Yonsei Med J.
2016 Jan;57(1):225-231. 10.3349/ymj.2016.57.1.225.
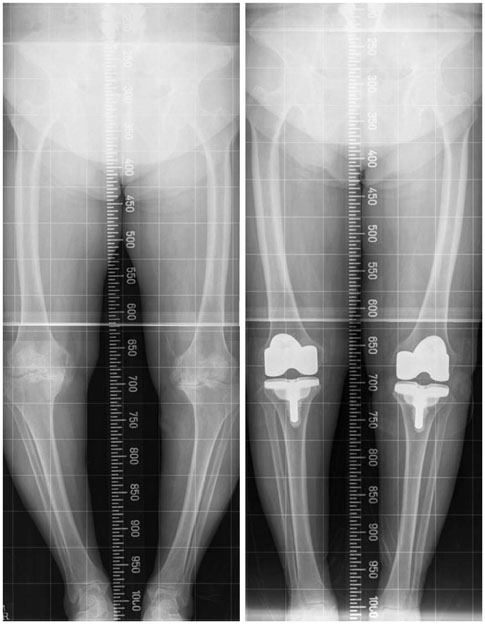
Radiologic Outcomes According to Varus Deformity in Minimally Invasive Surgery Total Knee Arthroplasty
- Affiliations
-
- 1Department of Orthopedic Surgery, National Health Insurance Service, Ilsan Hospital, Goyang, Korea. orthomania@gmail.com
- 2Department of Orthopedic Surgery, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2466374
- DOI: http://doi.org/10.3349/ymj.2016.57.1.225
Abstract
- PURPOSE
To identify the accuracy of postoperative implant alignment in minimally invasive surgery total knee arthroplasty (MIS-TKA), based on the degree of varus deformity.
MATERIALS AND METHODS
The research examined 627 cases of MIS-TKA from November 2005 to December 2007. The cases were categorized according to the preoperative degree of varus deformity in the knee joint in order to compare the postoperative alignment of the implant: less than 5degrees varus (Group 1, 351 cases), 5degrees to less than 10degrees varus (Group 2, 189 cases), 10degrees to less than 15degrees varus (Group 3, 59 cases), and 15degrees varus or more (Group 4, 28 cases).
RESULTS
On average, the alignment of the tibial implant was 0.2+/-1.4degrees, 0.1+/-1.3degrees, 0.1+/-1.6degrees, and 0.3+/-1.7degrees varus, and the tibiofemoral alignment was 5.2+/-1.9degrees, 4.7+/-1.9degrees, 4.9+/-1.9degrees, and 5.1+/-2.0degrees valgus for Groups 1, 2, 3, and 4, respectively, in the preoperative stage, indicating no difference between the groups (p>0.05). With respect to the accuracy of the tibial implant alignment, 98.1%, 97.6%, 87.5%, and 86.7% of Groups 1, 2, 3, and 4, respectively, had 0+/-3degrees varus angulation, demonstrating a reduced level of accuracy in Groups 3 and 4 (p<0.0001). There was no difference in terms of tibiofemoral alignment, with 83.9%, 82.9%, 85.4%, and 86.7% of each group, respectively, showing 6+/-3degrees valgus angulation (p>0.05).
CONCLUSION
Satisfactory component alignment was achieved in minimally invasive surgery in total knee arthroplasty, regardless of the degree of varus deformity.
MeSH Terms
-
Aged
Arthroplasty, Replacement, Knee/*methods
Bone Anteversion/complications/*radiography
Bone Malalignment/etiology/*radiography
Female
Humans
Joint Deformities, Acquired/*surgery
Knee Joint/radiography/*surgery
Knee Prosthesis
Male
Middle Aged
Minimally Invasive Surgical Procedures/*methods
Osteoarthritis, Knee/complications/radiography/*surgery
Postoperative Period
Preoperative Period
Range of Motion, Articular
Tibia/surgery
Treatment Outcome
Figure
Cited by 1 articles
-
Revision Arthroplasty Using a MUTARS® Prosthesis in Comminuted Periprosthetic Fracture of the Distal Femur
Hyung-Suk Choi, Jae-Hwi Nho, Chung-Hyun Kim, Sai-Won Kwon, Jong-Seok Park, You-Sung Suh
Yonsei Med J. 2016;57(6):1517-1522. doi: 10.3349/ymj.2016.57.6.1517.
Reference
-
1. Kelly MA, Clarke HD. Long-term results of posterior cruciate-substituting total knee arthroplasty. Clin Orthop Relat Res. 2002; 51–57.
Article2. Jonsson B, Aström J. Alignment and long-term clinical results of a semiconstrained knee prosthesis. Clin Orthop Relat Res. 1988; 124–128.
Article3. Ritter MA, Faris PM, Keating EM, Meding JB. Postoperative alignment of total knee replacement. Its effect on survival. Clin Orthop Relat Res. 1994; 153–156.
