Chonnam Med J.
2018 Jan;54(1):1-9. 10.4068/cmj.2018.54.1.1.
Molecular Diagnosis of Tuberculosis
- Affiliations
-
- 1Department of Pulmonology and Respiratory Medicine, Universitas Indonesia Faculty of Medicine, Persahabatan Hospital, Jakarta, Indonesia. fariz.nurwidya@gmail.com
- KMID: 2458578
- DOI: http://doi.org/10.4068/cmj.2018.54.1.1
Abstract
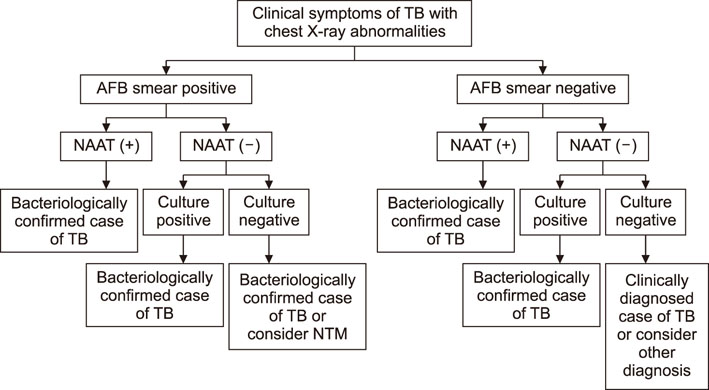
- Tuberculosis (TB) is one of the leading causes of adult death in the Asia-Pacific Region, including Indonesia. As an infectious disease caused by Mycobacterium tuberculosis (MTB), TB remains a major public health issue especially in developing nations due to the lack of adequate diagnostic testing facilities. Diagnosis of TB has entered an era of molecular detection that provides faster and more cost-effective methods to diagnose and confirm drug resistance in TB cases, meanwhile, diagnosis by conventional culture systems requires several weeks. New advances in the molecular detection of TB, including the faster and simpler nucleic acid amplification test (NAAT) and whole-genome sequencing (WGS), have resulted in a shorter time for diagnosis and, therefore, faster TB treatments. In this review, we explored the current findings on molecular diagnosis of TB and drug-resistant TB to see how this advancement could be integrated into public health systems in order to control TB.
MeSH Terms
Figure
Reference
-
1. World Health Organization. Global tuberculosis report 2014. Geneva: World Health Organization;2014.2. Lisdawati V, Puspandari N, Rif'ati L, Soekarno T, M M, K S, et al. Molecular epidemiology study of Mycobacterium tuberculosis and its susceptibility to anti-tuberculosis drugs in Indonesia. BMC Infect Dis. 2015; 15:366.
Article3. Engström A. Fighting an old disease with modern tools: characteristics and molecular detection methods of drug-resistant Mycobacterium tuberculosis. Infect Dis (Lond). 2016; 48:1–17.
Article4. Ghodbane R, Raoult D, Drancourt M. Dramatic reduction of culture time of Mycobacterium tuberculosis. Sci Rep. 2014; 4:4236.
Article5. Cho WH, Won EJ, Choi HJ, Kee SJ, Shin JH, Ryang DW, et al. Comparison of AdvanSure TB/NTM PCR and COBAS TaqMan MTB PCR for detection of mycobacterium tuberculosis complex in routine clinical practice. Ann Lab Med. 2015; 35:356–361.
Article6. Huggett JF, McHugh TD, Zumla A. Tuberculosis: amplification- based clinical diagnostic techniques. Int J Biochem Cell Biol. 2003; 35:1407–1412.7. Balasingham SV, Davidsen T, Szpinda I, Frye SA, Tønjum T. Molecular diagnostics in tuberculosis: basis and implications for therapy. Mol Diagn Ther. 2009; 13:137–151.8. Denkinger CM, Kik SV, Cirillo DM, Casenghi M, Shinnick T, Weyer K, et al. Defining the needs for next generation assays for tuberculosis. J Infect Dis. 2015; 211:Suppl 2. S29–S38.
Article9. Drobniewski F, Nikolayevskyy V, Maxeiner H, Balabanova Y, Casali N, Kontsevaya I, et al. Rapid diagnostics of tuberculosis and drug resistance in the industrialized world: clinical and public health benefits and barriers to implementation. BMC Med. 2013; 11:190.
