J Korean Orthop Assoc.
2020 Feb;55(1):46-53. 10.4055/jkoa.2020.55.1.46.
Clinical Results of Lateral-Posterior Internal Fixation for the Treatment of Scapular Body Fractures
- Affiliations
-
- 1Department of Orthopedic Surgery, The Catholic University of Korea, Yeouido St. Mary's Hospital, Seoul, Korea. simba0415@catholic.ac.kr
- KMID: 2470768
- DOI: http://doi.org/10.4055/jkoa.2020.55.1.46
Abstract
- PURPOSE
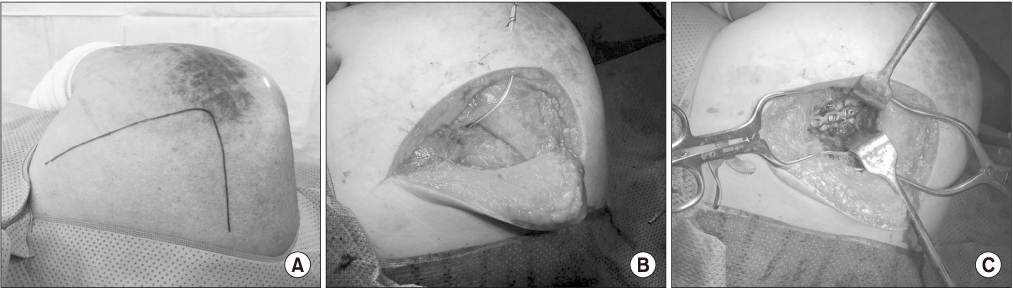
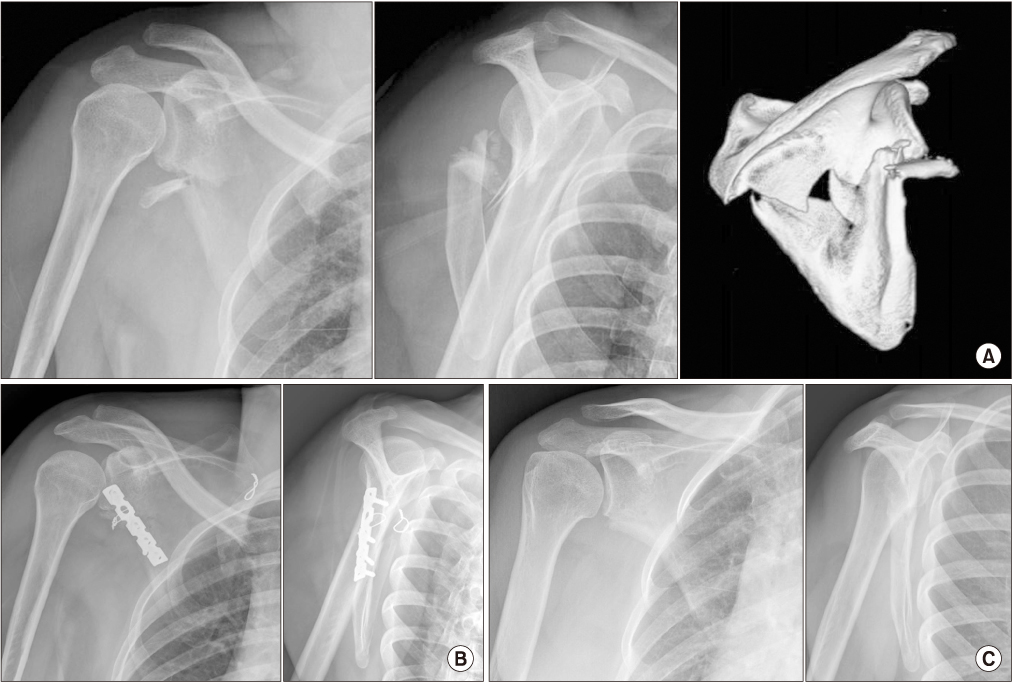
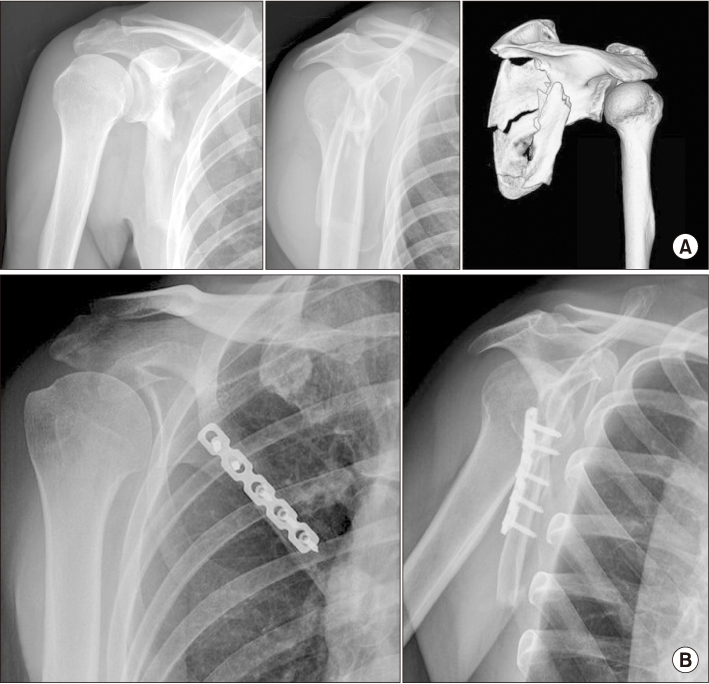
Scapular body fractures have generally been treated with non-surgical methods. This study reports the clinical and radiological outcomes after lateral-posterior internal fixation for treating displaced scapular body fractures.
