Ann Surg Treat Res.
2019 Nov;97(5):261-265. 10.4174/astr.2019.97.5.261.
Inverse ‘D’ incision technique in treatment of pilonidal sinus disease; excision with minimal tissue loss, closure without tension and lateral location of the suture line
- Affiliations
-
- 1Department of Surgery, Duzce University Medical Faculty, Duzce, Turkey. samidogan@hotmail.com
- KMID: 2461902
- DOI: http://doi.org/10.4174/astr.2019.97.5.261
Abstract
- PURPOSE
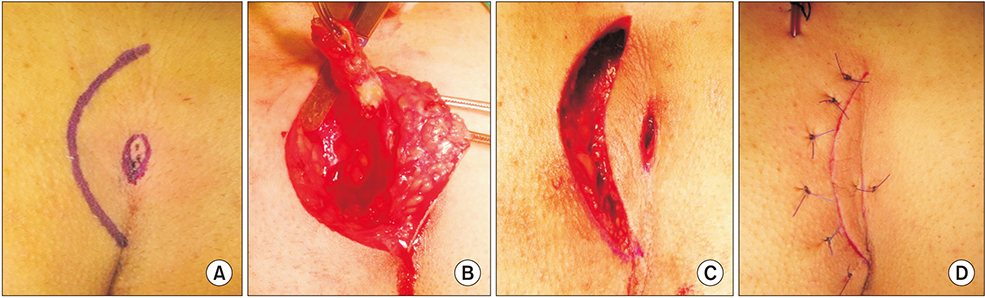
Surgical excision is the preferred treatment modality for sacrococcygeal pilonidal sinus (PS). Notably, the desirable features of an ideal surgical intervention are excision with minimal tissue loss, closure without tension, and a lateral suture line. The present study aimed to investigate early outcomes of surgical excision through the inverse D (á—¡) incision based on tissue loss, wound tension, and suture line location.
METHODS
This prospective study was comprised of 80 patients with PS in whom excision of PS was performed through the "˜á—¡' incision to minimize tissue loss with a tensionless primary surgical wound closure. The suture line was located laterally in all patients. Early and late postoperative complications, duration of hospital stay, return to work, and recurrence rates were investigated. The mean duration of the follow-up period was 36 months.
RESULTS
Sixty-three patients (78.8%) were male. PS in all patients was surgically removed by subcutaneous excision through a "˜á—¡' incision. Laterally placed surgical wounds were closed primarily with interrupted vertical mattress sutures. No general complications were encountered. Five patients (6.3%) experienced early postoperative surgical site complications. On average, the duration of hospital stay and return to work were 2.4 days and 3.8 days, respectively. Recurrence was seen in 1 case (1.3%) during the follow-up period. Satisfaction score was high in 83.8% of patients.
CONCLUSION
The method of sinus excision using the "˜á—¡' incision with a primary suture facilitates excision with minimal tissue loss and closure without tension with an off-midline suture. It is both a simple and effective surgical technique for the treatment of sacrococcygeal PS.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Unroofing curettage for treatment of simple and complex sacrococcygeal pilonidal disease
Engin Olcucuoglu, Alpaslan Şahin
Ann Surg Treat Res. 2022;103(4):244-251. doi: 10.4174/astr.2022.103.4.244.
Reference
-
1. Steele SR, Perry WB, Mills S, Buie WD. Standards Practice Task Force of the American Society of Colon and Rectal Surgeons. Practice parameters for the management of pilonidal disease. Dis Colon Rectum. 2013; 56:1021–1027.
Article2. de Parades V, Bouchard D, Janier M, Berger A. Pilonidal sinus disease. J Visc Surg. 2013; 150:237–247.
Article3. Cheetham M. Lateral incision surgery for pilonidal sinus: death of a dogma. World J Surg. 2012; 36:436.
Article4. Sewefy AM, Hassanen A, Atyia AM, Saleh SK. Karydakis flap with compressing tieover interrupted sutures without drain versus standard karydakis for treatment of sacrococcygeal pilonidal sinus disease. Dis Colon Rectum. 2017; 60:514–520.
