risk factor. J Clin Endocrinol Metab. 2007; 92:399–404.
Article3. Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome. Circulation. 2009; 120:1640–1645.
Article4. Groop L. Genetics of the metabolic syndrome. Br J Nutr. 2000; 83 Suppl 1:S39–S48.
Article5. Edwardson CL, Gorely T, Davies MJ, Gray LJ, Khunti K, Wilmot EG, et al. Association of sedentary behaviour with metabolic syndrome: a meta-analysis. PLoS One. 2012; 7:e34916.
Article6. Xi B, He D, Zhang M, Xue J, Zhou D. Short sleep duration predicts risk of metabolic syndrome: a systematic review and meta-analysis. Sleep Med Rev. 2014; 18:293–297.
Article7. Vancampfort D, Correll CU, Wampers M, Sienaert P, Mitchell AJ, De Herdt A, et al. Metabolic syndrome and metabolic abnormalities in patients with major depressive disorder: a meta-analysis of prevalences and moderating variables. Psychol Med. 2014; 44:2017–2028.
Article8. Sun K, Ren M, Liu D, Wang C, Yang C, Yan L. Alcohol consumption and risk of metabolic syndrome: a meta-analysis of prospective studies. Clin Nutr. 2014; 33:596–602.
Article9. Simmons RK, Alberti KG, Gale EA, Colagiuri S, Tuomilehto J, Qiao Q, et al. The metabolic syndrome: useful concept or clinical tool? Report of a WHO Expert Consultation. Diabetologia. 2010; 53:600–605.
Article10. Pérez-Martínez P, Mikhailidis DP, Athyros VG, Bullo M, Couture P, Covas MI, et al. Lifestyle recommendations for the prevention and management of metabolic syndrome: an international panel recommendation. Nutr Rev. 2017; 75:307–326.
Article11. Lakka TA, Laaksonen DE. Physical activity in prevention and treatment of the metabolic syndrome. Appl Physiol Nutr Metab. 2007; 32:76–88.
Article12. Semlitsch T, Jeitler K, Hemkens LG, Horvath K, Nagele E, Schuermann C, et al. Increasing physical activity for the treatment of hypertension: a systematic review and meta-analysis. Sports Med. 2013; 43:1009–1023.
Article13. Piercy KL, Troiano RP, Ballard RM, Carlson SA, Fulton JE, Galuska DA, et al. The physical activity guidelines for Americans. JAMA. 2018; 320:2020–2028.
Article14. Arem H, Moore SC, Patel A, Hartge P, Berrington de Gonzalez A, Visvanathan K, et al. Leisure time physical activity and mortality: a detailed pooled analysis of the dose-response relationship. JAMA Intern Med. 2015; 175:959–967.15. Huh JH, Kang DR, Jang JY, Shin JH, Kim JY, Choi S, et al. Metabolic syndrome epidemic among Korean adults: Korean survey of Cardiometabolic Syndrome (2018). Atherosclerosis. 2018; 277:47–52.
Article16. Vinluan CM, Zreikat HH, Levy JR, Cheang KI. Comparison of different metabolic syndrome definitions and risks of incident cardiovascular events in the elderly. Metabolism. 2012; 61:302–309.
Article17. Huh JH, Yadav D, Kim JS, Son JW, Choi E, Kim SH, et al. An association of metabolic syndrome and chronic kidney disease from a 10-year prospective cohort study. Metabolism. 2017; 67:54–61.
Article18. Kim Y, Han BG. KoGES group. Cohort profile: the Korean Genome and Epidemiology Study (KoGES) consortium. Int J Epidemiol. 2017; 46:e20.
Article19. Lee SY, Park HS, Kim DJ, Han JH, Kim SM, Cho GJ, et al. Appropriate waist circumference cutoff points for central obesity in Korean adults. Diabetes Res Clin Pract. 2007; 75:72–80.
Article20. Ainsworth BE, Haskell WL, Leon AS, Jacobs DR Jr, Montoye HJ, Sallis JF, et al. Compendium of Physical Activities: classification of energy costs of human physical activities. Med Sci Sports Exerc. 1993; 25:71–80.
Article21. Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, et al. Compendium of Physical Activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000; 32:9 Suppl. S498–S504.
