J Korean Fract Soc.
2019 Oct;32(4):196-203. 10.12671/jkfs.2019.32.4.196.
Simulation for Reduction of Transverse Acetabular Fractures in Sawbones Models
- Affiliations
-
- 1Department of Orthopaedic Surgery, CHA Bundang Medical Center, CHA University, Seongnam, Korea.
- 2Department of Orthopaedic Surgery, Denver Health Medical Center, University of Colorado, Denver, CO, USA.
- 3Department of Orthopaedic Surgery, Hallym University Sacred Heart Hospital, College of Medicine, Hallym University, Anyang, Korea.
- 4Department of Orthopaedic Surgery, Hallym University Kangnam Sacred Heart Hospital, College of Medicine, Hallym University, Seoul, Korea. hwangjihyo7309@gmail.com
- KMID: 2468682
- DOI: http://doi.org/10.12671/jkfs.2019.32.4.196
Abstract
- PURPOSE
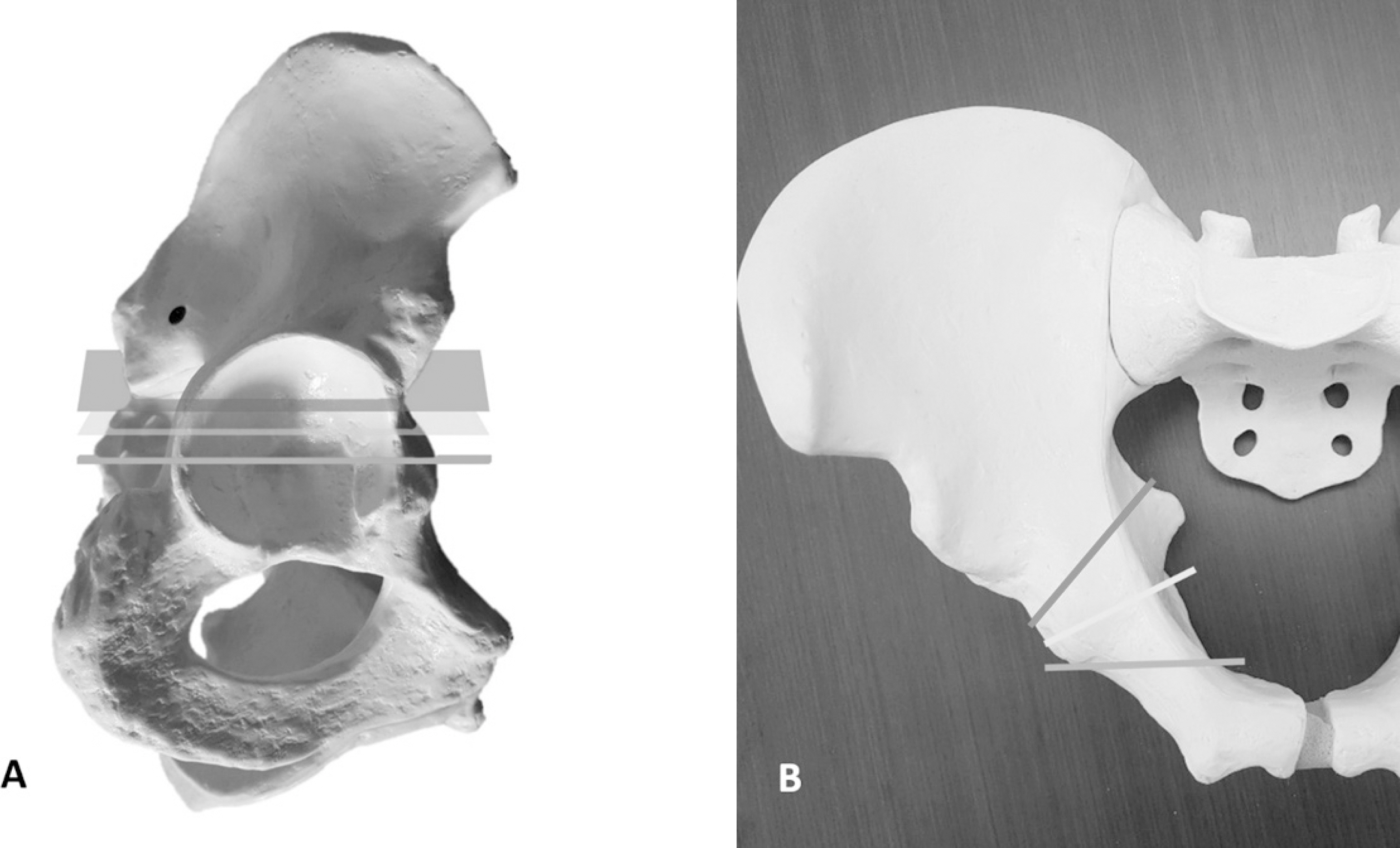
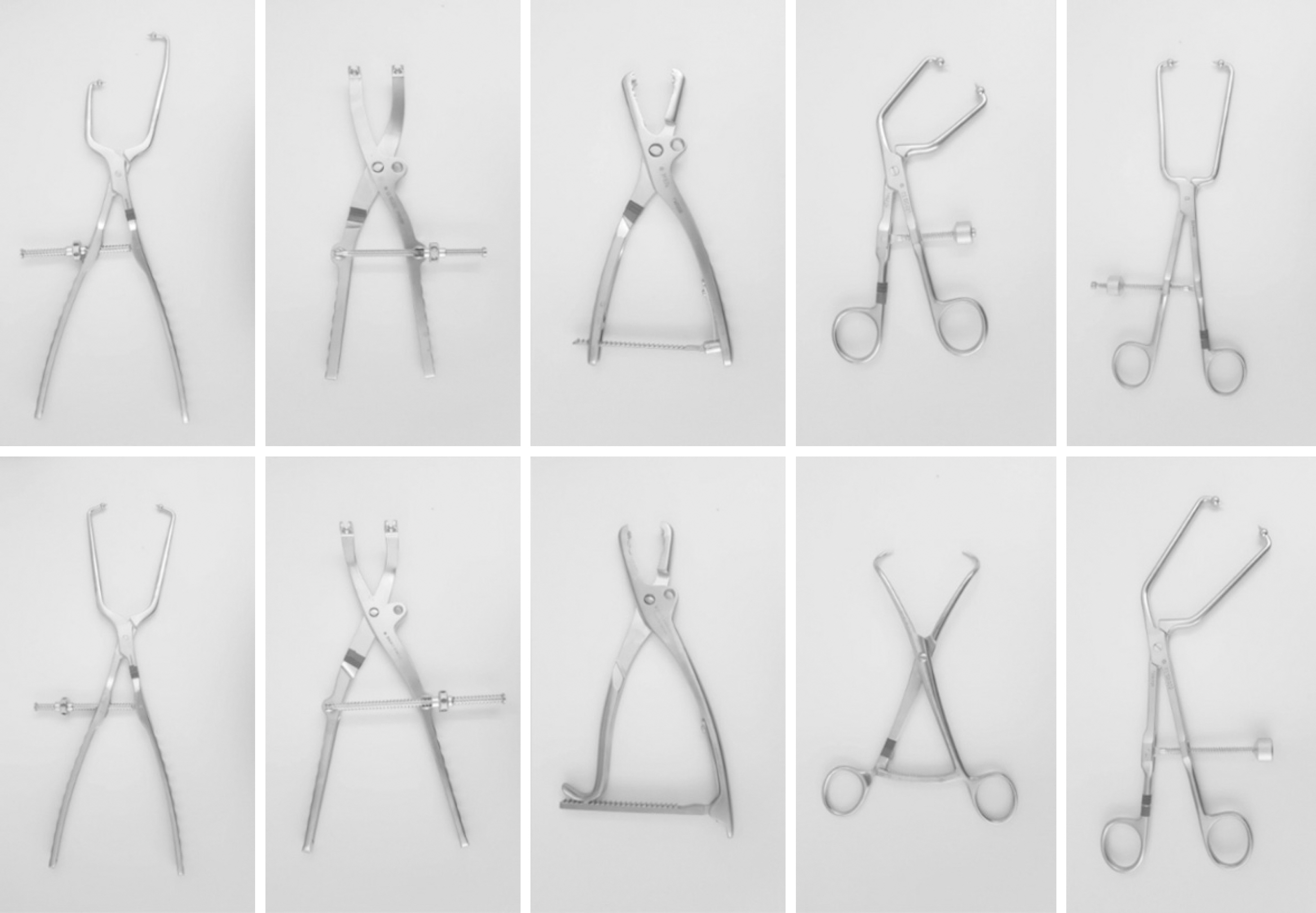
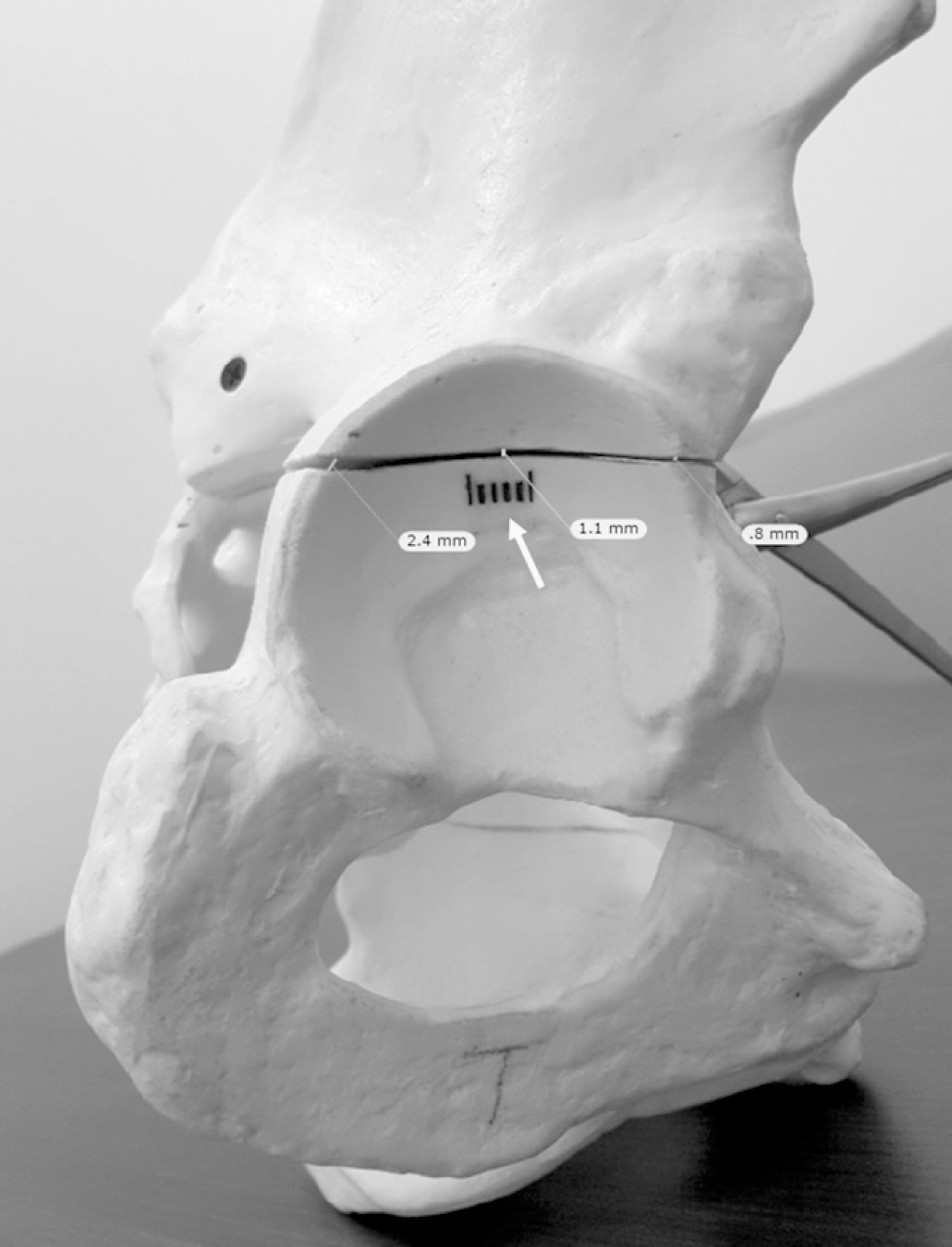
The transversely oriented fracture lines are very difficult to reduce during operations, even after clear exposure of the fracture site, in acetabular fractures. The purpose of this study is to verify the quality of reduction between the different subtypes (transtectal, juxtatectal, and infratectal) of transverse fractures. This study also determined the proper type of clamps to use and the proper zone for achieving accurate reductions in Sawbones models.
