Diabetes and the Risk of Infection: A National Cohort Study
- Affiliations
-
- 1Department of Infectious Diseases, Ajou University School of Medicine, Suwon, Korea. yhwa1805@ajou.ac.kr
- 2Department of Endocrinology and Metabolism, Ajou University School of Medicine, Suwon, Korea.
- 3Cardiovascular and Metabolic Disease Etiology Research Center, Ajou University School of Medicine, Suwon, Korea.
- KMID: 2466502
- DOI: http://doi.org/10.4093/dmj.2019.0071
Abstract
- BACKGROUND
Several studies have shown that people with diabetes are vulnerable to infection. This study compared the risk of infection-related hospitalizations, intensive care unit (ICU) admission, and deaths between the person with diabetes and the general population in South Korea.
METHODS
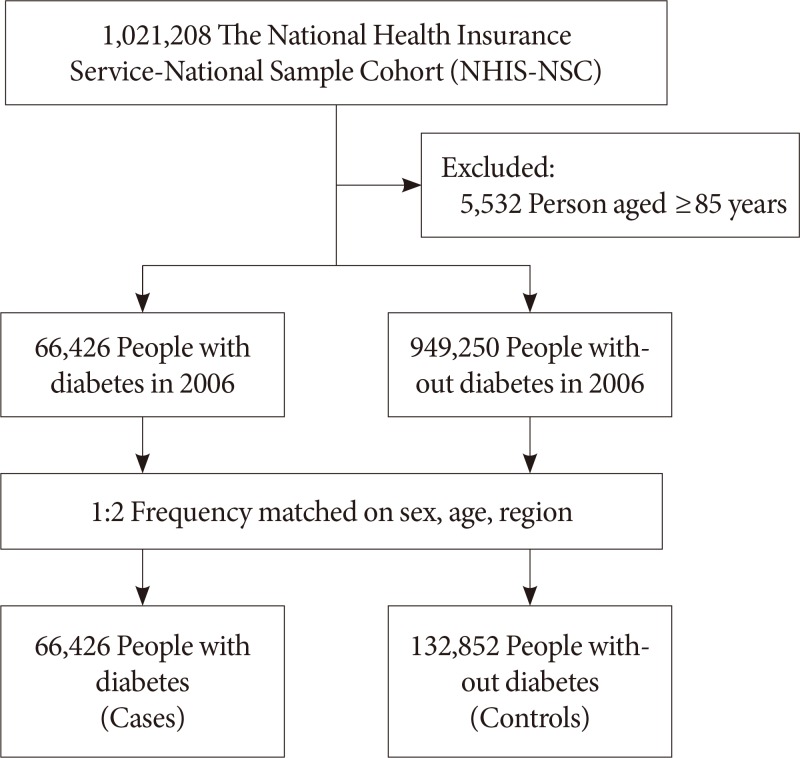
We conducted a cohort study of 66,426 diabetes and 132,852 age-sex-region-matched non-diabetes controls from the general population using a sample of data from the National Health Insurance Service-National Sample Cohort. The cohort was followed up for 9 years. Infections were classified into 17 separate categories. We used Poisson regression, with adjustment for household income and other comorbidities, to estimate incidence rate ratios (IRRs) in order to compare of infection-related hospitalizations, ICU admissions, and deaths.
RESULTS
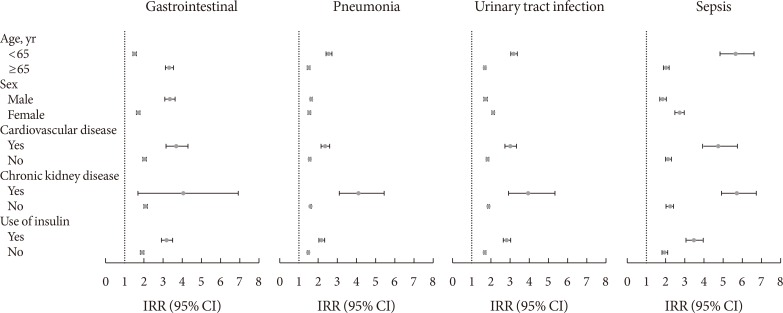
Compared to non-diabetes controls, diabetes group had a greater risk of almost all the types of infections considered, with the adjusted IRRs (aIRRs) for infection-related hospitalizations being the highest for hepatic abscess (aIRR, 10.17; 95% confidence interval [CI], 7.04 to 14.67), central nervous system (CNS) infections (aIRR, 8.72; 95% CI, 6.64 to 11.45), and skin and soft tissue infections other than cellulitis (SSTIs) (aIRR, 3.52; 95% CI, 3.20 to 3.88). Diabetes group also had a greater risk of ICU admission and death due to SSTIs (aIRR, 11.75; 95% CI, 7.32 to 18.86), CNS infections (aIRR, 5.25; 95% CI, 3.53 to 7.79), and bone and joint infections (aIRR, 4.78; 95% CI, 3.09 to 7.39).
