J Korean Acad Community Health Nurs.
2019 Dec;30(4):400-413. 10.12799/jkachn.2019.30.4.400.
A Systematic Review of Studies Using Video-recording to Capture Interactions between Staff and Persons with Dementia in Long-term Care Facilities
- Affiliations
-
- 1Visiting Scholar, School of Nursing, University of Wisconsin-Madison, Madison, WI, USA.
- 2Doctoral Student, College of Nursing, Seoul National University, Seoul, Korea.
- 3Associate Professor, College of Nursing · Research Institute of Nursing Science, Seoul National University, Seoul, Korea. yoon26@snu.ac.kr
- KMID: 2467642
- DOI: http://doi.org/10.12799/jkachn.2019.30.4.400
Abstract
- PURPOSE
The use of video-recording offers important advantages in observing and assessing the relationship between specific behaviors in health care settings. The purpose of this systematic review is to investigate and synthesize the methodological characteristics of studies using video-technology for measuring interactions with the older persons with dementia and staff in long-term care facilities.
METHODS
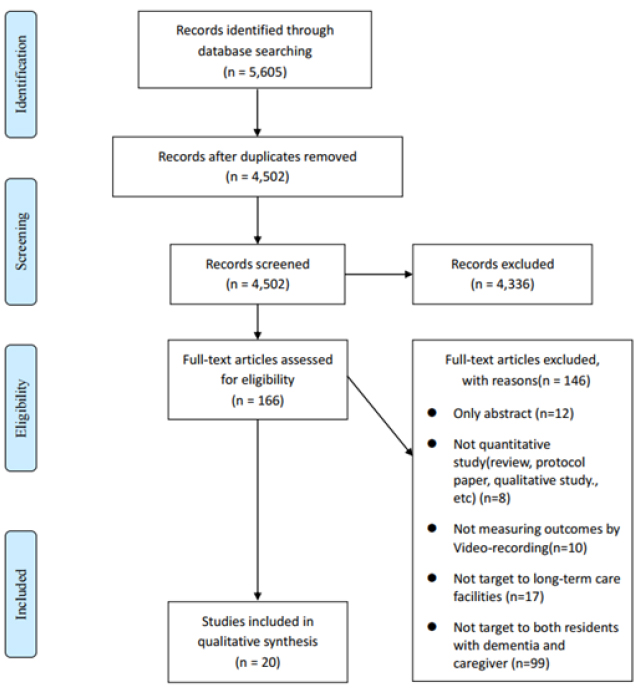
We searched Medline, Embase and CINHAL databases for published articles in English using a video-recording method for both staff and the residents with dementia. Quantitative research design studies (e.g., descriptive or experimental studies) were included.
RESULTS
Among 5,605 searched papers, a total of 20 studies were selected for this review. Situations of video-recording were providing personal care (n=12), mealtime (n=6), and conversation (n=3). Concepts measured by video-recording were classified into two groups: 1) Staff [care practice by staff (n=13) and communication by staff (n=11)] and 2) residents [communication by resident (n=4), activities of daily life function of resident (n=8), and behavioral and psychological symptoms of dementia (n=10)].
CONCLUSION
This review demonstrates that video technologies are actively used to evaluate the relationship between quality of care and health outcomes of the elderly with dementia in many international nursing studies. This study provides the foundation for a future research using video-recording technologies to examine the interactions and relationships between staff and the residents in Korean long-term care settings.
Figure
Reference
-
1. Koren MJ. Person-centered care for nursing home residents: The culture-change movement. Health Affairs. 2010; 29(2):312–317. DOI: 10.1377/hlthaff.2009.0966.
Article2. Li J, Porock D. Resident outcomes of person-centered care in long-term care: A narrative review of interventional research. International Journal of Nursing Studies. 2014; 51(10):1395–1415. DOI: 10.1016/j.ijnurstu.2014.04.003.
Article3. Ellis-Smith C, Evans CJ, Bone AE, Henson LA, Dzingina M, Kane PM, et al. Measures to assess commonly experienced symptoms for people with dementia in long-term care settings: A systematic review. BMC Medicine. 2016; 14(1):38. DOI: 10.1186/s12916-016-0582-x.
Article4. Latvala E, Vuokila Oikkonen P, Janhonen S. Videotaped recording as a method of participant observation in psychiatric nursing research. Journal of Advanced Nursing. 2000; 31(5):1252–1257. DOI: 10.1046/j.1365-2648.2000.01383.x.
Article5. Haidet KK, Tate J, Divirgilio Thomas D, Kolanowski A, Happ MB. Methods to improve reliability of video recorded behavioral data. Research in Nursing & Health. 2009; 32(4):465–474. DOI: 10.1002/nur.2033.6. Herman RE, Williams KN. Elderspeak's influence on resistiveness to care: Focus on behavioral events. American journal of Alzheimer's disease and other dementias. 2009; 24(5):417–423. DOI: 10.1177/1533317509341949.
Article7. Sloane PD, Miller LL, Mitchell CM, Rader J, Swafford K, Hiatt SO. Provision of morning care to nursing home residents with dementia: Opportunity for improvement? American journal of Alzheimer's disease and other dementias. 2007; 22(5):369–377. DOI: 10.1177/1533317507305593.
Article8. Gilmore-Bykovskyi AL, Roberts TJ, Bowers BJ, Brown RL. Caregiver person-centeredness and behavioral symptoms in nursing home residents with dementia: A timed-event sequential analysis. The Gerontologist. 2015; 55:Suppl 1. S61–S66. DOI: 10.1093/geront/gnu164.
Article9. Cook A. Using video observation to include the experiences of people with dementia in research. In : Wilkinson H, editor. The perspectives of people with dementia: Research methods and motivations. London and Philadelphia: Jessica Kingsley Publishers;2002. p. 209–222.10. Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic Reviews. 2015; 4(1):1. DOI: 10.1186/2046-4053-4-1.