MATERIALS AND METHODS
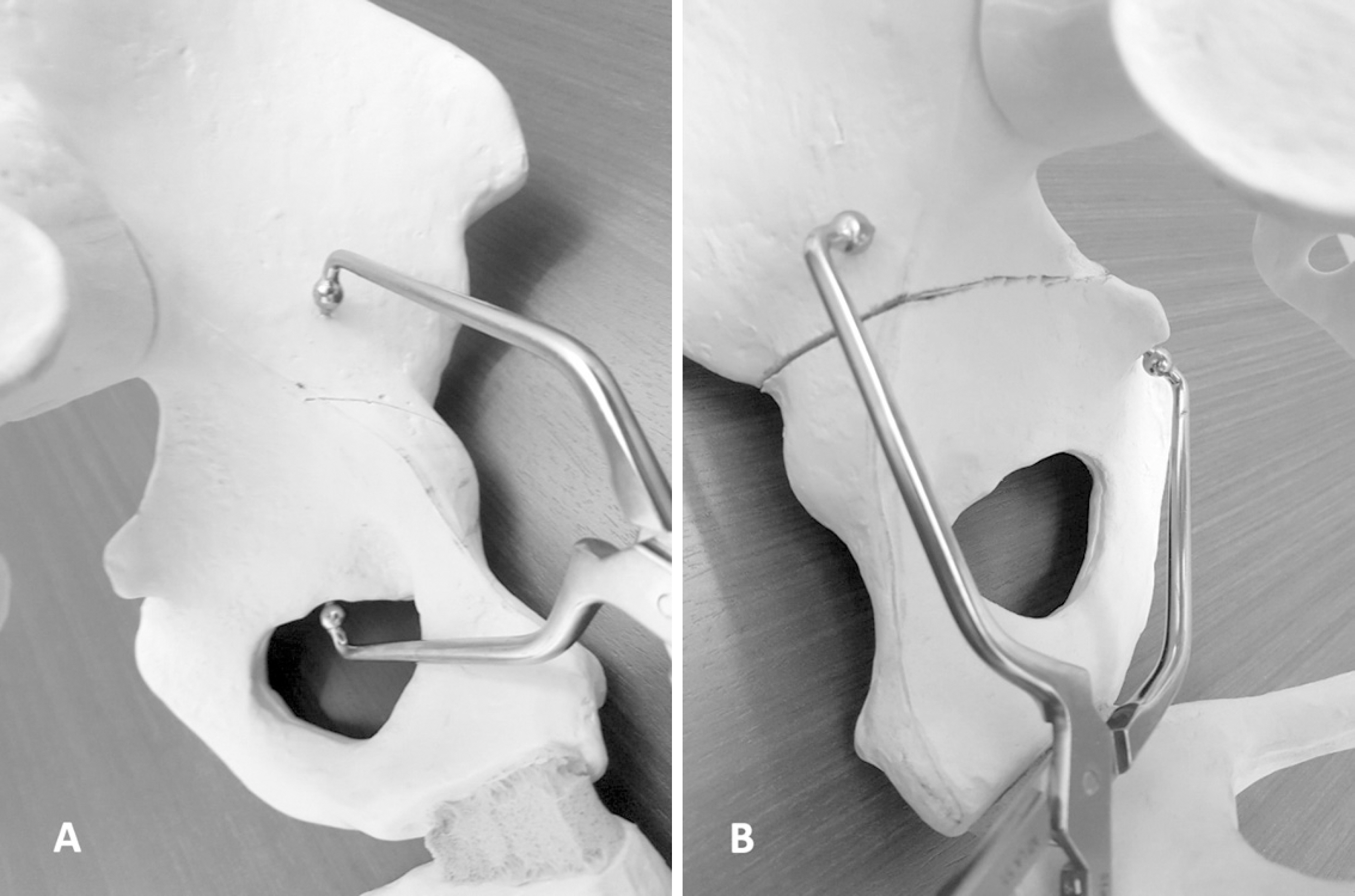
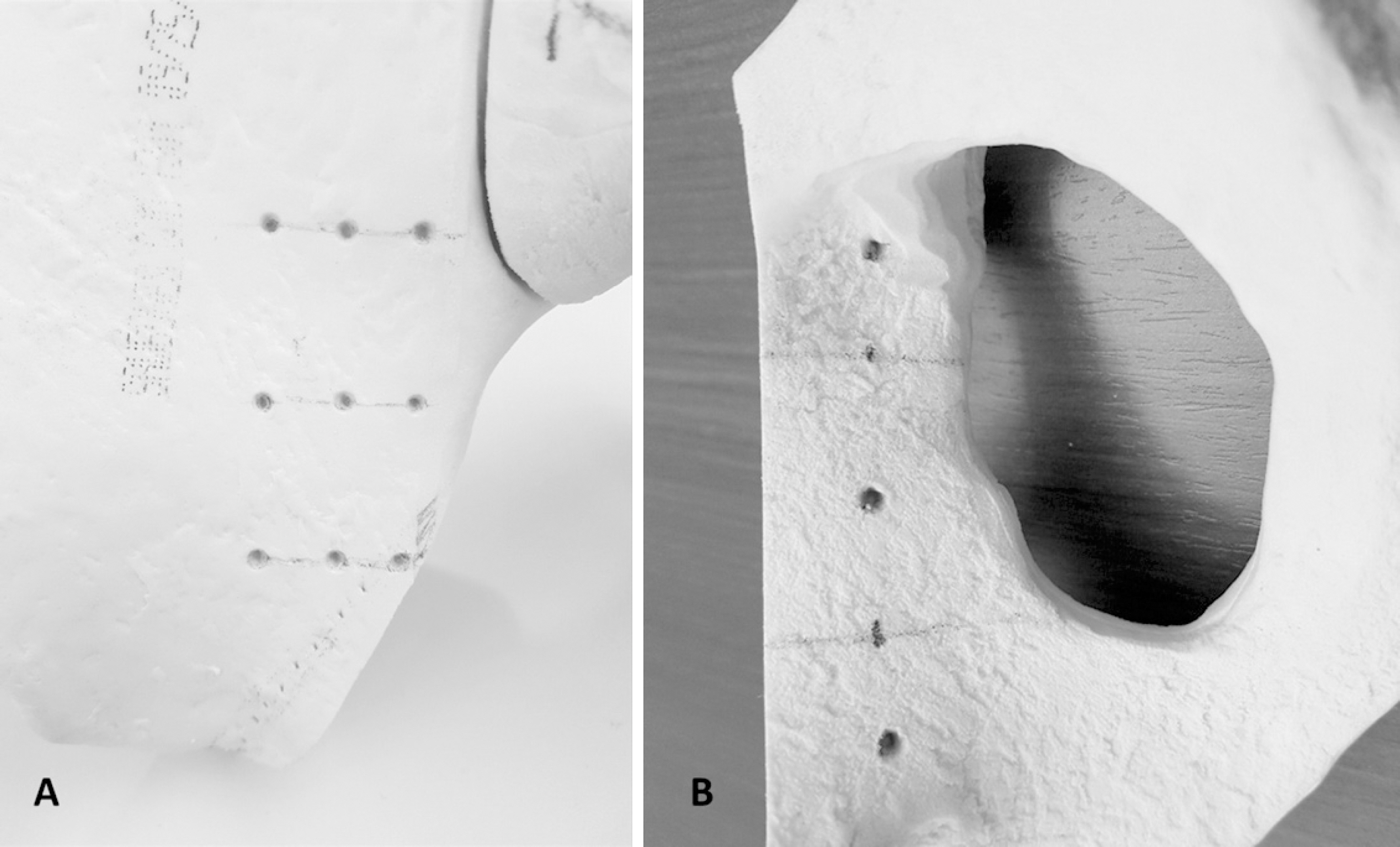
Six fractures in 3 different subtypes of transverse fractures were artificially created. Ten different reduction clamps were applied for reduction of the fractures. Twelve holes around the fracture were drilled for the maintenance of the clamps. The fracture displacements were measured at the extra-articular area and the intra-articular joint portion. The pictures of the intra-articular fracture displacements were taken by a camera and these were uploaded and analyzed by the TraumaCad® computer program (Brainlab).
RESULTS
