Arch Hand Microsurg.
2019 Dec;24(4):381-387. 10.12790/ahm.2019.24.4.381.
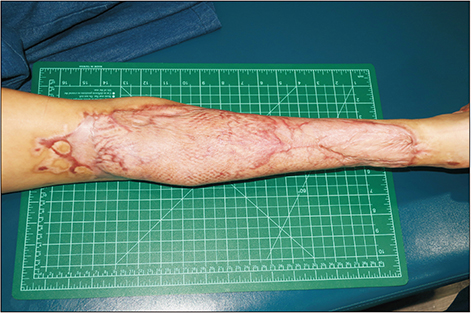
Salvage Procedure of a Lower Leg in a Contact Burn: Latissimus Dorsi Muscle Free Flap and Scalp Skin Graft
- Affiliations
-
- 1Department of Burn Reconstructive Surgery, Bestian Seoul Hospital, Seoul, Korea. sjoh46@nate.com
- 2Department of Burn Surgery, Bestian Seoul Hospital, Seoul, Korea.
- KMID: 2464475
- DOI: http://doi.org/10.12790/ahm.2019.24.4.381
Abstract
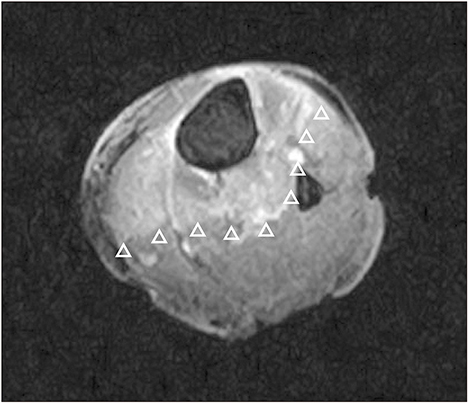
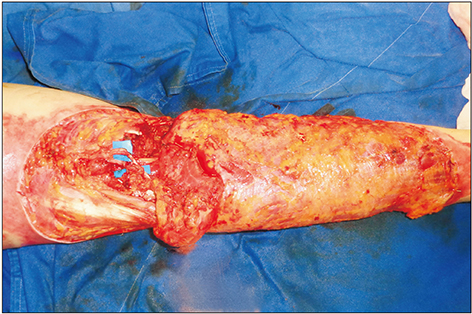
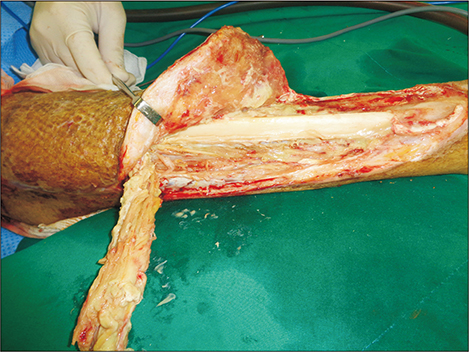
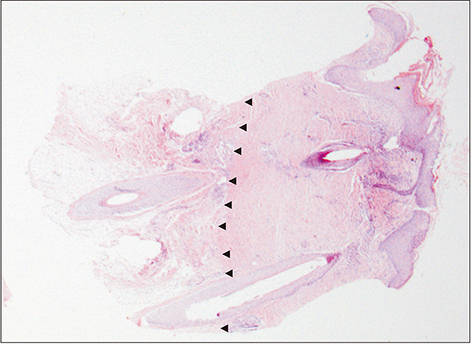
- Intentional carbon monoxide (CO) poisoning has become rapidly increased occurrence, also if the surviving patient is burnt and unconscious, the patient's burn wound is likely to be severely deep and to need flap surgery. A 44-year-old female patient suffered from a deep contact burn to the left posterior lower leg during intentional CO poisoning. The patient underwent escharotomy and treatment with a latissimus dorsi muscle neuro-vascularized free flap and scalp skin grafts. While harvesting 0.008 inches (300 cm²) of the scalp skin, some 25 cm² of the skin was accidentally harvested as a thick split-thickness skin graft (SSG) from the right occipital scalp. Interfollicular epidermal and dermal regeneration was achieved at eleven days postoperatively at the thick SSG donor site. The patient's deep burn wound was reconstructed by two staged surgeries. The patient was able to walk with the help of a supportive shoe one year postoperatively.
Keyword
MeSH Terms
Figure
Reference
-
1. Chang SS, Chen YY, Yip PS, Lee WJ, Hagihara A, Gunnell D. Regional changes in charcoal-burning suicide rates in East/Southeast Asia from 1995 to 2011: a time trend analysis. PLoS Med. 2014; 11:e1001622.
Article2. Choi YR, Cha ES, Chang SS, Khang YH, Lee WJ. Suicide from carbon monoxide poisoning in South Korea: 2006-2012. J Affect Disord. 2014; 167:322–325.
Article3. Chai J, Song H, Sheng Z, Chen B, Yang H, Li L. Repair and reconstruction of massively damaged burn wounds. Burns. 2003; 29:726–732.
Article4. Rednam RS, Rinker BD. Reconstruction of posterior compartment of lower extremity using a functional latissimus dorsi free flap: a case report. Microsurgery. 2016; 36:77–80.
Article5. Crawford BS. An unusual skin donor site. Br J Plast Surg. 1964; 17:311–313.
Article6. Gyger D, Genin B, Bugmann P, Lironi A, Coultre CL. Skin harvesting on the scalp in children: utopia or reality. Eur J Pediatr Surg. 1996; 6:166–169.
Article7. Weyandt GH, Bauer B, Berens N, Hamm H, Broecker EB. Split-skin grafting from the scalp: the hidden advantage. Dermatol Surg. 2009; 35:1873–1879.8. Chang LY, Yang JY, Chuang SS, Hsiao CW. Use of the scalp as a donor site for large burn wound coverage: review of 150 patients. World J Surg. 1998; 22:296–299. discussion 299-300.
Article9. Malpass KG, Snelling CF, Tron V. Comparison of donorsite healing under Xeroform and Jelonet dressings: unexpected findings. Plast Reconstr Surg. 2003; 112:430–439.
Article10. McBride CA, Kempf M, Kimble RM, Stockton K. Variability in split-thickness skin graft depth when using an air-powered dermatome: a paediatric cohort study. Burns. 2017; 43:1552–1560.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Neovascularization in the "Cross-Leg Fashioned" Muscular Free Flap
- Reconstruction of Extensive Lower Extermity Soft Tissue Defect Using Free Latissimus Dorsi Muscle Flap with STSG
- Reconstruction of Knee in Long - term Flexion Contracture Using Latissimus Dorsi Flap
- Reconstruction of Midface Defect with Latissimus Dorsi Myocutaneous Free Flap
- A Retrospective Study for Method and Timing of Reconstruction Using Free Latissimus Dorsi Muscle Flap at Foot in Electrical Burn Patients