Prog Med Phys.
2019 Dec;30(4):94-103. 10.14316/pmp.2019.30.4.94.
Volumetric-Modulated Arc Radiotherapy Using Knowledge-Based Planning: Application to Spine Stereotactic Body Radiotherapy
- Affiliations
-
- 1Department of Radiation Oncology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. bcho@amc.seoul.kr, coocoori@amc.seoul.kr
- 2Department of Radiation Oncology, Yeungnam University Medical Center, Daegu, Korea.
- KMID: 2468170
- DOI: http://doi.org/10.14316/pmp.2019.30.4.94
Abstract
- PURPOSE
To evaluate the clinical feasibility of knowledge-based planning (KBP) for volumetric-modulated arc radiotherapy (VMAT) in spine stereotactic body radiotherapy (SBRT).
METHODS
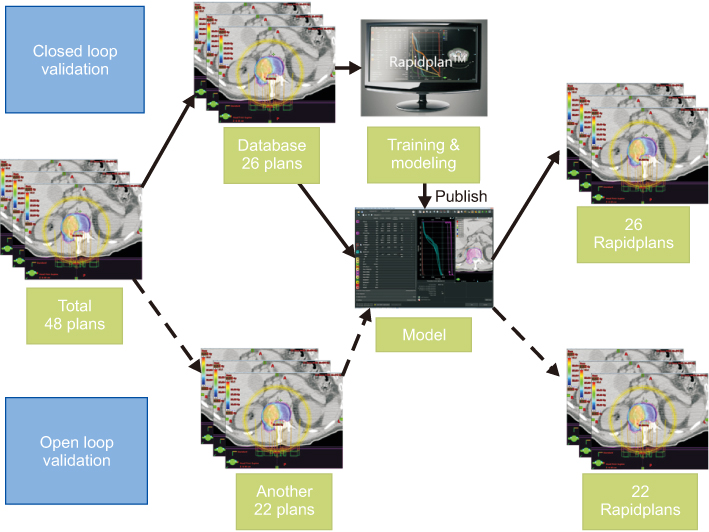
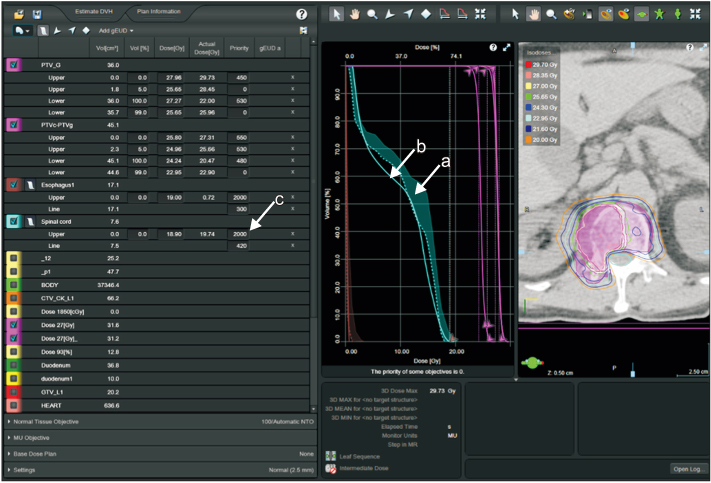
Forty-eight VMAT plans for spine SBRT was studied. Two planning target volumes (PTVs) were defined for simultaneous integrated boost: PTV for boost (PTV-B: 27 Gy/3fractions) and PTV elective (PTV-E: 24 Gy/3fractions). The expert VMAT plans were manually generated by experienced planners. Twenty-six plans were used to train the KBP model using Varian RapidPlan. With the trained KBP model each KBP plan was automatically generated by an individual with little experience and compared with the expert plan (closed-loop validation). Twenty-two plans that had not been used for KBP model training were also compared with the KBP results (open-loop validation).