CONCLUSION
In South Korea, people with diabetes has a considerably higher incidence of infection-related hospitalizations and deaths than the general population.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
Trends in Cardiovascular Complications and Mortality among Patients with Diabetes in South Korea
Jung Hwan Park, Kyoung Hwa Ha, Bo Yeon Kim, Jae Hyuk Lee, Dae Jung Kim
Diabetes Metab J. 2021;45(1):120-124. doi: 10.4093/dmj.2020.0175.Exercise Frequency Reduction Is Associated With Higher Risk of Infection in Newly Diagnosed Diabetes: A Nationally Representative Cohort Study
Yohwan Lim, Hye Jun Kim, Sung Soo Yoon, Sang Jun Lee, Myeong Hoon Lee, Hyewon Park, Sun Jae Park, Seogsong Jeong, Hyun Wook Han
J Korean Med Sci. 2023;38(23):e176. doi: 10.3346/jkms.2023.38.e176.Prediction of intensive care unit admission using machine learning in patients with odontogenic infection
Joo-Ha Yoon, Sung Min Park
J Korean Assoc Oral Maxillofac Surg. 2024;50(4):216-221. doi: 10.5125/jkaoms.2024.50.4.216.
Reference
-
1. International Diabetes Federation. IDF diabetes atlas. Brussels: International Diabetes Federation;2017.2. Ha KH, Kim DJ. Trends in the diabetes epidemic in Korea. Endocrinol Metab (Seoul). 2015; 30:142–146. PMID: 26194073.
Article3. Won JC, Lee JH, Kim JH, Kang ES, Won KC, Kim DJ, Lee MK. Diabetes fact sheet in Korea, 2016: an appraisal of current status. Diabetes Metab J. 2018; 42:415–424. PMID: 30113146.4. Bae JC. Trends of diabetes epidemic in Korea. Diabetes Metab J. 2018; 42:377–379. PMID: 30362303.
Article5. Trevelin SC, Carlos D, Beretta M, da Silva JS, Cunha FQ. Diabetes mellitus and sepsis: a challenging association. Shock. 2017; 47:276–287. PMID: 27787406.6. Carey IM, Critchley JA, DeWilde S, Harris T, Hosking FJ, Cook DG. Risk of infection in type 1 and type 2 diabetes compared with the general population: a matched cohort study. Diabetes Care. 2018; 41:513–521. PMID: 29330152.
Article7. Geerlings SE, Hoepelman AI. Immune dysfunction in patients with diabetes mellitus (DM). FEMS Immunol Med Microbiol. 1999; 26:259–265. PMID: 10575137.
Article8. Joshi N, Caputo GM, Weitekamp MR, Karchmer AW. Infections in patients with diabetes mellitus. N Engl J Med. 1999; 341:1906–1912. PMID: 10601511.
Article9. Korbel L, Spencer JD. Diabetes mellitus and infection: an evaluation of hospital utilization and management costs in the United States. J Diabetes Complications. 2015; 29:192–195. PMID: 25488325.
Article10. Mor A, Berencsi K, Nielsen JS, Rungby J, Friborg S, Brandslund I, Christiansen JS, Vaag A, Beck-Nielsen H, Sorensen HT, Thomsen RW. Rates of community-based antibiotic prescriptions and hospital-treated infections in individuals with and without type 2 diabetes: a Danish nationwide cohort study, 2004-2012. Clin Infect Dis. 2016; 63:501–511. PMID: 27353662.
Article11. McDonald HI, Nitsch D, Millett ER, Sinclair A, Thomas SL. New estimates of the burden of acute community-acquired infections among older people with diabetes mellitus: a retrospective cohort study using linked electronic health records. Diabet Med. 2014; 31:606–614. PMID: 24341529.
Article12. Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort profile: the National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int J Epidemiol. 2017; 46:e15. PMID: 26822938.
Article13. Naghibi M, Smith RP, Baltch AL, Gates SA, Wu DH, Hammer MC, Michelsen PB. The effect of diabetes mellitus on chemotactic and bactericidal activity of human polymorphonuclear leukocytes. Diabetes Res Clin Pract. 1987; 4:27–35. PMID: 3121272.
Article14. Mowat A, Baum J. Chemotaxis of polymorphonuclear leukocytes from patients with diabetes mellitus. N Engl J Med. 1971; 284:621–627. PMID: 5545603.
Article15. McManus LM, Bloodworth RC, Prihoda TJ, Blodgett JL, Pinckard RN. Agonist-dependent failure of neutrophil function in diabetes correlates with extent of hyperglycemia. J Leukoc Biol. 2001; 70:395–404. PMID: 11527989.16. Alba-Loureiro TC, Munhoz CD, Martins JO, Cerchiaro GA, Scavone C, Curi R, Sannomiya P. Neutrophil function and metabolism in individuals with diabetes mellitus. Braz J Med Biol Res. 2007; 40:1037–1044. PMID: 17665039.
Article17. Lehuen A, Diana J, Zaccone P, Cooke A. Immune cell crosstalk in type 1 diabetes. Nat Rev Immunol. 2010; 10:501–513. PMID: 20577267.
Article18. Wong CK, Ho AW, Tong PC, Yeung CY, Chan JC, Kong AP, Lam CW. Aberrant expression of soluble co-stimulatory molecules and adhesion molecules in type 2 diabetic patients with nephropathy. J Clin Immunol. 2008; 28:36–43. PMID: 18026823.