The reduction quality was poor in order of transtectal, juxtatectal and infratectal. The intraarticular opening was more prominent in the transtectal subtype. The safe zone, when giving consideration of the neurovascular bundles, was a quadrilateral surface of the ilium. Drill holes are useful for maintenance of the reduction clamps. Reduction clamps with points (Weber clamp) were the best for maintenance and accurate reduction. Regarding the concerns of placement of clamps, the middle to posterior combination was the best. The upper hole among the posterior holes in the ilium was the most likely to well reduce the intra-articular opening.
CONCLUSION
Transtectal was the more complicated subtype in the aspect of reduction quality. The Weber type reduction clamp was the best for reduction by centrally located holes in the quadrilateral surface and posteriorly located iliac holes in transverse acetabular fractures. The upper hole, among the posterior holes in the ilium, was the best for reduction of the fracture displacements in the intraarticular portion of acetabulum.
Figure
Reference
-
References
1. Fan L, Jin YJ, He L, Lü Z, Fan HH. [Modified Stoppa approach in treatment of pelvic and acetabular fractures]. Zhongguo Gu Shang. 25:810–812. 2012; Chinese.2. Letournel E. Acetabulum fractures: classification and management. Clin Orthop Relat Res. 151:81–106. 1980.
Article3. Hak DJ, Hamel AJ, Bay BK, Sharkey NA, Olson SA. Consequences of transverse acetabular fracture malreduction on load transmission across the hip joint. J Orthop Trauma. 12:90–100. 1998.
Article4. Thomas KA, Vrahas MS, Noble JW Jr, Bearden CM, Reid JS. Evaluation of hip stability after simulated transverse acetabular fractures. Clin Orthop Relat Res. 340:244–256. 1997.
Article5. Malkani AL, Voor MJ, Rennirt G, Helfet D, Pedersen D, Brown T. Increased peak contact stress after incongruent reduction of transverse acetabular fractures: a cadaveric model. J Trauma. 51:704–709. 2001.