Article10. Qin L, Zheng R, Fan C, Cai J, Liu Z, Wang J, et al. Identification and evaluation of a new nucleic acid amplification test target for specific detection of Mycobacterium tuberculosis. Clin Chem Lab Med. 2010; 48:1501–1505.
Article11. Niemz A, Boyle DS. Nucleic acid testing for tuberculosis at the point-of-care in high-burden countries. Expert Rev Mol Diagn. 2012; 12:687–701.
Article12. Tiwari S, Nataraj G, Kanade S, Mehta P. Diagnosis of pediatric pulmonary tuberculosis with special reference to polymerase chain reaction based nucleic acid amplification test. Int J Mycobacteriol. 2015; 4:48–53.
Article13. Sia IG, Wieland ML. Current concepts in the management of tuberculosis. Mayo Clin Proc. 2011; 86:348–361.
Article14. Automated real-time nucleic acid amplification technology for rapid and simultaneous detection of tuberculosis and rifampicin resistance: xpert MTB/RIF assay for the diagnosis of pulmonary and extrapulmonary TB in adults and children. WHO Global TB Programme. Geneva: World Health Organization;2013.15. Coll P, Garrigó C, Moreno C, Martì N. Routine use of Gen-Probe Amplified Mycobacterium Tuberculosis Direct (MTD) test for detection of Mycobacterium tuberculosis with smear-positive and smear-negative specimens. Int J Tuberc Lung Dis. 2003; 7:886–891.16. Kunduracğlu A, Karasu I, Biçmen C, Ozsöz A, Erbaycu AE. Comparison of the performances of MTD Gene-Probe® test, BACTEC 960™ system and Löwenstein-Jensen culture methods in the diagnosis of smear-negative tuberculosis cases. Mikrobiyol Bul. 2013; 47:417–431.
Article17. Papaventsis D, Ioannidis P, Karabela S, Nikolaou S, Syridou G, Marinou I, et al. Impact of the Gen-Probe Amplified MTD® Test on tuberculosis diagnosis in children. Int J Tuberc Lung Dis. 2012; 16:384–390.
Article18. Carpentier E, Drouillard B, Dailloux M, Moinard D, Vallee E, Dutilh B, et al. Diagnosis of tuberculosis by Amplicor Mycobacterium tuberculosis test: a multicenter study. J Clin Microbiol. 1995; 33:3106–3110.
Article19. Bergmann JS, Woods GL. Clinical evaluation of the Roche AMPLICOR PCR Mycobacterium tuberculosis test for detection of M. tuberculosis in respiratory specimens. J Clin Microbiol. 1996; 34:1083–1085.
Article20. Devallois A, Legrand E, Rastogi N. Evaluation of Amplicor MTB test as adjunct to smears and culture for direct detection of Mycobacterium tuberculosis in the French Caribbean. J Clin Microbiol. 1996; 34:1065–1068.
Article21. Woods GL. Molecular methods in the detection and identification of mycobacterial infections. Arch Pathol Lab Med. 1999; 123:1002–1006.
Article22. Iwamoto T, Sonobe T, Hayashi K. Loop-mediated isothermal amplification for direct detection of Mycobacterium tuberculosis complex, M. avium, and M. intracellulare in sputum samples. J Clin Microbiol. 2003; 41:2616–2622.
Article23. Neonakis IK, Spandidos DA, Petinaki E. Use of loop-mediated isothermal amplification of DNA for the rapid detection of Mycobacterium tuberculosis in clinical specimens. Eur J Clin Microbiol Infect Dis. 2011; 30:937–942.
Article24. Mitarai S, Okumura M, Toyota E, Yoshiyama T, Aono A, Sejimo A, et al. Evaluation of a simple loop-mediated isothermal amplification test kit for the diagnosis of tuberculosis. Int J Tuberc Lung Dis. 2011; 15:1211–1217.
Article25. Fang R, Li X, Hu L, You Q, Li J, Wu J, et al. Cross-priming amplification for rapid detection of Mycobacterium tuberculosis in sputum specimens. J Clin Microbiol. 2009; 47:845–847.