Article19. Graham PL 3rd, Lin SX, Larson EL. A U.S. population-based survey of Staphylococcus aureus colonization. Ann Intern Med. 2006; 144:318–325. PMID: 16520472.
Article20. de Leon EM, Jacober SJ, Sobel JD, Foxman B. Prevalence and risk factors for vaginal Candida colonization in women with type 1 and type 2 diabetes. BMC Infect Dis. 2002; 2:1. PMID: 11835694.
Article21. Abu-Ashour W, Twells LK, Valcour JE, Gamble JM. Diabetes and the occurrence of infection in primary care: a matched cohort study. BMC Infect Dis. 2018; 18:67. PMID: 29402218.
Article22. van Vught LA, Scicluna BP, Hoogendijk AJ, Wiewel MA, Klein Klouwenberg PM, Cremer OL, Horn J, Nurnberg P, Bonten MM, Schultz MJ, van der Poll T. Association of diabetes and diabetes treatment with the host response in critically ill sepsis patients. Crit Care. 2016; 20:252. PMID: 27495247.
Article23. Hirji I, Guo Z, Andersson SW, Hammar N, Gomez-Caminero A. Incidence of urinary tract infection among patients with type 2 diabetes in the UK General Practice Research Database (GPRD). J Diabetes Complications. 2012; 26:513–516. PMID: 22889712.
Article24. Li W, Chen H, Wu S, Peng J. A comparison of pyogenic liver abscess in patients with or without diabetes: a retrospective study of 246 cases. BMC Gastroenterol. 2018; 18:144. PMID: 30285638.
Article25. Tian LT, Yao K, Zhang XY, Zhang ZD, Liang YJ, Yin DL, Lee L, Jiang HC, Liu LX. Liver abscesses in adult patients with and without diabetes mellitus: an analysis of the clinical characteristics, features of the causative pathogens, outcomes and predictors of fatality: a report based on a large population, retrospective study in China. Clin Microbiol Infect. 2012; 18:E314–E330. PMID: 22676078.
Article26. Lee CJ, Jung DS, Jung SH, Baik JH, Lee JH, Cho YR, Go BS, Lee SW, Han SY, Lee DH. Comparison of liver abscess between diabetic patients and non-diabetic patients. Korean J Hepatol. 2005; 11:339–349. PMID: 16380663.27. Zhang M, Pan L, Xu D, Cao C, Shi R, Han S, Liu J, Li X, Li M. The NFκB signaling pathway serves an important regulatory role in Klebsiella pneumoniae liver abscesses. Exp Ther Med. 2018; 15:5443–5449. PMID: 29904423.28. Jay CA, Solbrig MV. Neurologic infections in diabetes mellitus. Handb Clin Neurol. 2014; 126:175–194. PMID: 25410222.
Article29. Raya-Cruz M, Payeras-Cifre A, Ventayol-Aguilo L, Diaz-Antolin P. Factors associated with readmission and mortality in adult patients with skin and soft tissue infections. Int J Dermatol. 2019; 58:916–924. PMID: 30770547.
Article30. Hine JL, de Lusignan S, Burleigh D, Pathirannehelage S, McGovern A, Gatenby P, Jones S, Jiang D, Williams J, Elliot AJ, Smith GE, Brownrigg J, Hinchliffe R, Munro N. Association between glycaemic control and common infections in people with type 2 diabetes: a cohort study. Diabet Med. 2017; 34:551–557. PMID: 27548909.
Article31. Donnelly JP, Nair S, Griffin R, Baddley JW, Safford MM, Wang HE, Shapiro NI. Association of diabetes and insulin therapy with risk of hospitalization for infection and 28-day mortality risk. Clin Infect Dis. 2017; 64:435–442. PMID: 28174913.32. Song SO, Song YD, Nam JY, Park KH, Yoon JH, Son KM, Ko Y, Lim DH. Epidemiology of type 1 diabetes mellitus in Korea through an investigation of the national registration project of type 1 diabetes for the reimbursement of glucometer strips with additional analyses using claims data. Diabetes Metab J. 2016; 40:35–45. PMID: 26912154.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Exercise Frequency Reduction Is Associated With Higher Risk of Infection in Newly Diagnosed Diabetes: A Nationally Representative Cohort Study
- Increased Risk of Cardiovascular Disease and Mortality in Patients with Diabetes and Coexisting Depression: A Nationwide Population-Based Cohort Study (Diabetes Metab J 2021;45:379-89)
- Hypoglycemia and Dementia Risk in Older Patients with Type 2 Diabetes Mellitus: A Propensity-Score Matched Analysis of a Population-Based Cohort Study (Diabetes Metab J 2020;44:125-33)
- Hypoglycemia and Dementia Risk in Older Patients with Type 2 Diabetes Mellitus: A Propensity-Score Matched Analysis of a Population-Based Cohort Study (Diabetes Metab J 2020;44:125-33)
- Comparison of New-Onset Diabetes Mellitus among Patients with Atrial Fibrillation or Atrial Flutter