Clin Orthop Surg.
2019 Dec;11(4):474-481. 10.4055/cios.2019.11.4.474.
Diagnosis and Management of Hip Dislocation in Patients with Kabuki Syndrome
- Affiliations
-
- 1Division of Pediatric Orthopaedics, Seoul National University Children's Hospital, Seoul, Korea. tjcho@snu.ac.kr
- 2Department of Orthopedic Surgery, Chonnam National University Hospital, Gwangju, Korea.
- 3Department of Orthopedic Surgery, Seoul National University Bundang Hospital, Seongnam, Korea.
- 4Department of Pediatrics, Seoul National University Children's Hospital, Seoul, Korea.
- KMID: 2462543
- DOI: http://doi.org/10.4055/cios.2019.11.4.474
Abstract
- BACKGROUND
Kabuki syndrome is a rare genetic disorder characterized by distinct dysmorphic facial features, growth deficiency, intellectual disabilities, unusual dermatoglyphic patterns, and skeletal abnormalities. The incidence of hip dislocation in Kabuki syndrome ranges from 18% to 62%. We reviewed the outcomes of management of hip dislocations in patients with Kabuki syndrome with special attention to the diagnostic processes for hip dislocation and Kabuki syndrome.
METHODS
Among 30 patients with mutation-confirmed Kabuki syndrome, we selected six patients who had hip dislocations and reviewed their medical records and plain radiographs. The modes of presentation and diagnostic processes for both hip dislocations and Kabuki syndrome were investigated. The management and treatment outcomes of hip dislocations in patients with Kabuki syndrome were evaluated.
RESULTS
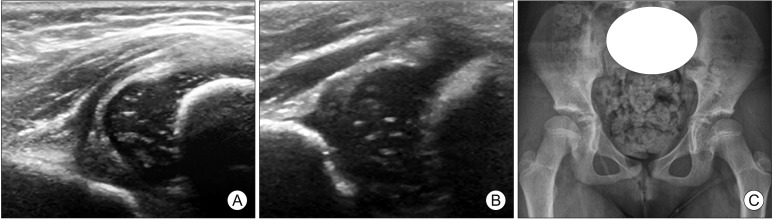
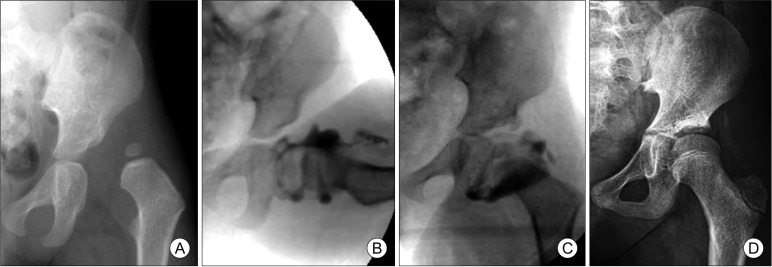
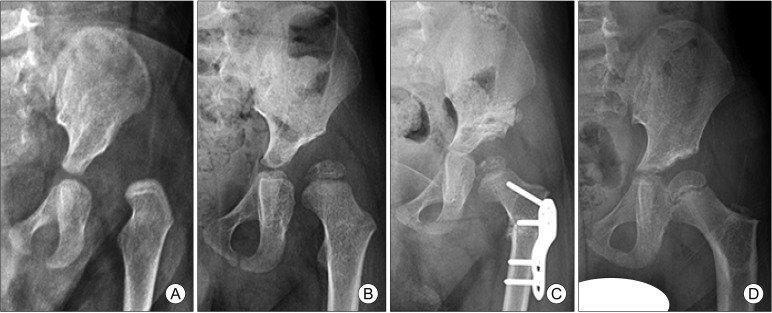
The average age of patients at the time of diagnosis of hip dislocation was 7.7 months (range, 1 week to 22 months). None of the patients were diagnosed as having Kabuki syndrome at that time. Two patients were treated with a Pavlik harness; one, with closed reduction; two, with open reduction and later pelvic and/or femoral osteotomies; and one, with open reduction combined with pelvic osteotomy. The patients were followed up for 5.8 years on average (range, 2.0 to 10.5 years). The radiologic outcome was graded as Severin IA or IB for three patients who were older than 6 years at the latest follow-up (mean age, 9.9 years; range, 7.8 to 12.4 years). In the remaining three patients younger than 6 years (mean age, 3.8 years; range, 2.7 to 5.3 years), the lateral center edge angle was more than 15°. The clinical diagnosis of Kabuki syndrome was made during follow-up after hip dislocation treatment and confirmed by mutational analysis at a mean age of 4.7 years. The mean interval between the diagnosis of hip dislocation and Kabuki syndrome was 4.0 years.
CONCLUSIONS
The management of hip dislocation by conservative or surgical method showed successful results. Awareness of Kabuki syndrome could lead to an early diagnosis of this rare disease in patients with hip dislocation and allow for early detection of other underlying conditions and multidisciplinary management.