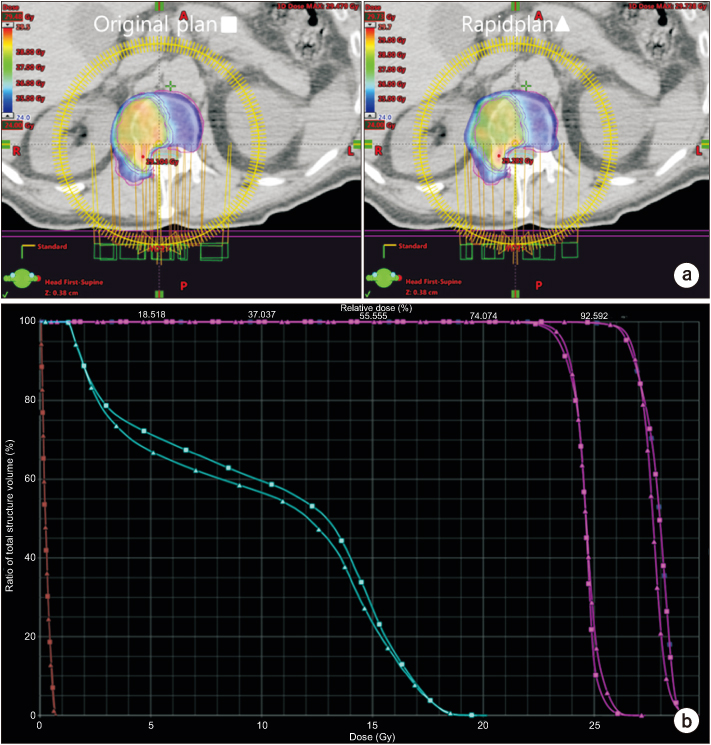
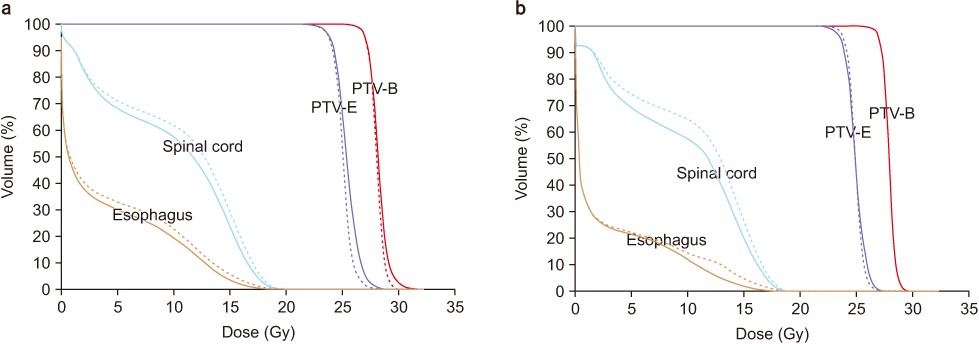
RESULTS
Although the minimal dose of PTV-B and PTV-E was lower and the maximal dose was higher than those of the expert plan, the difference was no larger than 0.7 Gy. In the closed-loop validation, D(1.2cc), D(0.35cc), and D(mean) of the spinal cord was decreased by 0.9 Gy, 0.6 Gy, and 0.9 Gy, respectively, in the KBP plans (P<0.05). In the open-loop validation, only D(mean) of the spinal cord was significantly decreased, by 0.5 Gy (P<0.05).
CONCLUSIONS
The dose coverage and uniformity for PTV was slightly worse in the KBP for spine SBRT while the dose to the spinal cord was reduced, but the differences were small. Thus, inexperienced planners could easily generate a clinically feasible plan for spine SBRT by using KBP.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Dosimetric Comparison of Noncoplanar and Coplanar Volumetric Modulated Arc Therapy Plans for Esophageal Cancer
So-Yeon Park
Prog Med Phys. 2020;31(4):179-188. doi: 10.14316/pmp.2020.31.4.179.
Reference
-
1. Chung HT, Lee B, Park E, Lu JJ, Xia P. Can all centers plan intensity-modulated radiotherapy (IMRT) effectively? An external audit of dosimetric comparisons between three-dimensional conformal radiotherapy and IMRT for adjuvant chemoradiation for gastric cancer. Int J Radiat Oncol Biol Phys. 2008; 71:1167–1174.
Article2. Nelms BE, Robinson G, Markham J, Velasco K, Boyd S, Narayan S, et al. Variation in external beam treatment plan quality: an inter-institutional study of planners and planning systems. Pract Radiat Oncol. 2012; 2:296–305.
Article3. Moore KL, Brame RS, Low DA, Mutic S. Quantitative metrics for assessing plan quality. Semin Radiat Oncol. 2012; 22:62–69.
Article4. Moore KL, Brame RS, Low DA, Mutic S. Experience-based quality control of clinical intensity-modulated radiotherapy planning. Int J Radiat Oncol Biol Phys. 2011; 81:545–551.
Article5. Yang Y, Ford EC, Wu B, Pinkawa M, van Triest B, Campbell P, et al. An overlap-volume-histogram based method for rectal dose prediction and automated treatment planning in the external beam prostate radiotherapy following hydrogel injection. Med Phys. 2013; 40:011709.
Article6. Zarepisheh M, Long T, Li N, Tian Z, Romeijn HE, Jia X, et al. A DVH-guided IMRT optimization algorithm for automatic treatment planning and adaptive radiotherapy replanning. Med Phys. 2014; 41:061711.
Article7. Yang Y, Xing L. Clinical knowledge-based inverse treatment planning. Phys Med Biol. 2004; 49:5101–5117.
Article8. Fogliata A, Wang PM, Belosi F, Clivio A, Nicolini G, Vanetti E, et al. Assessment of a model based optimization engine for volumetric modulated arc therapy for patients with advanced hepatocellular cancer. Radiat Oncol. 2014; 9:236.
Article9. Fogliata A, Belosi F, Clivio A, Navarria P, Nicolini G, Scorsetti M, et al. On the pre-clinical validation of a commercial model-based optimisation engine: application to volumetric modulated arc therapy for patients with lung or prostate cancer. Radiother Oncol. 2014; 113:385–391.
