J Korean Assoc Oral Maxillofac Surg.
2019 Dec;45(6):374-376. 10.5125/jkaoms.2019.45.6.374.
Importance of various skin sutures in cheiloplasty of cleft lip
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Dental Research Institute, School of Dentistry, Seoul National University, Seoul, Korea. smin5@snu.ac.kr
- KMID: 2467191
- DOI: http://doi.org/10.5125/jkaoms.2019.45.6.374
Abstract
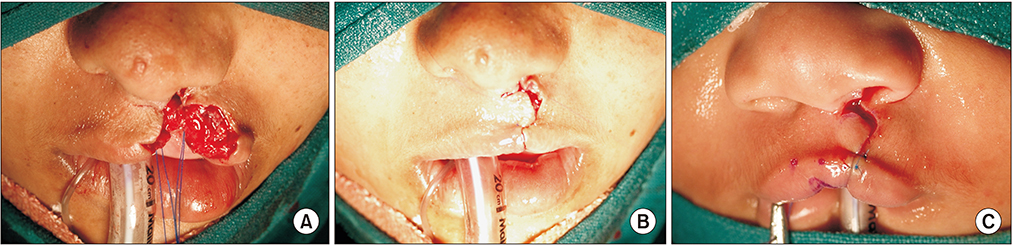
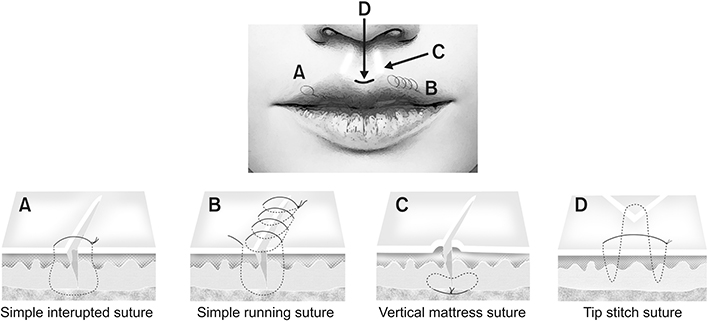
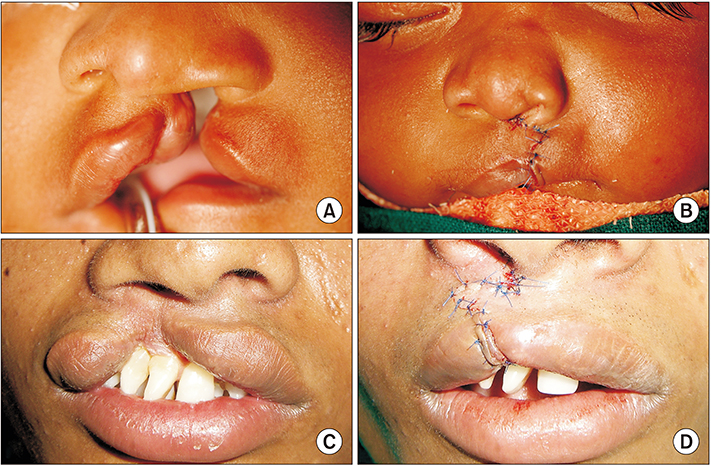
- Last week, after our receiving online journal regarding Journal of the Korean Association of Oral and Maxillofacial Surgeons, we found a recently published original article by Alawode et al., entitled "A comparative study of immediate wound healing complications following cleft lip repair using either absorbable or non-absorbable skin sutures". Although this clinical article was well written and provided a great deal of information regarding the suture materials in the cleft lip repair, I would like to add a few additional comments based on the importance of skin suture during cheiloplasties in the primary cleft lip or secondary revision patients with representative figures.
Figure
Cited by 1 articles
-
Current options in jaw and facial reconstructions
Soung Min Kim, Jong Ho Lee
J Korean Assoc Oral Maxillofac Surg. 2024;50(6):309-325. doi: 10.5125/jkaoms.2024.50.6.309.
Reference
-
1. Alawode AO, Adeyemi MO, James O, Ogunlewe MO, Butali A, Adeyemo WL. A comparative study of immediate wound healing complications following cleft lip repair using either absorbable or non-absorbable skin sutures. J Korean Assoc Oral Maxillofac Surg. 2018; 44:159–166.
Article2. Adesina OA, Efunkoya AA, Omeje KU, Idon PI. Postoperative complications from primary repair of cleft lip and palate in a semiurban Nigerian teaching hospital. Niger Med J. 2016; 57:155–159.
Article3. Shinohara H, Matsuo K, Kikuchi N. Absorbable and nonabsorbable buried sutures for primary cleft lip repair. Ann Plast Surg. 1996; 36:44–46.
Article4. Datarkar AN, Rewanwar D, Rai A. Comperative analysis of unilateral cleft lip closure using absorbable and nonabsorbable sutures: a randomised clinical study. Plast Aesthet Res. 2014; 1:54–57.
Article5. Gabrielli F, Potenza C, Puddu P, Sera F, Masini C, Abeni D. Suture materials and other factors associated with tissue reactivity, infection, and wound dehiscence among plastic surgery outpatients. Plast Reconstr Surg. 2001; 107:38–45.
Article6. Adetayo AM, James O, Adeyemo WL, Ogunlewe MO, Butali A. Unilateral cleft lip repair: a comparison of treatment outcome with two surgical techniques using quantitative (anthropometry) assessment. J Korean Assoc Oral Maxillofac Surg. 2018; 44:3–11.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical correction of cleft lip lower-lip deformity: a report of three cases
- Dovetail Cheiloplasty
- Formation of Philtral Column using AlloDerm(R) in Secondary Cleft Lip Deformity
- A comprehensive review of surgical techniques in unilateral cleft lip repair
- Application of inferior turbinate flap in cheiloplasty for wide cleft gaps