Article26. Ou X, Song Y, Zhao B, Li Q, Xia H, Zhou Y, et al. A multicenter study of cross-priming amplification for tuberculosis diagnosis at peripheral level in China. Tuberculosis (Edinb). 2014; 94:428–433.
Article27. Castan P, de Pablo A, Fern . dez-Romero N, Rubio JM, Cobb BD, Mingorance J, et al. Point-of-care system for detection of Mycobacterium tuberculosis and rifampin resistance in sputum samples. J Clin Microbiol. 2014; 52:502–507.
Article28. Cheng VC, Yew WW, Yuen KY. Molecular diagnostics in tuberculosis. Eur J Clin Microbiol Infect Dis. 2005; 24:711–720.
Article29. Laraque F, Griggs A, Slopen M, Munsiff SS. Performance of nucleic acid amplification tests for diagnosis of tuberculosis in a large urban setting. Clin Infect Dis. 2009; 49:46–54.
Article30. Centers for Disease Control and Prevention (CDC). Updated guidelines for the use of nucleic acid amplification tests in the diagnosis of tuberculosis. MMWR Morb Mortal Wkly Rep. 2009; 58:7–10.31. Centers for Disease Control and Prevention (CDC). Update: Nucleic acid amplification tests for tuberculosis. MMWR Morb Mortal Wkly Rep. 2000; 49:593–594.32. Dylewski J. Nucleic Acid amplification testing for the diagnosis of tuberculosis: not for all. Clin Infect Dis. 2009; 49:1456–1457.
Article33. Ling DI, Flores LL, Riley LW, Pai M. Commercial nucleic-acid amplification tests for diagnosis of pulmonary tuberculosis in respiratory specimens: meta-analysis and meta-regression. PLoS One. 2008; 3:e1536.
Article34. Centers for Disease Control and Prevention (CDC). Availability of an assay for detecting Mycobacterium tuberculosis, including rifampin-resistant strains, and considerations for its use - United States, 2013. MMWR Morb Mortal Wkly Rep. 2013; 62:821–827.35. Friedrich SO, Rachow A, Saathoff E, Singh K, Mangu CD, Dawson R, et al. Assessment of the sensitivity and specificity of Xpert MTB/RIF assay as an early sputum biomarker of response to tuberculosis treatment. Lancet Respir Med. 2013; 1:462–470.
Article36. World Health Organization. Automated real-time nucleic acid amplification technology for rapid and simultaneous detection of tuberculosis and rifampicin resistance: Xpert MTB/RIF system. Geneva: World Health Organization;2011.37. WHO Global TB Programme. Xpert MTB/RIF implementation manual: technical and operational 'how-to': practical considerations. Geneva: World Health Organization;2014.38. Zeka AN, Tasbakan S, Cavusoglu C. Evaluation of the Gene- Xpert MTB/RIF assay for rapid diagnosis of tuberculosis and detection of rifampin resistance in pulmonary and extrapulmonary specimens. J Clin Microbiol. 2011; 49:4138–4141.
Article39. Boehme CC, Nabeta P, Hillemann D, Nicol MP, Shenai S, Krapp F, et al. Rapid molecular detection of tuberculosis and rifampin resistance. N Engl J Med. 2010; 363:1005–1015.
Article40. World Health Organization. Systematic screening for active tuberculosis: principles and recommendations. Geneva: World Health Organization;2013.41. Steingart KR, Schiller I, Horne DJ, Pai M, Boehme CC, Dendukuri N. Xpert® MTB/RIF assay for pulmonary tuberculosis and rifampicin resistance in adults. Cochrane Database Syst Rev. 2014; (1):CD009593.
Article42. Boehme CC, Nicol MP, Nabeta P, Michael JS, Gotuzzo E, Tahirli R, et al. Feasibility, diagnostic accuracy, and effectiveness of decentralised use of the Xpert MTB/RIF test for diagnosis of tuberculosis and multidrug resistance: a multicentre implementation study. Lancet. 2011; 377:1495–1505.
Article43. Steingart KR, Sohn H, Schiller I, Kloda LA, Boehme CC, Pai M, et al. Xpert® MTB/RIF assay for pulmonary tuberculosis and resistance in adults. Cochrane Database Syst Rev. 2013; (1):CD009593.44. Pantoja A, Kik SV, Denkinger CM. Costs of novel tuberculosis diagnostics--will countries be able to afford it? J Infect Dis. 2015; 211:Suppl 2. S67–S77.