Article22. 2018 Physical Activity Guidelines Advisory Committee. 2018 Physical Activity Guidelines Advisory Committee scientific report. Washington, DC: U.S. Department of Health and Human Services;2018. p. F2–F33.23. R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria [Computer software]. 2018. Available at: http://www.R-project.org/.24. The jamovi project. jamovi (Version 1.2) [Computer software]. 2019. Available at https://www.jamovi.org.25. Centers for Disease Control and Prevention. National diabetes statistics report, 2017. Atlanta (GA): Centers for Disease Control and Prevention, US Dept of Health and Human Services;2017.26. International Diabetes Federation. The IDF consensus worldwide definition of the metabolic syndrome. Brussels: International Diabetes Federation;2006.27. Mozumdar A, Liguori G. Persistent increase of prevalence of metabolic syndrome among US adults: NHANES III to NHANES 1999–2006. Diabetes Care. 2011; 34:216–219.
Article28. Paffenbarger RS Jr, Hyde RT, Wing AL, Hsieh CC. Physical activity, all-cause mortality, and longevity of college alumni. N Engl J Med. 1986; 314:605–613.
Article29. Kujala UM, Kaprio J, Sarna S, Koskenvuo M. Relationship of leisure-time physical activity and mortality: the Finnish twin cohort. JAMA. 1998; 279:440–444.
Article30. Ford ES, Kohl HW 3rd, Mokdad AH, Ajani UA. Sedentary behavior, physical activity, and the metabolic syndrome among U.S. adults. Obes Res. 2005; 13:608–614.
Article31. Rennie KL, McCarthy N, Yazdgerdi S, Marmot M, Brunner E. Association of the metabolic syndrome with both vigorous and moderate physical activity. Int J Epidemiol. 2003; 32:600–606.
Article32. He D, Xi B, Xue J, Huai P, Zhang M, Li J. Association between leisure time physical activity and metabolic syndrome: a meta-analysis of prospective cohort studies. Endocrine. 2014; 46:231–240.
Article33. Li CL, Lin JD, Lee SJ, Tseng RF. Associations between the metabolic syndrome and its components, watching television and physical activity. Public Health. 2007; 121:83–91.
Article34. Salonen MK, Wasenius N, Kajantie E, Lano A, Lahti J, Heinonen K, et al. Physical activity, body composition and metabolic syndrome in young adults. PLoS One. 2015; 10:e0126737.
Article35. Xiao J, Shen C, Chu MJ, Gao YX, Xu GF, Huang JP, et al. Physical activity and sedentary behavior associated with components of metabolic syndrome among people in rural China. PLoS One. 2016; 11:e0147062.
Article36. Bertrais S, Beyeme-Ondoua JP, Czernichow S, Galan P, Hercberg S, Oppert JM. Sedentary behaviors, physical activity, and metabolic syndrome in middle-aged French subjects. Obes Res. 2005; 13:936–944.
Article37. Dunstan DW, Salmon J, Owen N, Armstrong T, Zimmet PZ, Welborn TA, et al. Associations of TV viewing and physical activity with the metabolic syndrome in Australian adults. Diabetologia. 2005; 48:2254–2261.
Article38. Kim J, Tanabe K, Yokoyama N, Zempo H, Kuno S. Association between physical activity and metabolic syndrome in middle-aged Japanese: a cross-sectional study. BMC Public Health. 2011; 11:624.
Article39. Diaz KM, Booth JN 3rd, Seals SR, Abdalla M, Dubbert PM, Sims M, et al. Physical activity and incident hypertension in African Americans: the Jackson Heart Study. Hypertension. 2017; 69:421–427.
Article40. Lee YJ, Song S, Song Y. High-carbohydrate diets and food patterns and their associations with metabolic disease in the Korean population. Yonsei Med J. 2018; 59:834–842.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Relationship between Weekly Physical Activity Frequency and Metabolic Syndrome
- Construction of Leisure Physical Activity Model of Middle-Aged Women in Urban Area
- Relationship between Change in Physical Activity and Risk of Metabolic Syndrome: A Prospective Cohort Study
- Leisure time physical activity and its relationship to coronary risk factors in male workers
- Comparison of Leisure Activities of First-Year High School Students in Large Cities and Medium and Small Cities - Focusing on the Influence on Health Status -