Healthc Inform Res.
2020 Jan;26(1):50-60. 10.4258/hir.2020.26.1.50.
Immediate Effects and Acceptability of an Application-Based Stretching Exercise Incorporating Deep Slow Breathing for Neck Pain Self-management
- Affiliations
-
- 1Research Center in Back, Neck, Other Joint Pain and Human Performance (BNOJPH), Khon Kaen University, Khon Kaen, Thailand. orawan@kku.ac.th
- 2Faculty of Associated Medical Sciences, School of Physical Therapy, Khon Kaen University, Khon Kaen, Thailand.
- KMID: 2469400
- DOI: http://doi.org/10.4258/hir.2020.26.1.50
Abstract
OBJECTIVES
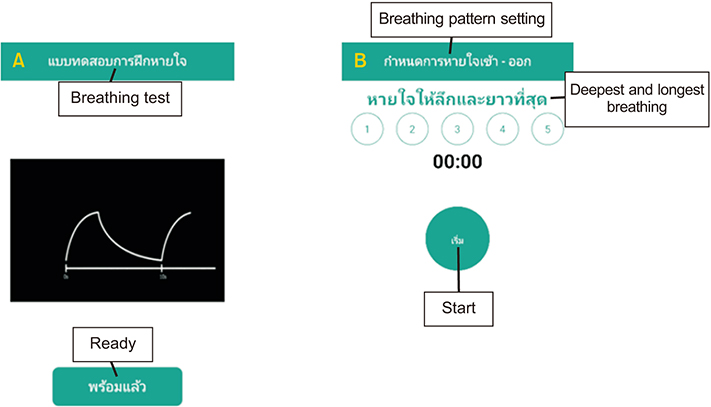
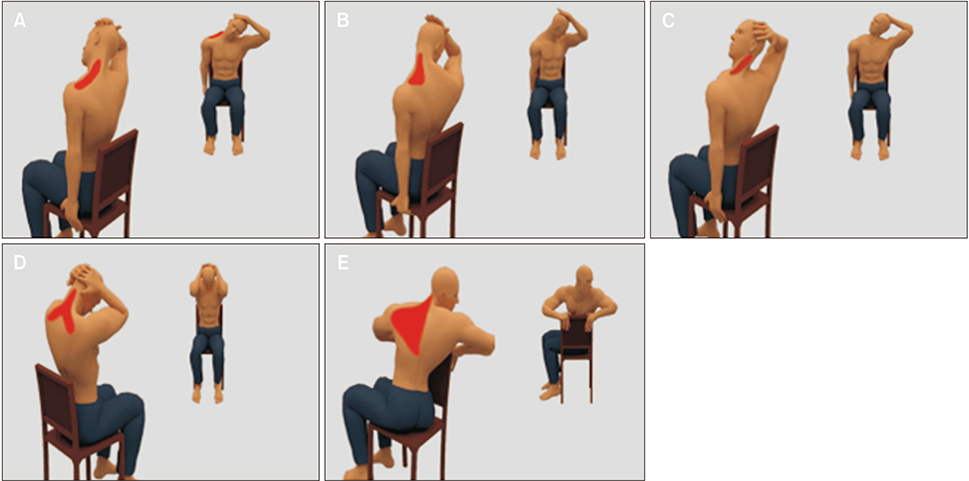
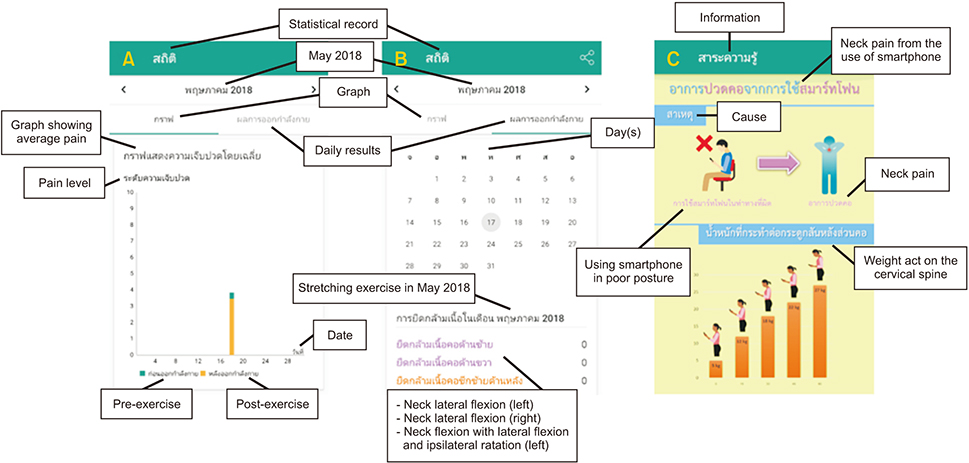
This study evaluated the immediate effects and acceptability of a smartphone application named NeckProtector to promote neck pain self-management through stretching incorporating deep slow breathing, among smartphone users with neck pain.