Article4. Repicci JA, Eberle RW. Minimally invasive surgical technique for unicondylar knee arthroplasty. J South Orthop Assoc. 1999; 8:20–27.5. Alan RK, Tria AJ Jr. Quadriceps-sparing total knee arthroplasty using the posterior stabilized TKA design. J Knee Surg. 2006; 19:71–76.
Article6. Bonutti PM, Zywiel MG, Seyler TM, Lee SY, McGrath MS, Marker DR, et al. Minimally invasive total knee arthroplasty using the contralateral knee as a control group: a case-control study. Int Orthop. 2010; 34:491–495.
Article7. Cheng T, Liu T, Zhang G, Peng X, Zhang X. Does minimally invasive surgery improve short-term recovery in total knee arthroplasty? Clin Orthop Relat Res. 2010; 468:1635–1648.
Article8. Juosponis R, Tarasevicius S, Smailys A, Kalesinskas RJ. Functional and radiological outcome after total knee replacement performed with mini-midvastus or conventional arthrotomy: controlled randomised trial. Int Orthop. 2009; 33:1233–1237.
Article9. King J, Stamper DL, Schaad DC, Leopold SS. Minimally invasive total knee arthroplasty compared with traditional total knee arthroplasty. Assessment of the learning curve and the postoperative recuperative period. J Bone Joint Surg Am. 2007; 89:1497–1503.
Article10. King JC, Manner PA, Stamper DL, Schaad DC, Leopold SS. Is minimally invasive total knee arthroplasty associated with lower costs than traditional TKA? Clin Orthop Relat Res. 2011; 469:1716–1720.
Article11. Pan WM, Li XG, Tang TS, Qian ZL, Zhang Q, Zhang CM. Mini-subvastus versus a standard approach in total knee arthroplasty: a prospective, randomized, controlled study. J Int Med Res. 2010; 38:890–900.
Article12. Barrack RL, Barnes CL, Burnett RS, Miller D, Clohisy JC, Maloney WJ. Minimal incision surgery as a risk factor for early failure of total knee arthroplasty. J Arthroplasty. 2009; 24:489–498.
Article13. Karachalios T, Giotikas D, Roidis N, Poultsides L, Bargiotas K, Malizos KN. Total knee replacement performed with either a mini-midvastus or a standard approach: a prospective randomised clinical and radiological trial. J Bone Joint Surg Br. 2008; 90:584–591.14. Lee MS, Yim MC, Wages JJ, Nakasone CK. Component alignment after minimally invasive total knee arthroplasty: results of the first 100 cases performed. J Arthroplasty. 2011; 26:926–930.
Article15. Martin A, Sheinkop MB, Langhenry MM, Widemschek M, Benesch T, von Strempel A. Comparison of two minimally invasive implantation instrument-sets for total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2010; 18:359–366.
Article16. Jeffery RS, Morris RW, Denham RA. Coronal alignment after total knee replacement. J Bone Joint Surg Br. 1991; 73:709–714.
Article17. Niki Y, Matsumoto H, Otani T, Enomoto H, Toyama Y, Suda Y. Accuracy of implant positioning for minimally invasive total knee arthroplasty in patients with severe varus deformity. J Arthroplasty. 2010; 25:381–386.
Article18. Chen AF, Alan RK, Redziniak DE, Tria AJ Jr. Quadriceps sparing total knee replacement. The initial experience with results at two to four years. J Bone Joint Surg Br. 2006; 88:1448–1453.19. Tsuji S, Tomita T, Fujii M, Laskin RS, Yoshikawa H, Sugamoto K. Is minimally invasive surgery-total knee arthroplasty truly less invasive than standard total knee arthroplasty? A quantitative evaluation. J Arthroplasty. 2010; 25:970–976.
Article20. Insall J, Scott WN, Ranawat CS. The total condylar knee prosthesis. A report of two hundred and twenty cases. J Bone Joint Surg Am. 1979; 61:173–180.
Article21. Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989; 13–14.
Article22. Hernández-Vaquero D, Suarez-Vazquez A, Iglesias-Fernandez S. Can computer assistance improve the clinical and functional scores in total knee arthroplasty? Clin Orthop Relat Res. 2011; 469:3436–3442.
Article23. Seo JG, Moon YW, Kim SM, Jo BC, Park SH. Easy identification of mechanical axis during total knee arthroplasty. Yonsei Med J. 2013; 54:1505–1510.
Article24. Ng VY, DeClaire JH, Berend KR, Gulick BC, Lombardi AV Jr. Improved accuracy of alignment with patient-specific positioning guides compared with manual instrumentation in TKA. Clin Orthop Relat Res. 2012; 470:99–107.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Minimally Invasive Quadriceps Sparing Total Knee Arthroplasty
- Windswept deformities of the knee are challenging to manage
- Preoperative Varus-Valgus Stress Angle Difference Is Valuable for Predicting the Extent of Medial Release in Varus Deformity during Total Knee Arthroplasty
- Total Knee Arthroplasty for Treating Valgus and Varus in the Knees of One Person
- Results of Primary Total Knee Arthroplasty in Osteoarthritis with Varus Thrust Knee and Severe Varus Deformity