Arch Hand Microsurg.
2019 Dec;24(4):402-407. 10.12790/ahm.2019.24.4.402.
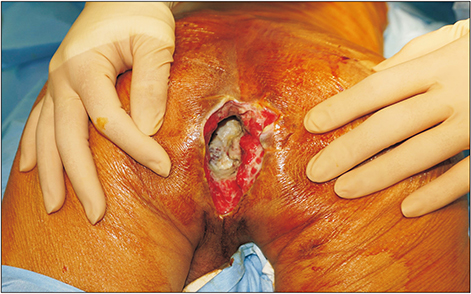
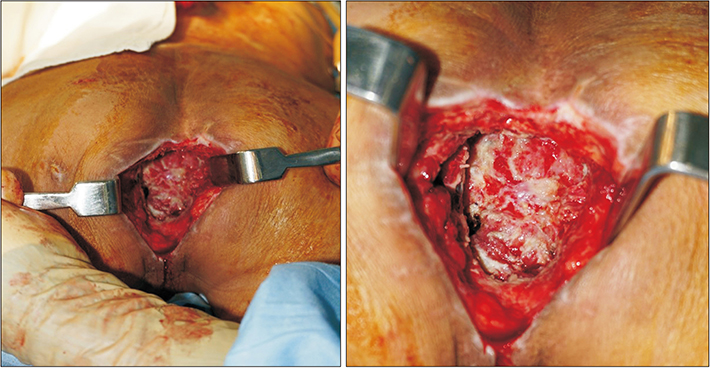
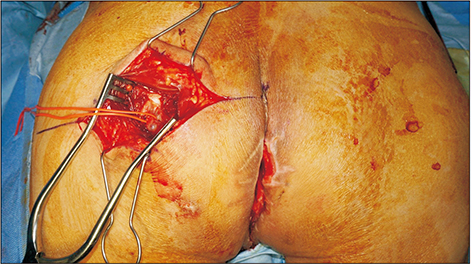
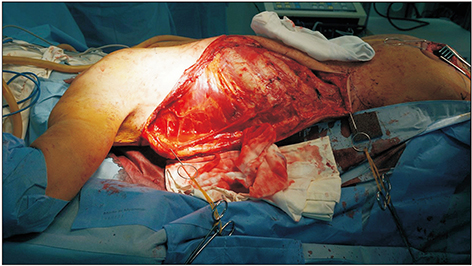
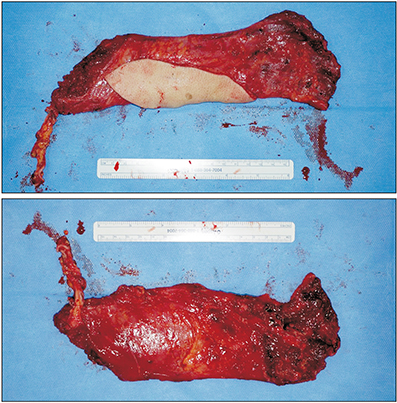
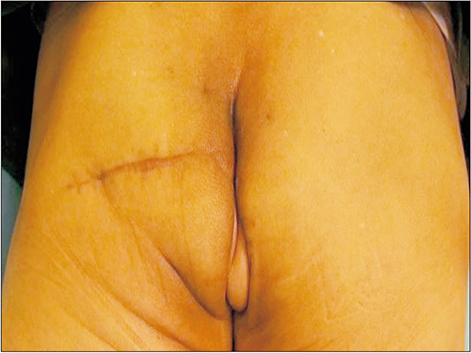
Radiation Induced Perineo-Coccygeal Defect Coverage with Latissimus Dorsi Musculocutaneous Free Flap
- Affiliations
-
- 1Department of Plastic and Reconstructive Surgery, Seoul National University College of Medicine, Seoul National University Bundang Hospital, Seongnam, Korea. sceun@snu.ac.kr
- KMID: 2464478
- DOI: http://doi.org/10.12790/ahm.2019.24.4.402
Abstract
- Perineal defect reconstruction is usually encountered in oncological conditions, trauma, or infection such as Fournier's gangrene. Reconstructive surgeons face challenges due to the complex structure and diversity of the different tissue and crucial organ components. In addition to innate characteristics, fecal contamination, difficulty of patient position to minimize trauma to the region, and suboptimal conditions for wound healing such as radiotherapy are other burdens to overcome. Common wound complications after perineal reconstruction are caused by remnant dead space, contamination, inadequate soft tissue volume, and chemoradiation-related entities after oncological resection. Classic methods such as direct closure or closure with local, regional, and distant pedicled flaps may often be unsuccessful. Free flap coverage has been reported to be successful, as the transferred tissue is outside the radiation field. We present a rare case of radiation-induced perineo-coccygeal defect covered with a free latissimus dorsi myocutaneous flap after abdominoperineal resection.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Latissimus dorsi and omental free flap reconstruction of a large buttock soft-tissue defect using the lateral circumflex femoral artery descending branch as the recipient vessel: a case report
Seungjun Lee, Seokchan Eun
Arch Hand Microsurg. 2025;30(1):66-73. doi: 10.12790/ahm.24.0064.
Reference
-
1. Brodbeck R, Horch RE, Arkudas A, Beier JP. Plastic and reconstructive surgery in the treatment of oncological perineal and genital defects. Front Oncol. 2015; 5:212.
Article2. Kolehmainen M, Suominen S, Tukiainen E. Pelvic, perineal and genital reconstructions. Scand J Surg. 2013; 102:25–31.
Article3. Artioukh DY, Smith RA, Gokul K. Risk factors for impaired healing of the perineal wound after abdominoperineal resection of rectum for carcinoma. Colorectal Dis. 2007; 9:362–367.
Article4. Anthony JP, Mathes SJ. The recalcitrant perineal wound after rectal extirpation. Applications of muscle flap closure. Arch Surg. 1990; 125:1371–1376. discussion 1376–7.5. Winterton RI, Lambe GF, Ekwobi C, et al. Gluteal fold flaps for perineal reconstruction. J Plast Reconstr Aesthet Surg. 2013; 66:397–405.
Article6. Onaitis MW, Noone RB, Hartwig M, et al. Neoadjuvant chemoradiation for rectal cancer: analysis of clinical outcomes from a 13-year institutional experience. Ann Surg. 2001; 233:778–785.
Article7. Di Benedetto G, Bertani A, Pallua N. The free latissimus dorsi flap revisited: a primary option for coverage of wide recurrent lumbosacral defects. Plast Reconstr Surg. 2002; 109:1960–1965.
Article8. Asko-Seljavaara S, Lähteenmäki T, Waris T, Sundell B. Comparison of latissimus dorsi and rectus abdominis free flaps. Br J Plast Surg. 1987; 40:620–628.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Reconstruction of an abdominal wall defect using a latissimus dorsi musculocutaneous free flap after high-intensity focused ultrasound: a case report
- V-Y Latissimus Dorsi Musculocutaneous Flap for Reconstruction of Radiation-induced Skin Injuries on the Back
- Reconstruction of Extensive Lower Extermity Soft Tissue Defect Using Free Latissimus Dorsi Muscle Flap with STSG
- Scalp Reconstruction and Cranioplasty using the Latissimus Dorsi Musculocutaneous Flap in a Patient with Recurrent Wound Dehiscence Accompanied by MRSA Infection
- Reconstruction of Midface Defect with Latissimus Dorsi Myocutaneous Free Flap