METHODS
One-hundred participants were recruited in the study. Participants were divided into two groups by block randomized allocation. The researchers gave the NeckProtector application to all participants for acceptability testing by navigation of the application for 20-30 minutes. Next, the treatment group (n = 50) conducted the exercise program via smartphone application for 15-20 minutes, while the control group (n = 50) rested for 20 minutes. Evaluations were performed at baseline and after intervention for pain intensity, muscle tension, pressure pain threshold (PPT), and cervical range of motion (CROM). Quantitative and qualitative feedback was then obtained by an acceptability survey and open-ended questionnaires.
RESULTS
The immediate effects showed statistically significant improvements in pain intensity, muscle tension, PPT, and CROM in the treatment group in comparison to the control group. Participants reported a high level of acceptability through ratings on a Likert scale. The qualitative questionnaires received positive responses that the application was easy to use and the exercise program was useful to cope with neck pain.
CONCLUSIONS
NeckProtector can be an alternative treatment for neck pain self-management via smartphone application among smartphone users with neck pain. Further studies should examine the long-term effectiveness (Clinical trials registry: TCTR20160523001).
Keyword
MeSH Terms
Figure
Reference
-
1. Sarwar M, Soomro TR. Impact of smartphone's on society. Eur J Sci Res. 2013; 98(2):216–226.2. Statista. Number of smartphone users in Thailand from 2013 to 2021 [Internet]. New York (NY): Statista;2017. cited at 2020 Jan 7. Available from: https://www.statista.com/statistics/467191/forecast-of-smartphone-users-in-thailand.3. Poushter J. Smartphone ownership and Internet usage continues to climb in emerging economies [Internet]. Washington (DC): Pew Research Center;2016. cited at 2020 Jan 7. Available from: http://www.pewglobal.org/2016/02/22/smartphone-ownership-and-internet-usage-continues-to-climb-in-emerging-economies/.4. Kim SY, Koo SJ. Effect of duration of smartphone use on muscle fatigue and pain caused by forward head posture in adults. J Phys Ther Sci. 2016; 28(6):1669–1672.
Article5. Berolo S, Wells RP, Amick BC 3rd. Musculoskeletal symptoms among mobile hand-held device users and their relationship to device use: a preliminary study in a Canadian university population. Appl Ergon. 2011; 42(2):371–378.
Article6. Namwongsa S, Puntumetakul R, Swangnetr M. Prevalence of musculoskeletal disorders of smartphone users in Khon Kaen University students, Thailand. In : Proceedings of the 2nd Thailand National Ergonomics Conference; 2017 Dec 20-22; Bangkok, Thailand.7. Lee S, Kang H, Shin G. Head flexion angle while using a smartphone. Ergonomics. 2015; 58(2):220–226.
Article8. Gold JE, Driban JB, Thomas N, Chakravarty T, Channell V, Komaroff E. Postures, typing strategies, and gender differences in mobile device usage: an observational study. Appl Ergon. 2012; 43(2):408–412.
Article9. Kang JH, Park RY, Lee SJ, Kim JY, Yoon SR, Jung KI. The effect of the forward head posture on postural balance in long time computer based worker. Ann Rehabil Med. 2012; 36(1):98–104.
Article10. Szeto GP, Straker LM, O'Sullivan PB. Neck-shoulder muscle activity in general and task-specific resting postures of symptomatic computer users with chronic neck pain. Man Ther. 2009; 14(3):338–345.
Article11. Bonney RA, Corlett EN. Head posture and loading of the cervical spine. Appl Ergon. 2002; 33(5):415–417.
Article12. Lee S, Lee D, Park J. Effect of the cervical flexion angle during smart phone use on muscle fatigue of the cervical erector spinae and upper trapezius. J Phys Ther Sci. 2015; 27(6):1847–1849.
