J Korean Ophthalmol Soc.
2019 Sep;60(9):843-850. 10.3341/jkos.2019.60.9.843.
The Effect of Epiretinal Membrane on Dexamethasone Implant for Branch Retinal Vein Occlusion Macular Edema
- Affiliations
-
- 1Department of Ophthalmology, Jeju National University School of Medicine, Jeju, Korea. righthanded8282@gmail.com
- 2Department of Ophthalmology, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2459128
- DOI: http://doi.org/10.3341/jkos.2019.60.9.843
Abstract
- PURPOSE
To evaluate the effect of epiretinal membrane (ERM) on the outcomes of intravitreal dexamethasone implant (Ozurdex®, Allergan, Irvine, CA, USA) treatment for macular edema (ME) secondary to branch retinal vein occlusion (BRVO).
METHODS
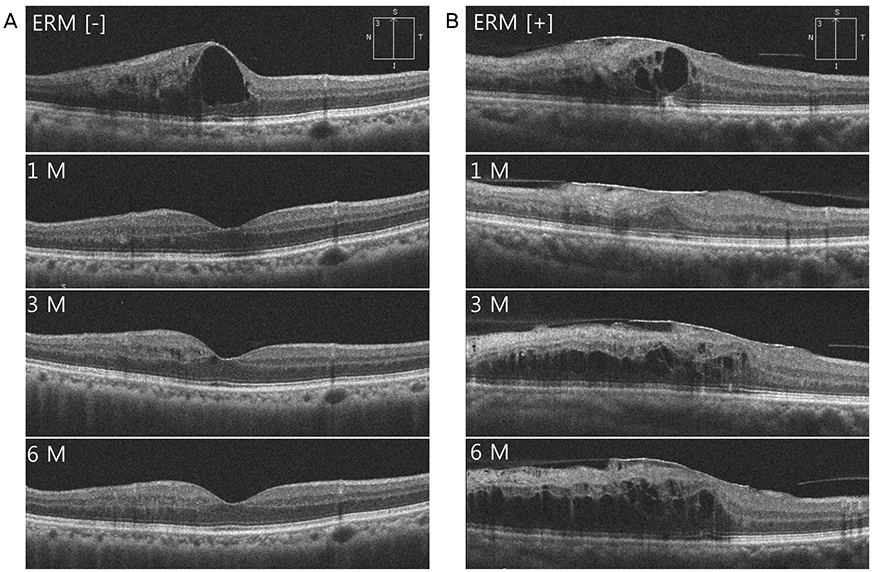
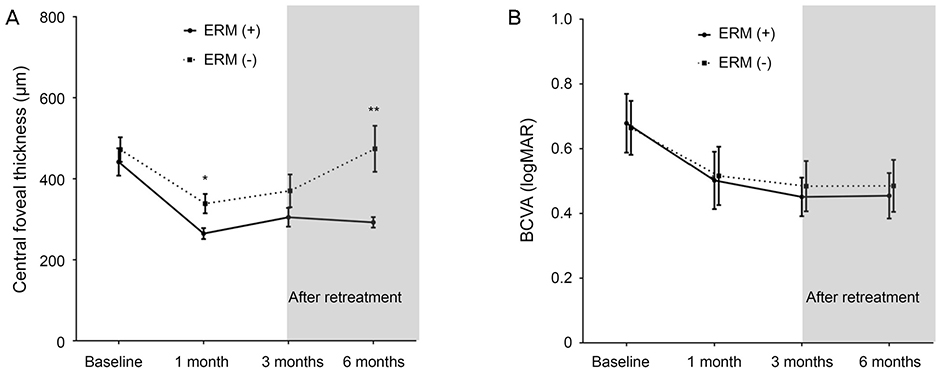
Thirty eyes of 30 patients who received Ozurdex treatment for ME secondary to BRVO, and were followed-up for at least 6 months were retrospectively reviewed. Patients were divided into two groups based on the presence (ERM [+] or absence ERM [−]) of ERM at baseline. The best-corrected visual acuity (BCVA), central foveal thickness (CFT), recurrence of ME, and retreatment rate were evaluated at baseline, 1, 3, and 6 months after Ozurdex injection.
RESULTS
Ten eyes of 30 eyes (33%) showed ERM at baseline. While the mean CFT was significantly reduced at 1 month after Ozurdex injection, it began to increase gradually thereafter in both groups. The ERM (+) group showed a significantly higher mean CFT than the corresponding values of the ERM (−) group at 1 (p = 0.022) and 6 months (p = 0.001) after Ozurdex injection. However, no significant difference was found in the BCVA between the two groups at every visit. The proportion of eyes with ME was significantly higher in the ERM (+) group (90%) than that in the ERM (−) group (35%) at 6 months after Ozurdex injection (p = 0.009). There were no significant differences between the two groups in the percentage of retreatment, time to retreatment, and type of materials used for retreatment.
CONCLUSIONS
In patients with ME secondary to BRVO, the treatment effect of Ozurdex was low and the duration of treatment was short when ERM was concurrently present. However, the presence of ERM did not significantly affect visual outcomes after treatment with Ozurdex.
