Acute Crit Care.
2019 Nov;34(4):246-254. 10.4266/acc.2019.00668.
Effect of a rapid response system on code rates and in-hospital mortality in medical wards
- Affiliations
-
- 1Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea. apricot6@snu.ac.kr
- 2Rapid Response Team, Seoul National University Hospital, Seoul, Korea.
- 3Department of Thoracic and Cardiovascular Surgery, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea.
- 4Department of Anesthesiology and Pain Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea.
- 5Department of General Surgery, Seoul National University Hospital, Seoul, Korea.
- 6Critical Care Center, Seoul National University Hospital, Seoul, Korea.
- 7Department of Neurology, Seoul National University Hospital, Seoul, Korea.
- KMID: 2467303
- DOI: http://doi.org/10.4266/acc.2019.00668
Abstract
- BACKGROUND
To determine the effects of implementing a rapid response system (RRS) on code rates and in-hospital mortality in medical wards.
METHODS
This retrospective study included adult patients admitted to medical wards at Seoul National University Hospital between July 12, 2016 and March 12, 2018; the sample comprised 4,224 patients admitted 10 months before RRS implementation and 4,168 patients admitted 10 months following RRS implementation. Our RRS only worked during the daytime (7 AM to 7 PM) on weekdays. We compared code rates and in-hospital mortality rates between the preintervention and postintervention groups.
RESULTS
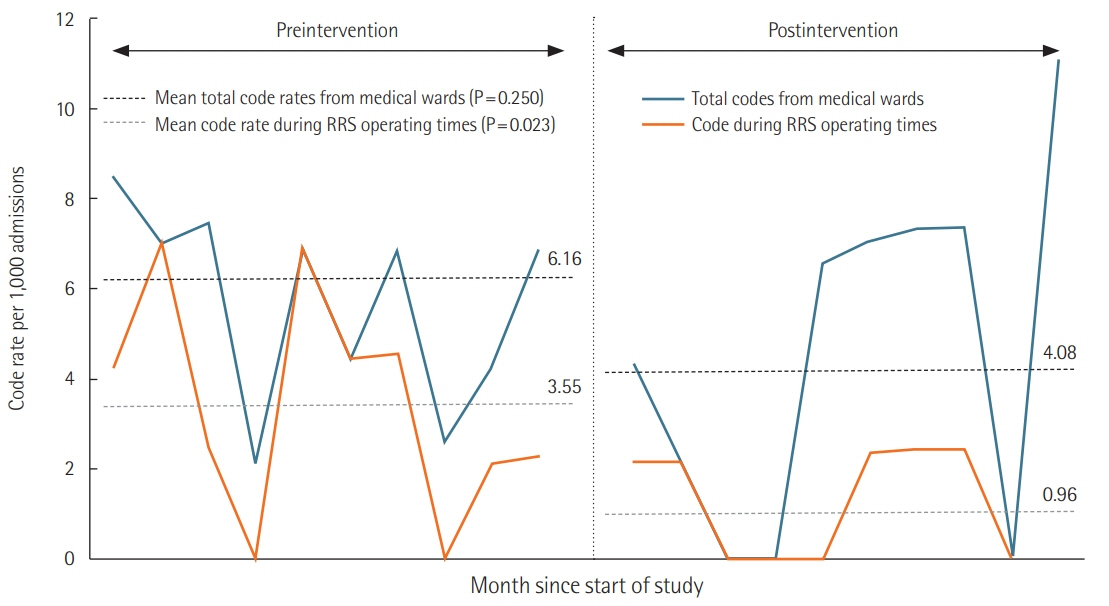
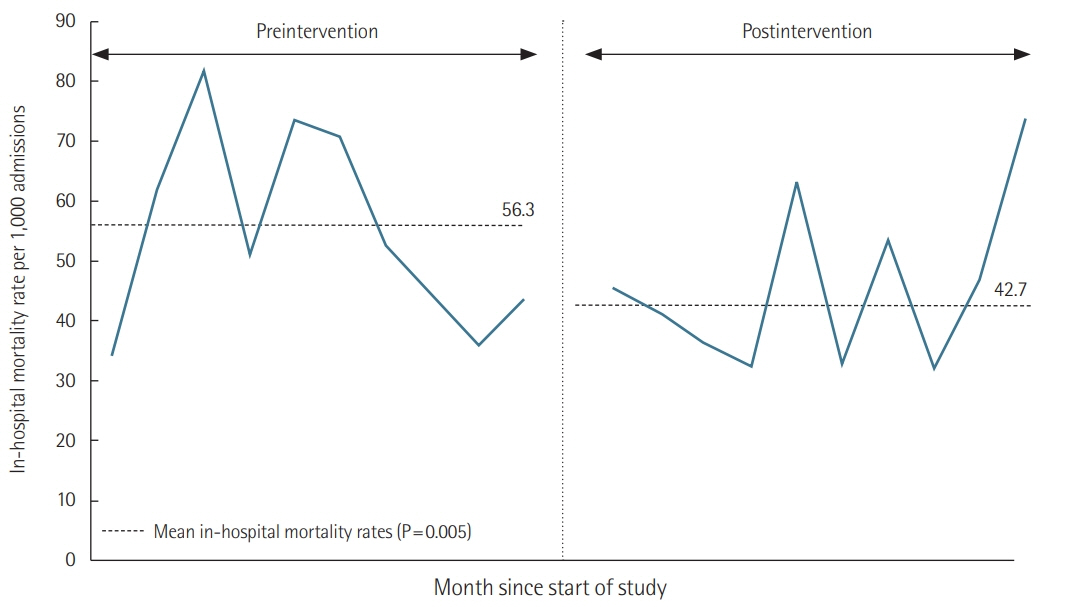
There were 62.3 RRS activations per 1,000 admissions. The most common reasons for RRS activation were tachypnea or hypopnea (44%), hypoxia (31%), and tachycardia or bradycardia (21%). Code rates from medical wards during RRS operating times significantly decreased from 3.55 to 0.96 per 1,000 admissions (adjusted odds ratio [aOR], 0.29; 95% confidence interval [CI], 0.10 to 0.87; P=0.028) after RRS implementation. However, code rates from medical wards during RRS nonoperating times did not differ between the preintervention and postintervention groups (2.60 vs. 3.12 per 1,000 admissions; aOR, 1.23; 95% CI, 0.55 to 2.76; P=0.614). In-hospital mortality significantly decreased from 56.3 to 42.7 per 1,000 admissions after RRS implementation (aOR, 0.79; 95% CI, 0.64 to 0.97; P=0.024).
