J Clin Neurol.
2019 Apr;15(2):228-234. 10.3988/jcn.2019.15.2.228.
Conjugate Eye Deviation in Unilateral Lateral Medullary Infarction
- Affiliations
-
- 1Department of Neurology, Ludwig Maximilian University (LMU), Munich, Germany. katharina.feil@med.uni-muenchen.de
- 2German Center for Vertigo and Balance Disorders, Ludwig Maximilian University (LMU), Munich, Germany.
- 3Department of Neuroradiology, University Hospital Carl Gustav Carus, Dresden, Germany.
- 4Department of Neurology Inselspital, Bern University Hospital, Bern, Switzerland.
- KMID: 2467737
- DOI: http://doi.org/10.3988/jcn.2019.15.2.228
Abstract
- BACKGROUND AND PURPOSE
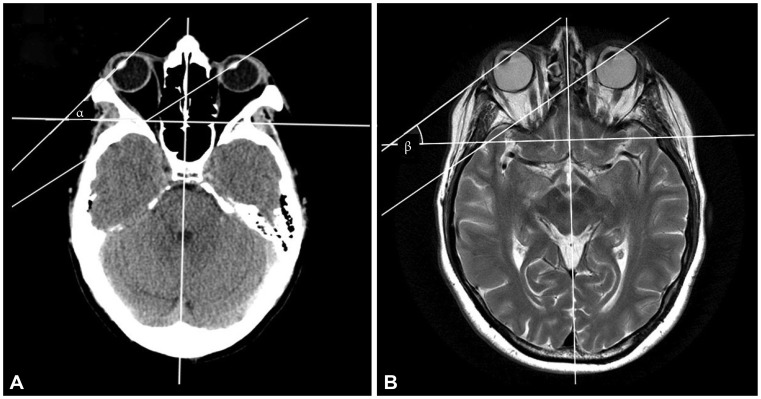
The initial diagnosis of medullary infarction can be challenging since CT and even MRI results in the very acute phase are often negative.
METHODS
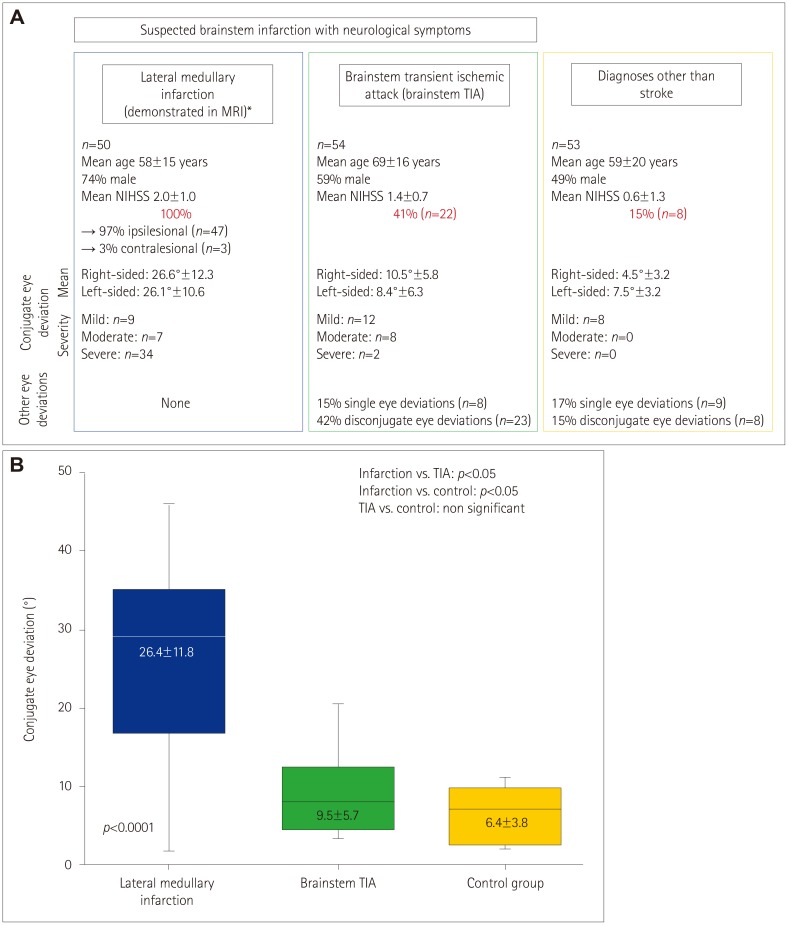
A retrospective, observer-blinded study of horizontal conjugate eye deviation was performed in 1) 50 consecutive patients [age 58±15 years (mean±SD), 74% male, National Institutes of Health Stroke Scale 2±1] with acute unilateral lateral medullary infarction as seen in MRI (infarction group), 2) 54 patients with transient brainstem symptoms [transient ischemic attack of brainstem (TIA) group; age 69±16 years, 59% male], and 3) 53 patients (age 59±20 years, 49% male) with diagnoses other than stroke (control group).