Keyword
MeSH Terms
Figure
Reference
-
1. Orth DH, Patz A. Retinal branch vein occlusion. Surv Ophthalmol. 1978; 22:357–376.
Article2. Zhao J, Sastry SM, Sperduto RD, et al. Arteriovenous crossing patterns in branch retinal vein occlusion. The Eye Disease Case-Control Study Group. Ophthalmology. 1993; 100:423–428.3. Weinberg D, Dodwell DG, Fern SA. Anatomy of arteriovenous crossings in branch retinal vein occlusion. Am J Ophthalmol. 1990; 109:298–302.
Article4. The Branch Vein Occlusion Study Group. Argon laser photocoagulation for macular edema in branch vein occlusion. Am J Ophthalmol. 1984; 98:271–282.5. Pe'er J, Folberg R, Itin A, et al. Vascular endothelial growth factor upregulation in human central retinal vein occlusion. Ophthalmology. 1998; 105:412–416.6. Coscas G, Loewenstein A, Augustin A, et al. Management of retinal vein occlusion--consensus document. Ophthalmologica. 2011; 226:4–28.7. Glacet-Bernard A, Coscas G, Zourdani A, et al. Steroids and macular edema from retinal vein occlusion. Eur J Ophthalmol. 2011; 21 Suppl 6:S37–S44.8. Haller JA, Bandello F, Belfort R Jr, et al. Randomized, sham-controlled trial of dexamethasone intravitreal implant in patients with macular edema due to retinal vein occlusion. Ophthalmology. 2010; 117:1134–1146.e3.
Article9. Chatziralli I, Stavrakas P, Theodossiadis G, et al. The impact of epiretinal membrane in neovascular age-related macular degeneration treatment: a spectral-domain optical coherence tomography study. Semin Ophthalmol. 2018; 33:651–656.
Article10. Kulikov AN, Sosnovskii SV, Berezin RD, et al. Vitreoretinal interface abnormalities in diabetic macular edema and effectiveness of anti-VEGF therapy: an optical coherence tomography study. Clin Ophthalmol. 2017; 11:1995–2002.
Article11. Hayreh SS, Zimmerman MB. Fundus changes in branch retinal vein occlusion. Retina. 2015; 35:1016–1027.
Article12. Mitchell P, Smith W, Chey T, et al. Prevalence and associations of epiretinal membranes. The Blue Mountains Eye Study, Australia. Ophthalmology. 1997; 104:1033–1040.13. Marticorena J, Romano MR, Heimann H, et al. Intravitreal bevacizumab for retinal vein occlusion and early growth of epiretinal membrane: a possible secondary effect? Br J Ophthalmol. 2011; 95:391–395.
Article14. Stevenson W, Prospero Ponce CM, Agarwal DR, et al. Epiretinal membrane: optical coherence tomography-based diagnosis and classification. Clin Ophthalmol. 2016; 10:527–534.
Article15. Sugar EA, Jabs DA, Altaweel MM, et al. Identifying a clinically meaningful threshold for change in uveitic macular edema evaluated by optical coherence tomography. Am J Ophthalmol. 2011; 152:1044–1052.e5.
Article16. Gass J. Macular dysfunction caused by epiretinal membrane contraction. In : Gass JDM, editor. Stereoscopic Atlas of Macular Diseases: Diagnosis and Treatment. 4th ed. St. Louis: Mosby;1997. p. 938–951. v. 2.17. Boyer DS, Yoon YH, Belfort R Jr, et al. Three-year, randomized, sham-controlled trial of dexamethasone intravitreal implant in patients with diabetic macular edema. Ophthalmology. 2014; 121:1904–1914.
Article18. Myung JS, Aaker GD, Kiss S. Treatment of noninfectious posterior uveitis with dexamethasone intravitreal implant. Clin Ophthalmol. 2010; 4:1423–1426.19. Zhao F, Gandorfer A, Haritoglou C, et al. Epiretinal cell proliferation in macular pucker and vitreomacular traction syndrome: analysis of flat-mounted internal limiting membrane specimens. Retina. 2013; 33:77–88.20. Cho HJ, Kim JM, Kim HS, et al. Effect of epiretinal membranes on antivascular endothelial growth factor treatment for neovascular age-related macular degeneration. J Ocul Pharmacol Ther. 2017; 33:452–458.
Article21. Wong Y, Steel DHW, Habib MS, et al. Vitreoretinal interface abnormalities in patients treatedwith ranibizumab for diabetic macular oedema. Graefes Arch Clin Exp Ophthalmol. 2017; 255:733–742.
Article22. Lee SJ, Koh HJ. Effects of vitreomacular adhesion on anti-vascular endothelial growth factor treatment for exudative age-related macular degeneration. Ophthalmology. 2011; 118:101–110.
Article23. Nomura Y, Takahashi H, Tan X, et al. Effects of vitreomacular adhesion on ranibizumab treatment in Japanese patients with age-related macular degeneration. Jpn J Ophthalmol. 2014; 58:443–447.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Vitrectomy on the Complication of Branch Retinal Vein Occlusion
- The Clinical Study of Retinal Detachment Associated with B ranch Retinal Vein Occlusion
- Clinical Aspect of Branch Retinal Vein Occlusion
- Clinical Evaluation for Branch Retinal Vein Occlusion
- A Case of Retinal Hemorrhage Following a Dexamethasone Intravitreal Implant