J Clin Neurol.
2019 Oct;15(4):545-554. 10.3988/jcn.2019.15.4.545.
Long-Term Outcomes of Real-World Korean Patients with Atrial-Fibrillation-Related Stroke and Severely Decreased Ejection Fraction
- Affiliations
-
- 1Department of Neurology, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea.
- 2Department of Cardiology, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea.
- 3Department of Neurology, Korea University Anam Hospital, Korea University College of Medicine, Seoul, Korea.
- 4Department of Neurology, Korea University Guro Hospital, Korea University College of Medicine, Seoul, Korea.
- 5Department of Neurology, Mokdong Hospital, Ewha Womans University, College of Medicine, Seoul, Korea.
- 6Department of Neurology, Eunpyeong St. Mary's Hospital, The Catholic University of Korea, Seoul, Korea.
- 7Department of Neurology, Kyung Hee University College of Medicine, Seoul, Korea.
- 8Department of Neurology, Chung-Ang University College of Medicine, Chung-Ang University Hospital, Seoul, Korea.
- 9Department of Neurology, Myongji Hospital, Hanyang University College of Medicine, Goyang, Korea.
- 10Department of Neurology, Jeju National University, Jeju, Korea.
- 11Department of Neurology, Chonnam National University Hospital, Gwangju, Korea.
- 12Department of Neurology, Chonnam National University Hwasun Hospital, Hwasun, Korea.
- 13Department of Neurology, School of Medicine, Kyungpook National University, Daegu, Korea.