Article6. Chiboub H, Lamrani O, Kharmaz M, el Yazidi A, Wahbi S, el Manouar M. [Transverse and T fractures with fracture of the posterior wall of the acetabulum. Results of orthopedic and surgical treatment. Apropos of 52 cases]. Ann Chir. 52:913–917. 1998; French.7. Ziran NM, Johnson JL, Morgan SJ, Smith WR. Femoral artery thrombosis after internal fixation of a transverse acetabular fracture in a patient with osteogenesis imperfecta type I. Patient Saf Surg. 2:1. 2008.
Article8. Lehmann W, Hoffmann M, Fensky F, et al. What is the frequency of nerve injuries associated with acetabular fractures? Clin Orthop Relat Res. 472:3395–3403. 2014.
Article9. Isaacson MJ, Taylor BC, French BG, Poka A. Treatment of acetabulum fractures through the modified Stoppa approach: strategies and outcomes. Clin Orthop Relat Res. 472:3345–3352. 2014.
Article10. Iqbal F, Uddin AA, Younus S, Zia OB, Khan N. Surgical outcomes of acute acetabular transverse fracture using ilioinguinal and Stoppa approach. J Acute Dis. 6:278–283. 2017.
Article11. Gross T, Jacob AL, Messmer P, Regazzoni P, Steinbrich W, Huegli RW. Transverse acetabular fracture: hybrid minimal access and percutaneous CT-navigated fixation. AJR Am J Roentgenol. 183:1000–1002. 2004.
Article12. Kistler BJ, Smithson IR, Cooper SA, et al. Are quadrilateral surface buttress plates comparable to traditional forms of transverse acetabular fracture fixation? Clin Orthop Relat Res. 472:3353–3361. 2014.
Article13. Liu H, Li L, Wu X, Xu H, Zhang R. [Biomechanical research of different internal fixations using locking reconstruction plate for acetabular transverse fracture]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 29:1084–1087. 2015; Chinese.14. Fahmy M, Abdel Karim M, Khaled SA, Abdelazeem AH, Elnahal WA, Elnahal A. Single versus double column fixation in transverse fractures of the acetabulum: a randomised controlled trial. Injury. 49:1291–1296. 2018.
Article15. Yildirim AO, Alemdaroglu KB, Yuksel HY, Öken ÖF, Ucaner A. Finite element analysis of the stability of transverse acetabular fractures in standing and sitting positions by different fixation options. Injury. 46(Suppl 2):S29–S35. 2015.
Article16. Shazar N, Brumback RJ, Novak VP, Belkoff SM. Biomechanical evaluation of transverse acetabular fracture fixation. Clin Orthop Relat Res. 352:215–222. 1998.
Article17. Ruggieri F, Zinghi GF, Montanari G, Benghi M. Transverse fractures of the acetabulum. Ital J Orthop Traumatol. 12:25–40. 1986.18. Øvre S, Madsen JE, Røise O. Transitional transverse acetabular fractures: differences between fractures with a large posterio-superior fragment and the inverse T-fracture–a report of 10 unusual cases. Acta Orthop. 76:803–808. 2005.
Article19. Oh CW, Kim PT, Park BC, et al. Results after operative treatment of transverse acetabular fractures. J Orthop Sci. 11:478–484. 2006.
Article20. Giordano V, do Amaral NP, Pallottino A, Pires e Albuquerque R, Franklin CE, Labronici PJ. Operative treatment of transverse acetabular fractures: is it really necessary to fix both columns? Int J Med Sci. 6:192–199. 2009.
Article21. Li XG, Tang TS, Sun JY. Results after surgical treatment of transtectal transverse acetabular fractures. Orthop Surg. 2:7–13. 2010.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Factors Influencing the Result of Transverse Acetabular Fractures
- Surgical Treatment of Displaced Acetabular Fractures
- Treatment of Acetabular Column Fractures with Limited Open Reduction and Screw Fixation
- Surgical Treatment of Displaced Acetabular Fractures - focused on Complications after open reduction -
- Single Percutaneous Retrograde Anterior Column Screw Fixation in a Minimally Displaced Transverse Acetabular Fracture - A Case Report -