Article13. Hansraj KK. Assessment of stresses in the cervical spine caused by posture and position of the head. Surg Technol Int. 2014; 25:277–279.14. Kong YS, Kim YM, Shim JM. The effect of modified cervical exercise on smartphone users with forward head posture. J Phys Ther Sci. 2017; 29(2):328–331.
Article15. Litman L, Rosen Z, Spierer D, Weinberger-Litman S, Goldschein A, Robinson J. Mobile exercise apps and increased leisure time exercise activity: a moderated mediation analysis of the role of self-efficacy and barriers. J Med Internet Res. 2015; 17(8):e195.
Article16. Christiansen S, Gupta A. Can mobile technology improve treatment of chronic pain? Pain Med. 2014; 15(8):1434–1435.
Article17. Lauche R, Stumpe C, Fehr J, Cramer H, Cheng YW, Wayne PM, et al. The effects of Tai Chi and neck exercises in the treatment of chronic nonspecific neck pain: a randomized controlled trial. J Pain. 2016; 17(9):1013–1027.
Article18. Kim SD. Effects of yoga on chronic neck pain: a systematic review of randomized controlled trials. J Phys Ther Sci. 2016; 28(7):2171–2174.
Article19. Dou K, Yu P, Deng N, Liu F, Guan Y, Li Z, et al. Patients' acceptance of smartphone health technology for chronic disease management: a theoretical model and empirical test. JMIR Mhealth Uhealth. 2017; 5(12):e177.
Article20. Wongwilairat K, Buranruk O, Eungpinichpong W, Puntumetakul R, Kantharadussadee-Triamchaisri S. Muscle stretching with deep and slow breathing patterns: a pilot study for therapeutic development. J Complement Integr Med. 2018; 16(2):20170167.
Article21. Morone NE, Lynch CS, Greco CM, Tindle HA, Weiner DK. “I felt like a new person.” the effects of mindfulness meditation on older adults with chronic pain: qualitative narrative analysis of diary entries. J Pain. 2008; 9(9):841–848.
Article22. Bijur PE, Silver W, Gallagher EJ. Reliability of the visual analog scale for measurement of acute pain. Acad Emerg Med. 2001; 8(12):1153–1157.
Article23. Kinser AM, Sands WA, Stone MH. Reliability and validity of a pressure algometer. J Strength Cond Res. 2009; 23(1):312–314.
Article24. Fletcher JP, Bandy WD. Intrarater reliability of CROM measurement of cervical spine active range of motion in persons with and without neck pain. J Orthop Sports Phys Ther. 2008; 38(10):640–645.
Article25. Brooke J. SUS: a quick and dirty usability scale. Usability Eval Ind. 1996; 189(194):4–7.26. Lee M, Lee SH, Kim T, Yoo HJ, Kim SH, Suh DW, et al. Feasibility of a smartphone-based exercise program for office workers with neck pain: an individualized approach using a self-classification algorithm. Arch Phys Med Rehabil. 2017; 98(1):80–87.
Article27. Busch V, Magerl W, Kern U, Haas J, Hajak G, Eichhammer P. The effect of deep and slow breathing on pain perception, autonomic activity, and mood processing: an experimental study. Pain Med. 2012; 13(2):215–228.
Article28. Berry RR, Lai B. The emerging role of technology in cognitive–behavioral therapy for anxious youth: a review. J Ration Emot Cogn Behav Ther. 2014; 32(1):57–66.
Article29. Palermo TM, Valenzuela D, Stork PP. A randomized trial of electronic versus paper pain diaries in children: impact on compliance, accuracy, and acceptability. Pain. 2004; 107(3):213–219.
Article30. Jamison RN, Raymond SA, Levine JG, Slawsby EA, Nedeljkovic SS, Katz NP. Electronic diaries for monitoring chronic pain: 1-year validation study. Pain. 2001; 91(3):277–285.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Changes in the Pressure Threshold of Myofascial Trigger Points of the Shoulder Girdle Muscles Following Stretching Exercise
- Effects of Stretching Exercise on the Head Speed of Golf Club and Driving Distance
- Effectiveness of Deep Breathing Exercise for Postoperative Pulmonary Complications Prevention: A Systematic Review
- Effects of the Neck Stabilization Exercises with Vibratory Stimulation on the Neck Disability Index and Thickness of Deep Neck Flexor in Neck Pain Patient
- The Effects of Stretching and Strengthening Exercise on the Pain, Pelvic Tilt, Functional Disability Index, and Balance Ability of Patients with Chronic Lower Back Pain