- 14Department of Neurology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. mcastenosis@gmail.com
- KMID: 2467765
- DOI: http://doi.org/10.3988/jcn.2019.15.4.545
Abstract
- BACKGROUND AND PURPOSE
The clinical implications of echocardiography findings for long-term outcomes in atrial fibrillation (AF)-related stroke patients are unknown.
METHODS
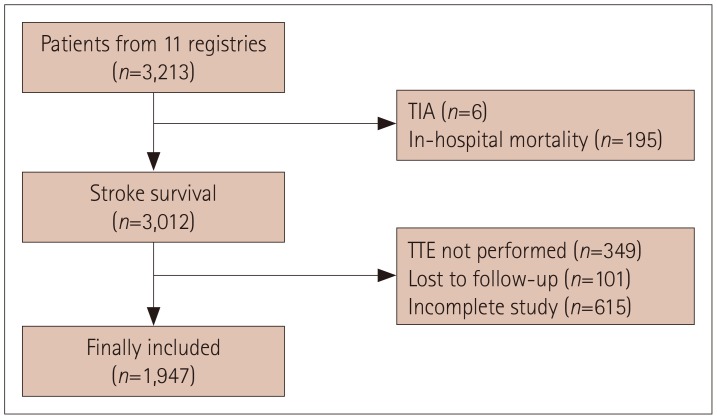
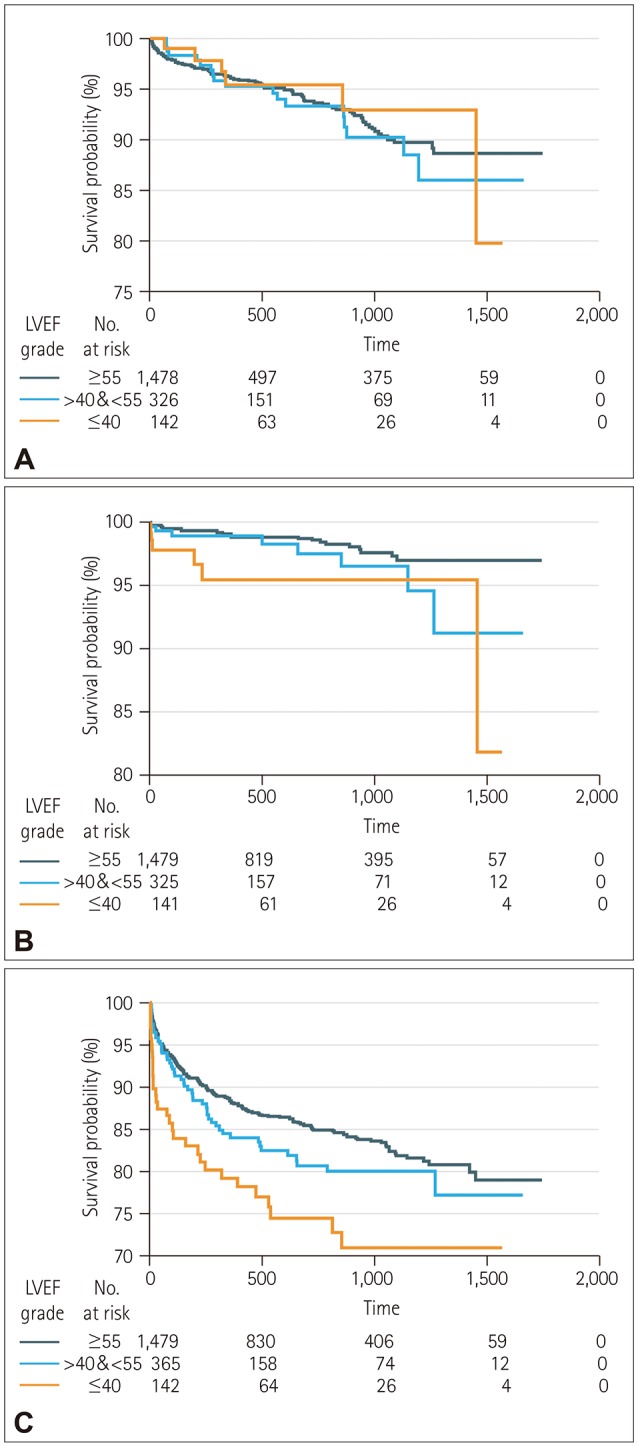
This was a substudy of the Korean ATrial fibrillaTion EvaluatioN regisTry in Ischemic strOke patieNts (K-ATTENTION), which is a multicenter-based cohort comprising prospective stroke registries from 11 tertiary centers. Stroke survivors who underwent two-dimensional transthoracic echocardiography during hospitalization were enrolled. Echocardiography markers included the left-ventricle (LV) ejection fraction (LVEF), the left atrium diameter, and the ratio of the peak transmitral filling velocity to the mean mitral annular velocity during early diastole (E/e"² ratio). LVEF was categorized into normal (≥55%), mildly decreased (>40% and <55%), and severely decreased (≤40%). The E/e"² ratio associated with the LV filling pressure was categorized into normal (<8), borderline (≥8 and <15), and elevated (≥15). Kaplan-Meier and Cox regression analyses were performed for recurrent stroke, major adverse cardiac events, and all-cause death.