Article11. Kim SY, Park JE, Seo HJ, Lee YJ, Jang BH, Son HJ, et al. NECA's guidance for undertaking systematic reviews and meta-analyses for intervention [Internet]. Seoul: National Evidence-based Healthcare Collaborating Agency;c2011. cited 2017 June 1. Available from: https://www.neca.re.kr/lay1/bbs/S1T11C102/F/39/view.do?article_seq=5329&cpage=2&rows=10&condition=&keyword=&show=&cat=.12. Bourgeois M, Dijkstra K, Burgio L, Allen-Burge R. Memory aids as an augmentative and alternative communication strategy for nursing home residents with dementia. Augmentative and Alternative Communication. 2001; 17(3):196–210. DOI: 10.1080/aac.17.3.196.210.
Article13. Kihlgren M, Kuremyr D, Norberg A, Bråne G, Karlson I, Engström B, et al. Nurse-patient interaction after training in integrity promoting care at a long-term ward: Analysis of video-recorded morning care sessions. International Journal of Nursing Studies. 1993; 30(1):1–13.
Article14. Cohen-Mansfield J, Creedon MA, Malone T, Parpura-Gill A, Dakheel-Ali M, Heasly C. Dressing of cognitively impaired nursing home residents: Description and analysis. The Gerontologist. 2006; 46(1):89–96.
Article15. Wilson R, Rochon E, Mihailidis A, Leonard C. Examining success of communication strategies used by formal caregivers assisting individuals with Alzheimer's disease during an activity of daily living. Journal of Speech, Language, and Hearing Research. 2012; 55(2):328–341. DOI: 10.1044/1092-4388(2011/10-0206).
Article16. Gilmore-Bykovskyi AL. Caregiver person-centeredness and behavioral symptoms during mealtime interactions: Development and feasibility of a coding scheme. Geriatric Nursing. 2015; 36(2 Suppl):S10–S15. DOI: 10.1016/j.gerinurse.2015.02.018.
Article17. Thunborg C, von Heideken Wågert P, Götell E, Ivarsson A-B, Söderlund A. Development of a new assessment scale for measuring interaction during staff-assisted transfer of residents in dementia special care units. BMC geriatrics. 2015; 15(1):6. DOI: 10.1186/s12877-015-0003-6.
Article18. Jordan KJ, Tsai PF, Heo S, Bai S, Dailey D, Beck CK, et al. Pilot testing a coaching intervention to improve certified nursing assistants' dressing of nursing home residents. Research in Gerontological Nursing. 2017; 10(6):267–276. DOI: 10.3928/19404921-20171013-04.
Article19. Williams KN, Perkhounkova Y, Herman R, Bossen A. A communication intervention to reduce resistiveness in dementia care: A cluster randomized controlled trial. The Gerontologist. 2016; 57(4):707–718. DOI: 10.1093/geront/gnw047.
Article20. Williams KN, Herman R, Gajewski B, Wilson K. Elderspeak communication: Impact on dementia care. American journal of Alzheimer's disease and other dementias. 2009; 24(1):11–20. DOI: 10.1177/1533317508318472.
Article21. Lann-Wolcott H, Medvene LJ, Williams K. Measuring the person-centeredness of caregivers working with nursing home residents with dementia. Behavior Therapy. 2011; 42(1):89–99. DOI: 10.1016/j.beth.2010.02.005.
Article22. Somboontanont W, Sloane PD, Floyd FJ, Holditch-Davis D, Hogue CC, Mitchell CM. Assaultive behavior in Alzheimer's disease: Identifying immediate antecedents during bathing. Journal of Gerontological Nursing. 2004; 30(9):22–29.
Article23. Happ MB, Sereika S, Garrett K, Tate J. Use of the quasi-experimental sequential cohort design in the Study of Patient-Nurse Effectiveness with Assisted Communication Strategies (SPEACS). Contemporary Clinical Trials. 2008; 29(5):801–808. DOI: 10.1016/j.cct.2008.05.010.
Article24. Cunningham J, Williams KN. A case study of resistiveness to care and elderspeak. Research and Theory for Nursing Practice. 2007; 21(1):45–56.
Article25. Caldwell K, Atwal A. Non-participant observation: Using video tapes to collect data in nursing research. Nurse Researcher. 2005; 13(2):42–54.
Article26. van Weert JC, van Dulmen AM, Spreeuwenberg PM, Ribbe MW, Bensing JM. Effects of snoezelen, integrated in 24h dementia care, on nurse-patient communication during morning care. Patient Education and Counseling. 2005; 58(3):312–326. DOI: 10.1016/j.pec.2004.07.013.
Article27. Belzil G, Vézina J. Impact of caregivers' behaviors on resistiveness to care and collaboration in persons with dementia in the context of hygienic care: An interactional perspective. International Psychogeriatrics. 2015; 27(11):1861–1873. DOI: 10.1017/S104161021500099X.
Article28. Carpiac-Claver ML, Levy-Storms L. In a manner of speaking: Communication between nurse aides and older adults in long-term care settings. Health Communication. 2007; 22(1):59–67. DOI: 10.1080/10410230701310307.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nursing Staff Stress From Caregiving and Attitudes Toward Family Members of Nursing Home Residents With Dementia in Korea
- Korean Family Caregivers' Perceptions of Care in Dementia Care Units
- Predictors of Behavioral and Psychological Symptoms of Dementia: Based on the Model of Multi-Dimensional Behavior
- Clinical Approaches to the Long-term Care Service focused on Dementia
- Family Membe's Caregiving Stress and Satisfaction of Care for Patients with Dementia in Long Term Care Facilities and Day Care Centers