MATERIALS AND METHODS
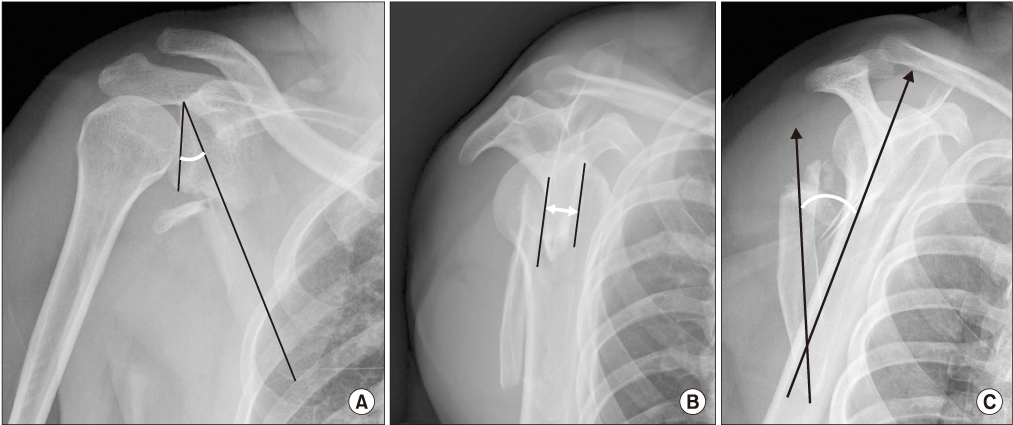
From March 2007 to May 2017, out of 40 patients who underwent internal fixation for scapular fractures, 13 cases of lateral plate fixation of a scapular body fracture were reviewed retrospectively. Preoperative and postoperative displacement, angulation and glenopolar angle (GPA) were measured. The range of shoulder motion, visual analogue scale (VAS), and disabilities of the arm, shoulder, and hand (DASH), and Constant score were assessed at the last follow-up.
RESULTS
The mean follow-up period was 17.7 months (range, 6-45 months). The mean preoperative GPA was 23.3°±3.96° (range, 17.8°-28.1°) and the postoperative GPA was 31.1°±4.75° (range, 22.5°-40.1°). Injury to the suprascapular nerve, nonunion, fracture redisplacement, metallic failure, or infection did not occur. At the last follow-up, the mean range of motion was 150.5°±19.3° in forward flexion, 146.6°±2.34° in lateral abduction, 66.6°±19.1° in external rotation, and 61.6°±18.9° in internal rotation. The VAS, DASH, and Constant scores were 1.7±1.3, 6.2±2.4, and 86±7.9 points, respectively.
CONCLUSION
A scapular body fracture with severe displacement, angulation and marked decreased GPA can be stabilized by lateralposterior plate fixation using the appropriate surgical technique with good functional and radiological results.
MeSH Terms
Figure
Reference
-
1. Nordqvist A, Petersson C. Fracture of the body, neck, or spine of the scapula. A long-term follow-up study. Clin Orthop Relat Res. 1992; (283):139–144.
Article2. You JW, Yoon HJ. Conservative treatment of scapular fractures. J Korean Soc Fract. 1994; 7:364–370.