CONCLUSIONS
Implementation of an RRS was associated with significant reductions in code rates during RRS operating times and in-hospital mortality in medical wards.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Evidence revealed the effects of rapid response system
Jae Hwa Cho
Acute Crit Care. 2019;34(4):282-283. doi: 10.4266/acc.2019.00710.
Reference
-
1. Jones D, Rubulotta F, Welch J. Rapid response teams improve outcomes: yes. Intensive Care Med. 2016; 42:593–5.
Article2. Litvak E, Pronovost PJ. Rethinking rapid response teams. JAMA. 2010; 304:1375–6.
Article3. Neumar RW, Shuster M, Callaway CW, Gent LM, Atkins DL, Bhanji F, et al. Part 1: executive summary: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015; 132(18 Suppl 2):S315–67.4. McGaughey J, Alderdice F, Fowler R, Kapila A, Mayhew A, Moutray M. Outreach and Early Warning Systems (EWS) for the prevention of intensive care admission and death of critically ill adult patients on general hospital wards. Cochrane Database Syst Rev. 2007; (3):CD005529.
Article5. Chan PS, Jain R, Nallmothu BK, Berg RA, Sasson C. Rapid response teams: a systematic review and meta-analysis. Arch Intern Med. 2010; 170:18–26.6. Salvatierra G, Bindler RC, Corbett C, Roll J, Daratha KB. Rapid response team implementation and in-hospital mortality. Crit Care Med. 2014; 42:2001–6.
Article7. Jung B, Daurat A, De Jong A, Chanques G, Mahul M, Monnin M, et al. Rapid response team and hospital mortality in hospitalized patients. Intensive Care Med. 2016; 42:494–504.
Article8. Maharaj R, Raffaele I, Wendon J. Rapid response systems: a systematic review and meta-analysis. Crit Care. 2015; 19:254.
Article9. Solomon RS, Corwin GS, Barclay DC, Quddusi SF, Dannenberg MD. Effectiveness of rapid response teams on rates of inhospital cardiopulmonary arrest and mortality: a systematic review and meta-analysis. J Hosp Med. 2016; 11:438–45.
Article10. Lee BY, Hong SB. Rapid response systems in Korea. Acute Crit Care. 2019; 34:108–16.
Article11. Subbe CP, Kruger M, Rutherford P, Gemmel L. Validation of a modified Early Warning Score in medical admissions. QJM. 2001; 94:521–6.
Article12. Hillman K, Chen J, Cretikos M, Bellomo R, Brown D, Doig G, et al. Introduction of the medical emergency team (MET) system: a cluster-randomised controlled trial. Lancet. 2005; 365:2091–7.13. Jones DA, DeVita MA, Bellomo R. Rapid-response teams. N Engl J Med. 2011; 365:139–46.
Article14. Jones D, Bellomo R, DeVita MA. Effectiveness of the medical emergency team: the importance of dose. Crit Care. 2009; 13:313.
Article15. Lee YJ, Park JJ, Yoon YE, Kim JW, Park JS, Kim T, et al. Successful Implementation of a Rapid Response System in the Department of Internal Medicine. Korean J Crit Care Med. 2014; 29:77–82.
Article16. Lee YJ, Lee DS, Min H, Choi YY, Lee EY, Song I, et al. Differences in the clinical characteristics of rapid response system activation in patients admitted to medical or surgical services. J Korean Med Sci. 2017; 32:688–94.
Article17. Tabak YP, Johannes RS, Silber JH, Kurtz SG. Should Do-NotResuscitate status be included as a mortality risk adjustor? The impact of DNR variations on performance reporting. Med Care. 2005; 43:658–66.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Extended Rapid Response System: 1-Year Experience in a University Hospital
- The Clinical Characteristics of Admissions to Acute Geriatric wards in Borame Hospital
- Rates of COVID-19 Infection Among Healthcare Workers in Designated COVID-19 Wards and General Wards
- Strategies for successful implementation and permanent maintenance of a rapid response system
- Early Experience of Medical Alert System in a Rural Training Hospital: a Pilot Study