RESULTS
Conjugate eye deviation was found in all patients in the infarction group [n=47 (94%) with ipsilesional deviation and n=3 (6%) with contralesional deviation] compared to 41% (n=22) in the brainstem TIA group and 15% (n=8) in the control group (p<0.0001). Within all groups mean deviation and range were similar for both sides (to the right vs. to the left side 26.6°±12.3 vs. 26.1°±12.3 in the infarction group, 10.5°±5.8 vs. 8.4°±6.3 in the brainstem TIA group and 4.5°±3.2 vs. 7.5°±3.2 in the control group). The extent of eye deviation was significantly greater in the infarction group (p<0.05).
CONCLUSIONS
All patients with MRI-demonstrated unilateral medullary infarction showed conjugate eye deviation. Therefore, conjugate eye deviation in patients with suspected acute lateral medullary infarction is a helpful sensitive sign for supporting the diagnosis, particularly if the deviation is >20°.
Keyword
MeSH Terms
Figure
Reference
-
1. Bryan RN, Levy LM, Whitlow WD, Killian JM, Preziosi TJ, Rosario JA. Diagnosis of acute cerebral infarction: comparison of CT and MR imaging. AJNR Am J Neuroradiol. 1991; 12:611–620. PMID: 1688347.2. Sylaja PN, Coutts SB, Krol A, Hill MD, Demchuk AM. VISION Study Group. When to expect negative diffusion-weighted images in stroke and transient ischemic attack. Stroke. 2008; 39:1898–1900. PMID: 18420957.
Article3. Singer OC, Humpich MC, Laufs H, Lanfermann H, Steinmetz H, Neumann-Haefelin T. Conjugate eye deviation in acute stroke: incidence, hemispheric asymmetry, and lesion pattern. Stroke. 2006; 37:2726–2732. PMID: 17008621.4. Ringman JM, Saver JL, Woolson RF, Adams HP. Hemispheric asymmetry of gaze deviation and relationship to neglect in acute stroke. Neurology. 2005; 65:1661–1662. PMID: 16301502.
Article5. Kim JS, Moon SY, Park SH, Yoon BW, Roh JK. Ocular lateropulsion in Wallenberg syndrome. Neurology. 2004; 62:2287. PMID: 15210896.
Article6. Crevits L, Vander Eecken H. Ocular lateropulsion in Wallenberg's syndrome: a prospective clinical study. Acta Neurol Scand. 1982; 65:219–222. PMID: 7080807.
Article7. Kattah JC, Pula J, Newman-Toker DE. Ocular lateropulsion as a central oculomotor sign in acute vestibular syndrome is not posturally dependent. Ann N Y Acad Sci. 2011; 1233:249–255. PMID: 21951001.
Article8. Dieterich M, Brandt T. Wallenberg's syndrome: lateropulsion, cyclorotation, and subjective visual vertical in thirty-six patients. Ann Neurol. 1992; 31:399–408. PMID: 1586141.
Article9. Kim JS. Pure lateral medullary infarction: clinical-radiological correlation of 130 acute, consecutive patients. Brain. 2003; 126:1864–1872. PMID: 12805095.
Article10. Solomon D, Galetta SL, Liu GT. Possible mechanisms for horizontal gaze deviation and lateropulsion in the lateral medullary syndrome. J Neuroophthalmol. 1995; 15:26–30. PMID: 7780568.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Isolated Axial Lateropulsion in Lateral Medullary Infarction
- A Case of Lateral Medullary Syndrome with Ipsilesional Nystagmus due to Intramedullary Hemorrhage
- A Case of Airway Obstruction Caused by Bilateral Vocal Cord Palsy in a Patient with Lateral Medullary Infarction
- The Effect of Unilateral Surgery in Dissociated Vertical Deviation
- Opalski Syndrome Presenting as Sensorimotor Deficits Ipsilateral to Cerebral Infarction