Article3. Judet R. [Surgical treatment of scapular fractures]. Acta Orthop Belg. 1964; 30:673–678. French.4. Magerl F. [Osteosyntheses in the shoulder region. Pertubercular humeral fractures, scapular neck fractures]. Helv Chir Acta. 1974; 41:225–232. German.5. Hardegger FH, Simpson LA, Weber BG. The operative treatment of scapular fractures. J Bone Joint Surg Br. 1984; 66:725–731.
Article6. Shim DM, Kim JW, Kweon SH, Jeung UO, Lee JM. Surgical treatment of scapular fracture using by plate fixation: 4 cases report. J Korean Fract Soc. 2006; 19:381–387.
Article7. Cole PA, Gauger EM, Schroder LK. Management of scapular fractures. J Am Acad Orthop Surg. 2012; 20:130–141.
Article8. Chadwick EK, van Noort A, van der Helm FC. Biomechanical analysis of scapular neck malunion--a simulation study. Clin Biomech (Bristol, Avon). 2004; 19:906–912.
Article9. Armstrong CP, Van der Spuy J. The fractured scapula: importance and management based on a series of 62 patients. Injury. 1984; 15:324–329.
Article10. Goss TP. Fractures of the glenoid cavity. J Bone Joint Surg Am. 1992; 74:299–305.
Article11. Wilber MC, Evans EB. Fractures of the scapula. An analysis of forty cases and a review of the literature. J Bone Joint Surg Am. 1977; 59:358–362.
Article12. Kibler WB, McMullen J. Scapular dyskinesis and its relation to shoulder pain. J Am Acad Orthop Surg. 2003; 11:142–151.
Article13. Ada JR, Miller ME. Scapular fractures. Analysis of 113 cases. Clin Orthop Relat Res. 1991; (269):174–180.14. Bartoníček J, Frič V. Scapular body fractures: results of operative treatment. Int Orthop. 2011; 35:747–753.
Article15. Jones CB, Sietsema DL. Analysis of operative versus nonoperative treatment of displaced scapular fractures. Clin Orthop Relat Res. 2011; 469:3379–3389.
Article16. Anavian J, Conflitti JM, Khanna G, Guthrie ST, Cole PA. A reliable radiographic measurement technique for extra-articular scapular fractures. Clin Orthop Relat Res. 2011; 469:3371–3378.
Article17. Wijdicks CA, Anavian J, Hill BW, Armitage BM, Vang S, Cole PA. The assessment of scapular radiographs: analysis of anteroposterior radiographs of the shoulder and the effect of rotational offset on the glenopolar angle. Bone Joint J. 2013; 95-B:1114–1120.18. Bozkurt M, Can F, Kirdemir V, Erden Z, Demirkale I, Başbozkurt M. Conservative treatment of scapular neck fracture: the effect of stability and glenopolar angle on clinical outcome. Injury. 2005; 36:1176–1181.
Article19. Romero J, Schai P, Imhoff AB. Scapular neck fracture: the influence of permanent malalignment of the glenoid neck on clinical outcome. Arch Orthop Trauma Surg. 2001; 121:313–316.20. Morey VM, Chua KHZ, Ng ZD, Tan HMB, Kumar VP. Management of the floating shoulder: does the glenopolar angle influence outcomes? A systematic review. Orthop Traumatol Surg Res. 2018; 104:53–58.
Article21. Kim KC, Rhee KJ, Shin HD, Yang JY. Can the glenopolar angle be used to predict outcome and treatment of the floating shoulder? J Trauma. 2008; 64:174–178.
Article22. Izadpanah K, Jaeger M, Maier D, Kubosch D, Hammer TO, Südkamp NP. The floating shoulder—clinical and radiological results after intramedullary stabilization of the clavicle in cases with minor displacement of the scapular neck fracture. J Trauma Acute Care Surg. 2012; 72:E8–E13.
Article23. Noguchi T, Mautner JF, Duncan SFM. Dorsal plate fixation of scapular fracture. J Hand Surg Am. 2017; 42:843.e1–843.e5.
Article24. Ao R, Yu B, Zhu Y, Jiang X, Shi J, Zhou J. Single lateral versus medial and lateral plates for treating displaced scapular body fractures: a retrospective comparative study. J Shoulder Elbow Surg. 2018; 27:231–236.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Management of Extra-articular Scapular Fractures: A Narrative Review and Proposal of a Treatment Algorithm
- The Posterior Plate for Distal Fibular Fixation
- Surgical Treatment of Scapular Fracture using by Plate Fixation: 4 Cases Report
- Surgical Treatment of the Fracture of the Scapular Body
- Odontoid Process Fracture Treated by Anterior Odontoid Screw Fixation