Article10. Kavanaugh JA, Holler S, DeWees TA, Robinson CG, Bradley JD, Iyengar P, et al. Multi-institutional validation of a knowledge-based planning model for patients enrolled in RTOG 0617: implications for plan quality controls in cooperative group trials. Pract Radiat Oncol. 2019; 9:e218–e227.
Article11. Campbell WG, Miften M, Olsen L, Stumpf P, Schefter T, Goodman KA, et al. Neural network dose models for knowledge-based planning in pancreatic SBRT. Med Phys. 2017; 44:6148–6158.
Article12. Fogliata A, Cozzi L, Reggiori G, Stravato A, Lobefalo F, Franzese C, et al. RapidPlan knowledge based planning: iterative learning process and model ability to steer planning strategies. Radiat Oncol. 2019; 14:187.
Article13. Agarawal JP, Swangsilpa T, van der Linden Y, Rades D, Jeremic B, Hoskin PJ. The role of external beam radiotherapy in the management of bone metastases. Clin Oncol (R Coll Radiol). 2006; 18:747–760.
Article14. Prasad D, Schiff D. Malignant spinal-cord compression. Lancet Oncol. 2005; 6:15–24.
Article15. Sahgal A, Ma L, Fowler J, Weinberg V, Gibbs I, Gerszten PC, et al. Impact of dose hot spots on spinal cord tolerance following stereotactic body radiotherapy: a generalized biological effective dose analysis. Technol Cancer Res Treat. 2012; 11:35–40.
Article16. Kirkpatrick JP, van der Kogel AJ, Schultheiss TE. Radiation dose-volume effects in the spinal cord. Int J Radiat Oncol Biol Phys. 2010; 76:3 Suppl. S42–S49.
Article17. Chawla S, Schell MC, Milano MT. Stereotactic body radiation for the spine: a review. Am J Clin Oncol. 2013; 36:630–636.18. Cox BW, Spratt DE, Lovelock M, Bilsky MH, Lis E, Ryu S, et al. International Spine Radiosurgery Consortium consensus guidelines for target volume definition in spinal stereotactic radiosurgery. Int J Radiat Oncol Biol Phys. 2012; 83:e597–e605.
Article19. Wu QJ, Yoo S, Kirkpatrick JP, Thongphiew D, Yin FF. Volumetric arc intensity-modulated therapy for spine body radiotherapy: comparison with static intensity-modulated treatment. Int J Radiat Oncol Biol Phys. 2009; 75:1596–1604.
Article20. Videtic GM, Hu C, Singh AK, Chang JY, Parker W, Olivier KR, et al. A randomized phase 2 study comparing 2 stereotactic body radiation therapy schedules for medically inoperable patients with stage I peripheral non-small cell lung cancer: NRG Oncology RTOG 0915 (NCCTG N0927). Int J Radiat Oncol Biol Phys. 2015; 93:757–764.
Article21. Yuan L, Ge Y, Lee WR, Yin FF, Kirkpatrick JP, Wu QJ. Quantitative analysis of the factors which affect the interpatient organ-at-risk dose sparing variation in IMRT plans. Med Phys. 2012; 39:6868–6878.
Article22. Wu B, McNutt T, Zahurak M, Simari P, Pang D, Taylor R, et al. Fully automated simultaneous integrated boosted-intensity modulated radiation therapy treatment planning is feasible for head-and-neck cancer: a prospective clinical study. Int J Radiat Oncol Biol Phys. 2012; 84:e647–e653.
Article23. Källman P, Agren A, Brahme A. Tumour and normal tissue responses to fractionated non-uniform dose delivery. Int J Radiat Biol. 1992; 62:249–262.
Article24. Miften MM, Das SK, Su M, Marks LB. Incorporation of functional imaging data in the evaluation of dose distributions using the generalized concept of equivalent uniform dose. Phys Med Biol. 2004; 49:1711–1721.
Article25. Wu Q, Mohan R, Niemierko A, Schmidt-Ullrich R. Optimization of intensity-modulated radiotherapy plans based on the equivalent uniform dose. Int J Radiat Oncol Biol Phys. 2002; 52:224–235.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Dosimetric Comparison of Three-Dimensional Conformal, Intensity-Modulated Radiotherapy, Volumetric Modulated Arc Therapy, and Dynamic Conformal Arc Therapy Techniques in Prophylactic Cranial Irradiation
- Evolution of Radiotherapy: High-precision Radiotherapy
- Sinonasal teratocarcinosarcoma treated with surgery followed by volumetric modulated radiotherapy: a case report with review of literature
- Comparison of IMRT and VMAT Techniques in Spine Stereotactic Radiosurgery with International Spine Radiosurgery Consortium Consensus Guidelines
- Optimization of Total Arc Degree for Stereotactic Radiotherapy by Using Integral Biologically Effective Dose and Irradiated Volume