J Korean Ophthalmol Soc.
2019 Dec;60(12):1250-1256. 10.3341/jkos.2019.60.12.1250.
Comparison of Intraocular Pressures Measured by the Corvis ST and Other Tonometers in Normal Eyes
- Affiliations
-
- 1Department of Ophthalmology, College of Medicine, The Catholic University, Seoul, Korea. younhea@hotmail.com
- KMID: 2466178
- DOI: http://doi.org/10.3341/jkos.2019.60.12.1250
Abstract
- PURPOSE
We compared the intraocular pressures (IOPs) measured by the Corvis ST (CST), Goldmann applanation tonometer (GAT), and Rebound tonometer (RBT) and correlated the measured IOPs with the corneal center thickness (CCT).
METHODS
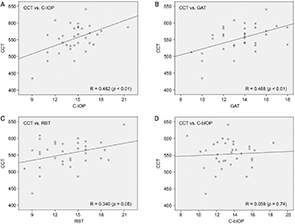
The IOPs were measured in 34 eyes of 34 normal subjects using the CST, GAT, and RBT by independent examiners. Comparisons between the IOPs measured by the CST and other tonometers were made using paired t-tests and Bland-Altman plots and Pearson's correlation coefficient was used to correlate the measured IOPs with the CCTs.
RESULTS
The IOP measured by the CST (C-IOP; 14.57 ± 2.37 mmHg) was significantly higher than that measured by the GAT(13.56 ± 2.25 mmHg) and RBT (13.57 ± 3.26 mmHg) (p < 0.05). The biomechanically corrected C-IOP (C-bIOP; 13.40 ± 2.06mmHg) showed no difference from the GAT-IOP and RBT-IOP (p > 0.50). In analyzing the correlation with CCT, RBT-IOP (R =0.34; p = 0.705) showed a lower correlation than the GAT-IOP (R = 0.49; p < 0.01) and C-IOP (R = 0.48; p < 0.01). The C-bIOP showed no correlation with the CCT (p = 0.74).
CONCLUSIONS
The IOP measurements using the C-IOP were significantly higher than the RBT-IOP and GAT-IOP but the C-bIOP showed no difference from the RBT-IOP and GAT-IOP. C-IOP, RBT-IOP, and GAT-IOP were significantly correlated with corneal thickness, but there was no correlation between CCT and C-bIOP. C-bIOP may therefore be considered clinically useful.
MeSH Terms
Figure
Reference
-
1. Coleman AL, Miglior S. Risk factors for glaucoma onset and progression. Surv Ophthalmol. 2008; 53 Suppl1:S3–S10.2. Gordon MO, Beiser JA, Brandt JD, et al. The ocular hypertension treatment study: baseline factors that predict the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002; 120:714–720. discussion 829-30.3. Leske MC, Heijl A, Hussein M, et al. Factors for glaucoma progression and the effect of treatment: the early manifest glaucoma trial. Arch Ophthalmol. 2003; 121:48–56.4. Leske MC, Heijl A, Hyman L, et al. Predictors of long-term progression in the early manifest glaucoma trial. Ophthalmology. 2007; 114:1965–1972.5. Liu J, Roberts CJ. Influence of corneal biomechanical properties on intraocular pressure measurement: quantitative analysis. J Cataract Refract Surg. 2005; 31:146–155.6. Jorge J, Fernandes P, Queirós A, et al. Comparison of the IOPen and iCare rebound tonometers with the Goldmann tonometer in a normal population. Ophthalmic Physiol Opt. 2010; 30:108–112.7. Fernandes P, Díaz-Rey JA, Queirós A, et al. Comparison of the ICare rebound tonometer with the Goldmann tonometer in a normal population. Ophthalmic Physiol Opt. 2005; 25:436–440.8. Lee H, Kang DSY, Ha BJ, et al. Biomechanical properties of the cornea using a dynamic scheimpflug analyzer in healthy eyes. Yonsei Med J. 2018; 59:1115–1122.9. Francis BA, Hsieh A, Lai MY, et al. Effects of corneal thickness, corneal curvature, and intraocular pressure level on Goldmann applanation tonometry and dynamic contour tonometry. Ophthalmology. 2007; 114:20–26.10. Jorge JM, González-Méijome JM, Queirós A, et al. Correlations between corneal biomechanical properties measured with the ocular response analyzer and ICare rebound tonometry. J Glaucoma. 2008; 17:442–448.11. Salim S, Du H, Wan J. Comparison of intraocular pressure measurements and assessment of intraobserver and interobserver reproducibility with the portable ICare rebound tonometer and Goldmann applanation tonometer in glaucoma patients. J Glaucoma. 2013; 22:325–329.12. Chui WS, Lam A, Chen D, Chiu R. The influence of corneal properties on rebound tonometry. Ophthalmology. 