Keyword
MeSH Terms
Figure
Reference
-
1. Niikawa N, Matsuura N, Fukushima Y, Ohsawa T, Kajii T. Kabuki make-up syndrome: a syndrome of mental retardation, unusual facies, large and protruding ears, and postnatal growth deficiency. J Pediatr. 1981; 99(4):565–569. PMID: 7277096.2. Kuroki Y, Suzuki Y, Chyo H, Hata A, Matsui I. A new malformation syndrome of long palpebral fissures, large ears, depressed nasal tip, and skeletal anomalies associated with postnatal dwarfism and mental retardation. J Pediatr. 1981; 99(4):570–573. PMID: 7277097.3. Niikawa N, Kuroki Y, Kajii T, et al. Kabuki make-up (Niikawa-Kuroki) syndrome: a study of 62 patients. Am J Med Genet. 1988; 31(3):565–589. PMID: 3067577.4. Philip N, Meinecke P, David A, et al. Kabuki make-up (Niikawa-Kuroki) syndrome: a study of 16 non-Japanese cases. Clin Dysmorphol. 1992; 1(2):63–77. PMID: 1285376.5. Schrander-Stumpel C, Meinecke P, Wilson G, et al. The Kabuki (Niikawa-Kuroki) syndrome: further delineation of the phenotype in 29 non-Japanese patients. Eur J Pediatr. 1994; 153(6):438–445. PMID: 8088300.
Article6. Banka S, Veeramachaneni R, Reardon W, et al. How genetically heterogeneous is Kabuki syndrome?: MLL2 testing in 116 patients, review and analyses of mutation and phenotypic spectrum. Eur J Hum Genet. 2012; 20(4):381–388. PMID: 22126750.
Article7. Li Y, Bogershausen N, Alanay Y, et al. A mutation screen in patients with Kabuki syndrome. Hum Genet. 2011; 130(6):715–724. PMID: 21607748.
Article8. Ng SB, Bigham AW, Buckingham KJ, et al. Exome sequencing identifies MLL2 mutations as a cause of Kabuki syndrome. Nat Genet. 2010; 42(9):790–793. PMID: 20711175.9. Bogershausen N, Wollnik B. Unmasking Kabuki syndrome. Clin Genet. 2013; 83(3):201–211. PMID: 23131014.10. Lintas C, Persico AM. Unraveling molecular pathways shared by Kabuki and Kabuki-like syndromes. Clin Genet. 2018; 94(3-4):283–295. PMID: 28139835.
Article11. Hinrichs B, Gramss B, Meinecke P. Defective clavicles in Kabuki syndrome. Genet Couns. 2002; 13(4):477–479. PMID: 12558121.12. Ikegawa S, Sakaguchi R, Kimizuka M, Yanagisako Y, Tokimura F. Recurrent dislocation of the patella in Kabuki make-up syndrome. J Pediatr Orthop. 1993; 13(2):265–267. PMID: 8459025.13. Kurosawa K, Kawame H, Ochiai Y, Nakashima M, Tohma T, Ohashi H. Patellar dislocation in Kabuki syndrome. Am J Med Genet. 2002; 108(2):160–163. PMID: 11857567.
Article14. Phillips S, Hemmady S, Thomas P, ODoherty D. Kabuki syndrome presenting with congenital talipes equinovarus. J Pediatr Orthop B. 2005; 14(4):285–286. PMID: 15931034.15. Ramachandran M, Kay RM, Skaggs DL. Treatment of hip dislocation in Kabuki syndrome: a report of three hips in two patients. J Pediatr Orthop. 2007; 27(1):37–40. PMID: 17195795.16. Wada A, Nakamura T, Yamaguchi T, et al. Surgical treatment of hip dislocation in Kabuki syndrome: use of incomplete periacetabular osteotomy for posterior acetabular wall deficiency. J Child Orthop. 2012; 6(4):261–267. PMID: 23904891.
Article17. Chung CY, Park MS, Choi IH, Cho TJ, Yoo WJ, Lee KM. Morphometric analysis of acetabular dysplasia in cerebral palsy. J Bone Joint Surg Br. 2006; 88(2):243–247. PMID: 16434532.
Article18. Chung CY, Choi IH, Cho TJ, Yoo WJ, Lee SH, Park MS. Morphometric changes in the acetabulum after Dega osteotomy in patients with cerebral palsy. J Bone Joint Surg Br. 2008; 90(1):88–91. PMID: 18160506.
Article19. Kim HT, Jang JH, Ahn JM, Lee JS, Kang DJ. Early results of one-stage correction for hip instability in cerebral palsy. Clin Orthop Surg. 2012; 4(2):139–148. PMID: 22662300.
Article20. Aly AS, Al-Kersh MA. Femoral and Dega osteotomies in the treatment of habitual hip dislocation in Down syndrome patients: is it efficient or not? J Child Orthop. 2018; 12(3):227–231. PMID: 29951121.21. Beighton P, Horan F. Orthopaedic aspects of the Ehlers-Danlos syndrome. J Bone Joint Surg Br. 1969; 51(3):444–453. PMID: 5820785.22. Badelon O, Bensahel H, Csukonyi Z, Chaumien JP. Congenital dislocation of the hip in Ehlers-Danlos syndrome. Clin Orthop Relat Res. 1990; (255):138–143.
Article23. Giunta C, Superti-Furga A, Spranger S, Cole WG, Steinmann B. Ehlers-Danlos syndrome type VII: clinical features and molecular defects. J Bone Joint Surg Am. 1999; 81(2):225–238. PMID: 10073586.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Phenotypic and Cytogenetic Delineation of Six Korean Children with Kabuki Syndrome
- Strabismus and Poor Stereoacuity Associated with Kabuki Syndrome
- The Treatment of Bilateral Congenital Dislocation of the Hip
- Intertrochanteric fracture associated with posterior hip dislocation
- Surgical Treatment of Pathological Dislocation of Child Hip After Acute Osteomyelitis of Ilium