Article45. Bodmer T, Ströhle A. Diagnosing pulmonary tuberculosis with the Xpert MTB/RIF test. J Vis Exp. 2012; (62):e3547.
Article46. Churchyard GJ, Stevens WS, Mametja LD, McCarthy KM, Chihota V, Nicol MP, et al. Xpert MTB/RIF versus sputum microscopy as the initial diagnostic test for tuberculosis: a cluster- randomised trial embedded in South African roll-out of Xpert MTB/RIF. Lancet Glob Health. 2015; 3:e450–e457.47. Kwong JC, McCallum N, Sintchenko V, Howden BP. Whole genome sequencing in clinical and public health microbiology. Pathology. 2015; 47:199–210.
Article48. Walker TM, Ip CL, Harrell RH, Evans JT, Kapatai G, Dedicoat MJ, et al. Whole-genome sequencing to delineate Mycobacterium tuberculosis outbreaks: a retrospective observational study. Lancet Infect Dis. 2013; 13:137–146.
Article49. Köser CU, Ellington MJ, Peacock SJ. Whole-genome sequencing to control antimicrobial resistance. Trends Genet. 2014; 30:401–407.
Article50. Metzker ML. Emerging technologies in DNA sequencing. Genome Res. 2005; 15:1767–1776.
Article51. Strausberg RL, Levy S, Rogers YH. Emerging DNA sequencing technologies for human genomic medicine. Drug Discov Today. 2008; 13:569–577.
Article52. Rizzo JM, Buck MJ. Key principles and clinical applications of "next-generation" DNA sequencing. Cancer Prev Res (Phila). 2012; 5:887–900.
Article53. Metzker ML. Sequencing technologies - the next generation. Nat Rev Genet. 2010; 11:31–46.
Article54. Witney AA, Cosgrove CA, Arnold A, Hinds J, Stoker NG, Butcher PD. Clinical use of whole genome sequencing for Mycobacterium tuberculosis. BMC Med. 2016; 14:46.
Article55. Köser CU, Bryant JM, Becq J, Török ME, Ellington MJ, Marti-Renom MA, et al. Whole-genome sequencing for rapid susceptibility testing of M. tuberculosis. N Engl J Med. 2013; 369:290–292.
Article56. Bjorn-Mortensen K, Zallet J, Lillebaek T, Andersen AB, Niemann S, Rasmussen EM, et al. Direct DNA Extraction from Mycobacterium tuberculosis Frozen Stocks as a Reculture-Independent Approach to Whole-Genome Sequencing. J Clin Microbiol. 2015; 53:2716–2719.
Article57. Votintseva AA, Pankhurst LJ, Anson LW, Morgan MR, Gascoyne-Binzi D, Walker TM, et al. Mycobacterial DNA extraction for whole-genome sequencing from early positive liquid (MGIT) cultures. J Clin Microbiol. 2015; 53:1137–1143.
Article58. Brown AC, Bryant JM, Einer-Jensen K, Holdstock J, Houniet DT, Chan JZ, et al. Rapid whole-genome sequencing of mycobacterium tuberculosis isolates directly from clinical samples. J Clin Microbiol. 2015; 53:2230–2237.
Article59. Witney AA, Gould KA, Arnold A, Coleman D, Delgado R, Dhillon J, et al. Clinical application of whole-genome sequencing to inform treatment for multidrug-resistant tuberculosis cases. J Clin Microbiol. 2015; 53:1473–1483.
Article60. McAlister AJ, Driscoll J, Metchock B. DNA sequencing for confirmation of rifampin resistance detected by Cepheid Xpert MTB/RIF assay. J Clin Microbiol. 2015; 53:1752–1753.
Article61. Takiff HE, Feo O. Clinical value of whole-genome sequencing of Mycobacterium tuberculosis. Lancet Infect Dis. 2015; 15:1077–1090.
Article62. Hasan MR, Tan R, Al-Rawahi GN, Thomas E, Tilley P. Short-term stability of pathogen-specific nucleic acid targets in clinical samples. J Clin Microbiol. 2012; 50:4147–4150.