RESULTS
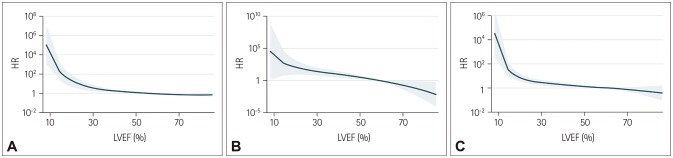
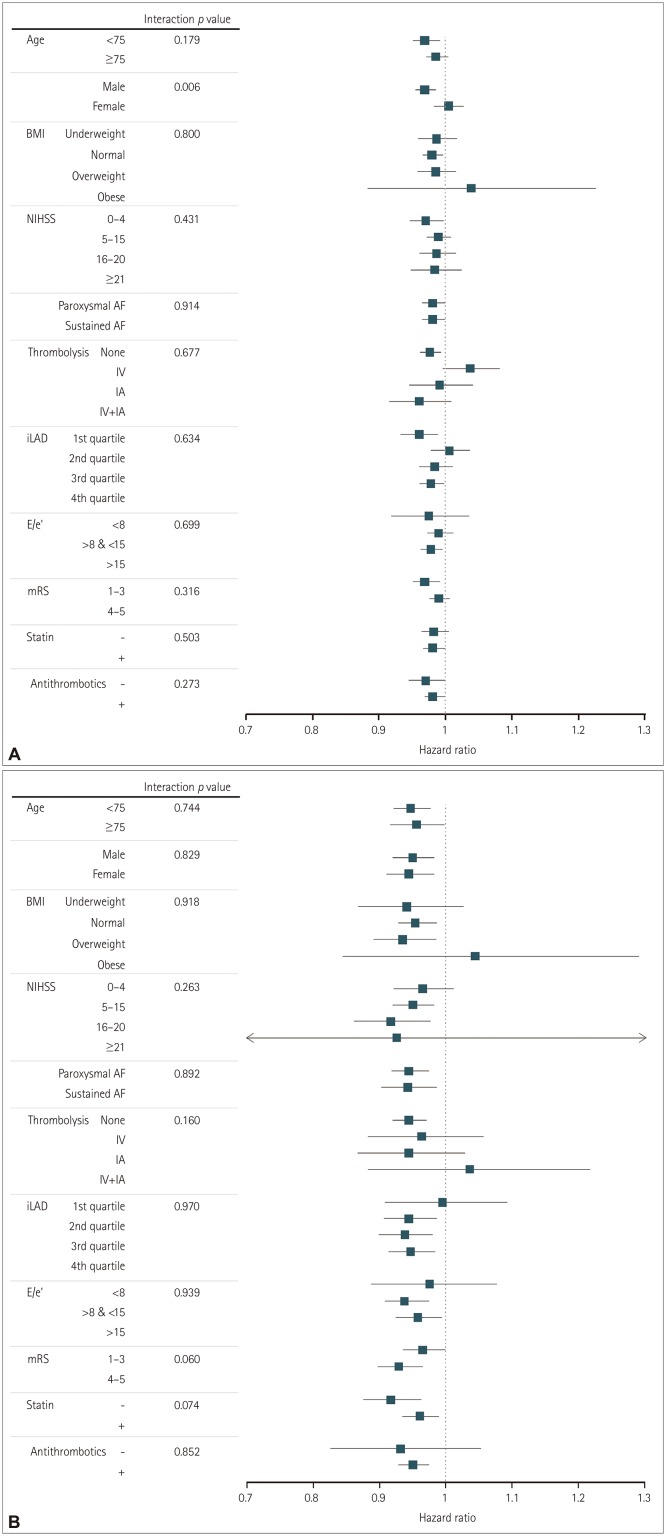
This study finally included 1,947 patients. Over a median follow-up of 1.65 years (interquartile range, 0.42-2.87 years), the rates of recurrent stroke, major adverse cardiac events, and all-cause death were 35.1, 10.8, and 69.6 cases per 1,000 person-years, respectively. Multivariable analyses demonstrated that severely decreased LVEF was associated with a higher risks of major adverse cardiac events [hazard ratio (HR), 3.91; 95% confidence interval (CI), 1.58-9.69] and all-cause death (HR, 1.95; 95% CI, 1.23-3.10). The multivariable fractional polynomial plot indicated that recurrent stroke might be associated with a lower LVEF.
CONCLUSIONS
Severe LV systolic dysfunction could be a determinant of long-term outcomes in AF-related stroke.
Keyword
MeSH Terms
Figure
Reference
-
1. Guo XY, Li N, Du X, Bai R, Yu RH, Long DY, et al. Atrial fibrillation is associated with an increased risk of myocardial infarction: insights from a meta-analysis. Atherosclerosis. 2016; 254:1–7. PMID: 27673698.