2008; 115:80–84.13. De Moraes CV, Hill V, Tello C, et al. Lower corneal hysteresis is associated with more rapid glaucomatous visual field progression. J Glaucoma. 2012; 21:209–213.14. Cho GE, Jun RM, Choi KR. Reproducibility of ocular response analyzer and comparison with Goldmann applanation tonometer and non-contact tonometer. J Korean Ophthalmol Soc. 2012; 53:1311–1317.15. Kanngiesser HE, Kniestedt C, Robert YC. Dynamic contour tonometry: presentation of a new tonometer. J Glaucoma. 2005; 14:344–350.16. Montard R, Kopito R, Touzeau O, et al. Ocular response analyzer: feasibility study and correlation with normal eyes. J Fr Ophtalmol. 2007; 30:978–984.17. Koprowski R. Automatic method of analysis and measurement of additional parameters of corneal deformation in the Corvis tonometer. Biomed Eng Online. 2014; 13:150.18. Chang DH, Stulting RD. Change in intraocular pressure measurements after LASIK the effect of the refractive correction and the lamellar flap. Ophthalmology. 2005; 112:1009–1016.19. Medeiros FA, Weinreb RN. Evaluation of the influence of corneal biomechanical properties on intraocular pressure measurements using the ocular response analyzer. J Glaucoma. 2006; 15:364–370.20. Knox Cartwright NE, Tyrer JR, Marshall J. Age-related differences in the elasticity of the human cornea. Invest Ophthalmol Vis Sci. 2011; 52:4324–4329.21. del Buey MA, Cristóbal JA, Ascaso FJ, et al. Biomechanical properties of the cornea in Fuchs' corneal dystrophy. Invest Ophthalmol Vis Sci. 2009; 50:3199–3202.22. Brettl S, Franko Zeitz P, Fuchsluger TA. Evaluation of corneal biomechanics in keratoconus using dynamic ultra-high-speed Scheimpflug measurements. Ophthalmologe. 2018; 115:644–648.23. Hugo J, Granget E, Ho Wang, et al. Intraocular pressure measurements and corneal biomechanical properties using a dynamic Scheimpflug analyzer, after several keratoplasty techniques, versus normal eyes. J Fr Ophtalmol. 2018; 41:30–38.24. Bhartiya S, Bali SJ, Sharma R, et al. Comparative evaluation of TonoPen AVIA, Goldmann applanation tonometry and non-contact tonometry. Int Ophthalmol. 2011; 31:297–302.25. Poostchi A, Mitchell R, Nicholas S, et al. The iCare rebound tonometer: comparisons with Goldmann tonometry, and influence of central corneal thickness. Clin Exp Ophthalmol. 2009; 37:687–691.26. Salouti R, Alishiri AA, Gharebaghi R, et al. Comparison among ocular response analyzer, Corvis ST and Goldmann applanation tonometry in healthy children. Int J Ophthalmol. 2018; 11:1330–1336.27. Han JW, Ha SJ. Comparison of Corvis ST tonometer to other tonometers and clinical usefulness of Corvis ST tonometer. J Korean Ophthalmol Soc. 2015; 56:404–412.28. Eliasy A, Chen KJ, Vinciguerra R, et al. Ex-vivo experimental validation of biomechanically-corrected intraocular pressure measurements on human eyes using the CorVis ST. Exp Eye Res. 2018; 175:98–102.29. Coudrillier B, Pijanka JK, Jefferys JL, et al. Glaucoma-related changes in the mechanical properties and collagen micro-architecture of the human sclera. PLoS One. 2015; 10:e0131396.30. Wu N, Chen Y, Yu X, et al. Changes in corneal biomechanical properties after long-term topical prostaglandin therapy. PLoS One. 2016; 11:e0155527.31. Bañeros-Rojas P, Martinez de la Casa JM, Arribas-Pardo P, et al. Comparison between Goldmann, Icare Pro and Corvis ST tonometry. Arch Soc Esp Oftalmol. 2014; 89:260–264.32. Valbon BF, Ambrósio R Jr, Fontes BM, Alves MR. Effects of age on corneal deformation by non-contact tonometry integrated with an ultra-high-speed (UHS) Scheimpflug camera. Arq Bras Oftalmol. 2013; 76:229–232.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Corvis ST Tonometer to Other Tonometers and Clinical Usefulness of Corvis ST Tonometer
- Analysis of Factors Affecting Corneal Deflection Amplitude in Normal Korean Eyes
- The Use of a Dynamic Scheimpflug Analyzer to Measure Changes of Post-keratoplasty Corneal Biomechanical Properties
- Comparison of the Noncontact Tonometer with Goldmann Tonometer
- Comparison of Intraocular Pressures According to Position Using Icare Rebound Tonometer