Article5. Iesalnieks I, Deimel S, Schlitt HJ. “Pit picking” surgery for patients with pilonidal disease: mid-term results and risk factors. Chirurg. 2015; 86:482–485.6. Iesalnieks I, Ommer A, Petersen S, Doll D, Herold A. German national guideline on the management of pilonidal disease. Langenbecks Arch Surg. 2016; 401:599–609.
Article7. Cetin K, Sikar HE, Kocaoglu AE, Kundes MF, Karahan M, Kaptanoglu L. Evaluation of intradermal absorbable and mattress sutures to close pilonidal sinus wounds with Limberg flap: a prospective randomized comparative study. Ann Surg Treat Res. 2018; 94:88–93.
Article8. Giarratano G, Toscana C, Shalaby M, Buonomo O, Petrella G, Sileri P. Endoscopic pilonidal sinus treatment: longterm results of a prospective series. JSLS. 2017; 21(3):e2017.00043. DOI: 10.4293/JSLS.2017.00043.
Article9. Suarez Valladares MJ, Rodriguez Prieto MA. Neodymium-doped yttrium aluminium garnet laser to treat primary pilonidal cysts: an alternative treatment. Br J Dermatol. 2018; 178:e127–e128.
Article10. Di Castro A, Guerra F, Levi Sandri GB, Ettorre GM. Minimally invasive surgery for the treatment of pilonidal disease. The Gips procedure on 2347 patients. Int J Surg. 2016; 36(Pt A):201–205.
Article11. Milone M, Fernandez LM, Musella M, Milone F. Safety and efficacy of minimally invasive video-assisted ablation of pilonidal sinus: a randomized clinical trial. JAMA Surg. 2016; 151:547–553.12. Hap W, Frejlich E, Rudno-Rudzinska J, Kotulski K, Kurnol K, Hap K, et al. Pilonidal sinus: finding the righttrack for treatment. Pol Przegl Chir. 2017; 89:68–75.
Article13. Dessily M, Charara F, Ralea S, Alle JL. Pilonidal sinus destruction with a radial laser probe: technique and first Belgian experience. Acta Chir Belg. 2017; 117:164–168.
Article14. Tezel E. A new classification according to navicular area concept for sacrococcygeal pilonidal disease. Colorectal Dis. 2007; 9:575–576.
Article15. Speter C, Zmora O, Nadler R, Shinhar D, Bilik R. Minimal incision as a promising technique for resection of pilonidal sinus in children. J Pediatr Surg. 2017; 52:1484–1487.
Article16. Soll C, Dindo D, Steinemann D, Hauffe T, Clavien PA, Hahnloser D. Sinusectomy for primary pilonidal sinus: less is more. Surgery. 2011; 150:996–1001.
Article17. Brusciano L, Limongelli P, Del Genio G, Tolone S, Amoroso V, Docimo G, et al. D-shape asymmetric excision of sacrococcygeal pilonidal sinus with primary closure, suction drain, and subcuticular skin closure: an analysis of risks factors for long-term recurrence. Surg Innov. 2015; 22:143–148.18. Zorlu M, Sahiner IT, Zobacı E, Kocak C, Yastı AC, Dolapcı M. Early results with the Mutaf technique: a novel off-midline approach in pilonidal sinus surgery. Ann Surg Treat Res. 2016; 90:265–271.
Article19. Kose E, Hasbahceci M, Tonyali H, Karagulle M. Comparative analysis of the same technique-the same surgeon approach in the surgical treatment of pilonidal sinus disease: a retrospective cohort study. Ann Surg Treat Res. 2017; 93:82–87.
Article20. McCallum I, King PM, Bruce J. Healing by primary versus secondary intention after surgical treatment for pilonidal sinus. Cochrane Database Syst Rev. 2007; (4):CD006213.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Evaluation of Wide Excision and Simple Primary Closure of Pilonidal Sinus
- A Case of Pilonidal Sinus Mimicking Inflammatory Epidermal Cyst
- Pilonidal Cysts Occurring in the Sacrococcygeal Region and that were Misdiagnosed as a Simple Abscess
- Comparative analysis of the same technique-the same surgeon approach in the surgical treatment of pilonidal sinus disease: a retrospective cohort study
- The Reduction and Fixation in Periorbital Bone Fracture via the Supratarsal Fold Incision