Article2. Kaarisalo MM, Immonen-Räihä P, Marttila RJ, Salomaa V, Kaarsalo E, Salmi K, et al. Atrial fibrillation and stroke. Mortality and causes of death after the first acute ischemic stroke. Stroke. 1997; 28:311–315. PMID: 9040681.3. Marini C, De Santis F, Sacco S, Russo T, Olivieri L, Totaro R, et al. Contribution of atrial fibrillation to incidence and outcome of ischemic stroke: results from a population-based study. Stroke. 2005; 36:1115–1119. PMID: 15879330.4. Lin HJ, Wolf PA, Kelly-Hayes M, Beiser AS, Kase CS, Benjamin EJ, et al. Stroke severity in atrial fibrillation. The Framingham Study. Stroke. 1996; 27:1760–1764. PMID: 8841325.5. Koga M, Yoshimura S, Hasegawa Y, Shibuya S, Ito Y, Matsuoka H, et al. Higher risk of ischemic events in secondary prevention for patients with persistent than those with paroxysmal atrial fibrillation. Stroke. 2016; 47:2582–2588. PMID: 27531346.
Article6. Lee SR, Choi EK, Han KD, Cha MJ, Oh S, Lip GYH. Temporal trends of antithrombotic therapy for stroke prevention in Korean patients with non-valvular atrial fibrillation in the era of non-vitamin K antagonist oral anticoagulants: a nationwide population-based study. PLoS One. 2017; 12:e0189495. PMID: 29261716.
Article7. Simpson E, Stevenson M, Scope A, Poku E, Minton J, Evans P. Echocardiography in newly diagnosed atrial fibrillation patients: a systematic review and economic evaluation. Health Technol Assess. 2013; 17:1–263. v–vi.
Article8. Miles JA, Garber L, Ghosh S, Spevack DM. Association of transthoracic echocardiography findings and long-term outcomes in patients undergoing workup of stroke. J Stroke Cerebrovasc Dis. 2018; 27:2943–2950. PMID: 30072178.
Article9. Milionis H, Faouzi M, Cordier M, D'Ambrogio-Remillard S, Eskandari A, Michel P. Characteristics and early and long-term outcome in patients with acute ischemic stroke and low ejection fraction. Int J Cardiol. 2013; 168:1082–1087. PMID: 23176765.
Article10. Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2015; 16:233–270. PMID: 25712077.
Article11. Kim WJ, Nah HW, Kim DH, Cha JK. Association between left ventricular dysfunction and functional outcomes at three months in acute ischemic stroke. J Stroke Cerebrovasc Dis. 2016; 25:2247–2252. PMID: 27449114.
Article12. Gupta DK, Giugliano RP, Ruff CT, Claggett B, Murphy S, Antman E, et al. The prognostic significance of cardiac structure and function in atrial fibrillation: the ENGAGE AF-TIMI 48 echocardiographic substudy. J Am Soc Echocardiogr. 2016; 29:537–544. PMID: 27106009.13. Friberg L, Hammar N, Pettersson H, Rosenqvist M. Increased mortality in paroxysmal atrial fibrillation: report from the Stockholm Cohort-Study of Atrial Fibrillation (SCAF). Eur Heart J. 2007; 28:2346–2353. PMID: 17670754.
Article14. Wang TJ, Larson MG, Levy D, Vasan RS, Leip EP, Wolf PA, et al. Temporal relations of atrial fibrillation and congestive heart failure and their joint influence on mortality: the Framingham Heart Study. Circulation. 2003; 107:2920–2925. PMID: 12771006.15. Marijon E, Le Heuzey JY, Connolly S, Yang S, Pogue J, Brueckmann M, et al. Causes of death and influencing factors in patients with atrial fibrillation: a competing-risk analysis from the randomized evaluation of long-term anticoagulant therapy study. Circulation. 2013; 128:2192–2201. PMID: 24016454.16. Kim W, Kim EJ. Heart failure as a risk factor for stroke. J Stroke. 2018; 20:33–45. PMID: 29402070.
Article17. Jover E, Roldán V, Gallego P, Hernández-Romero D, Valdés M, Vicente V, et al. Predictive value of the CHA2DS2-VASc score in atrial fibrillation patients at high risk for stroke despite oral anticoagulation. Rev Esp Cardiol (Engl Ed). 2012; 65:627–633. PMID: 22609214.18. Tanaka K, Yamada T, Torii T, Furuta K, Matsumoto S, Yoshimura T, et al. Pre-admission CHADS2, CHA2DS2-VASc, and R2CHADS2 scores on severity and functional outcome in acute ischemic stroke with atrial fibrillation. J Stroke Cerebrovasc Dis. 2015; 24:1629–1635. PMID: 25906940.19. Holmström A, Fu ML, Hjalmarsson C, Bokemark L, Andersson B. Heart dysfunction in patients with acute ischemic stroke or TIA does not predict all-cause mortality at long-term follow-up. BMC Neurol. 2013; 13:122. PMID: 24053888.
Article20. Stöllberger C, Chnupa P, Abzieher C, Länger T, Finsterer J, Klem I, et al. Mortality and rate of stroke or embolism in atrial fibrillation during long-term follow-up in the embolism in left atrial thrombi (ELAT) study. Clin Cardiol. 2004; 27:40–46. PMID: 14743856.
Article21. Ferreira JP, Girerd N, Gregson J, Länger T, Finsterer J, Klem I, et al. Stroke risk in patients with reduced ejection fraction after myocardial infarction without atrial fibrillation. J Am Coll Cardiol. 2018; 71:727–735. PMID: 29447733.
Article22. Pullicino PM, Qian M, Sacco RL, Freudenberger R, Graham S, Teerlink JR, et al. Recurrent stroke in the warfarin versus aspirin in reduced cardiac ejection fraction (WARCEF) trial. Cerebrovasc Dis. 2014; 38:176–181. PMID: 25300706.
Article23. Agarwal M, Apostolakis S, Lane DA, Lip GY. The impact of heart failure and left ventricular dysfunction in predicting stroke, thromboembolism, and mortality in atrial fibrillation patients: a systematic review. Clin Ther. 2014; 36:1135–1144. PMID: 25146364.
Article24. Yaghi S, Moon YP, Mora-McLaughlin C, Willey JZ, Cheung K, Di Tullio MR, et al. Left atrial enlargement and stroke recurrence: the Northern Manhattan Stroke Study. Stroke. 2015; 46:1488–1493. PMID: 25908460.
Article25. Broughton ST, O'Neal WT, Salahuddin T, Soliman EZ. The influence of left atrial enlargement on the relationship between atrial fibrillation and stroke. J Stroke Cerebrovasc Dis. 2016; 25:1396–1402. PMID: 27012217.
Article26. Paciaroni M, Agnelli G, Falocci N, Caso V, Becattini C, Marcheselli S, et al. Prognostic value of trans-thoracic echocardiography in patients with acute stroke and atrial fibrillation: findings from the RAF study. J Neurol. 2016; 263:231–237. PMID: 26566907.
Article27. Ogata T, Matsuo R, Kiyuna F, Hata J, Ago T, Tsuboi Y, et al. Left atrial size and long-term risk of recurrent stroke after acute ischemic stroke in patients with nonvalvular atrial fibrillation. J Am Heart Assoc. 2017; 6:e006402. PMID: 28862939.
Article28. Kalam K, Otahal P, Marwick TH. Prognostic implications of global LV dysfunction: a systematic review and meta-analysis of global longitudinal strain and ejection fraction. Heart. 2014; 100:1673–1680. PMID: 24860005.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Delayed Sealing of WATCHMAN Device Shunt
- The Mechanism of and Preventive Therapy for Stroke in Patients with Atrial Fibrillation
- Efficiency of MVP ECG Risk Score for Prediction of Long-Term Atrial Fibrillation in Patients With ICD for Heart Failure With Reduced Ejection Fraction
- The Difference of Left Atrial Volume Index: Can It Predict the Occurrence of Atrial Fibrillation after Radiofrequency Ablation of Atrial Flutter?
- How and When to Screen for Atrial Fibrillation after Stroke: Insights from Insertable Cardiac Monitoring Devices