Article63. Omar SV, Peters RP, Ismail NA, Dreyer AW, Said HM, Gwala T, et al. Laboratory evaluation of a specimen transport medium for downstream molecular processing of sputum samples to detect Mycobacterium tuberculosis. J Microbiol Methods. 2015; 117:57–63.
Article64. Daum LT, Peters RP, Fourie PB, Jonkman K, Worthy SA, Rodriguez JD, et al. Molecular detection of Mycobacterium tuberculosis from sputum transported in PrimeStore(®) from rural settings. Int J Tuberc Lung Dis. 2015; 19:552–557.
Article65. Das D, Dwibedi B, Kar SK. Transportation of sputum samples in cetylpyridinium chloride for drug resistance studies from remote areas of Odisha, India. J Infect Dev Ctries. 2014; 8:1059–1062.
Article66. Banada PP, Sivasubramani SK, Blakemore R, Boehme C, Perkins MD, Fennelly K, et al. Containment of bioaerosol infection risk by the Xpert MTB/RIF assay and its applicability to point-of-care settings. J Clin Microbiol. 2010; 48:3551–3557.
Article67. Alnimr AM, Hassan MI. Potential of two nucleic acid amplification assays for quantifying mycobacterial load in respiratory and non-respiratory specimens: a prospective study. Diagn Microbiol Infect Dis. 2014; 78:237–241.
Article68. Wang JY, Lee LN, Lai HC, Hsu HL, Jan IS, Yu CJ, et al. Performance assessment of the Capilia TB assay and the BD ProbeTec ET system for rapid culture confirmation of Mycobacterium tuberculosis. Diagn Microbiol Infect Dis. 2007; 59:395–399.
Article69. Kim YJ, Park MY, Kim SY, Cho SA, Hwang SH, Kim HH, et al. Evaluation of the performances of AdvanSure TB/NTM real time PCR kit for detection of mycobacteria in respiratory specimens. Korean J Lab Med. 2008; 28:34–38.
Article70. Lee H, Park KG, Lee G, Park J, Park YG, Park YJ. Assessment of the quantitative ability of AdvanSure TB/NTM real-time PCR in respiratory specimens by comparison with phenotypic methods. Ann Lab Med. 2014; 34:51–55.
Article71. Choe W, Kim E, Park SY, Chae JD. Performance evaluation of anyplex plus MTB/NTM and AdvanSure TB/NTM for the detection of Mycobacterium tuberculosis and nontuberculous mycobacteria. Ann Clin Microbiol. 2015; 18:44–51.
Article72. Steingart KR, Flores LL, Dendukuri N, Schiller I, Laal S, Ramsay A, et al. Commercial serological tests for the diagnosis of active pulmonary and extrapulmonary tuberculosis: an updated systematic review and meta-analysis. PLoS Med. 2011; 8:e1001062.
Article73. Senoputra MA, Shiratori B, Hasibuan FM, Koesoemadinata RC, Apriani L, Ashino Y, et al. Diagnostic value of antibody responses to multiple antigens from Mycobacterium tuberculosis in active and latent tuberculosis. Diagn Microbiol Infect Dis. 2015; 83:278–285.
Article74. Fujita Y, Doi T, Maekura R, Ito M, Yano I. Differences in serological responses to specific glycopeptidolipid-core and common lipid antigens in patients with pulmonary disease due to Mycobacterium tuberculosis and Mycobacterium avium complex. J Med Microbiol. 2006; 55:189–199.
Article75. Steingart KR, Ramsay A, Dowdy DW, Pai M. Serological tests for the diagnosis of active tuberculosis: relevance for India. Indian J Med Res. 2012; 135:695–702.76. World Health Organization. Tuberculosis serodiagnostic tests policy statement 2011. Geneva: World Health Organization;2013.77. Ahmad S, Mokaddas E. Current status and future trends in the diagnosis and treatment of drug-susceptible and multidrug-resistant tuberculosis. J Infect Public Health. 2014; 7:75–91.
Article78. Lee SH, Choi HB, Yu SY, Chang UJ, Kim CK, Kim HJ. Detection of first-line anti-tuberculosis drug resistance mutations by allele- specific primer extension on a microsphere-based platform. Ann Lab Med. 2015; 35:487–493.
Article79. Coll F, McNerney R, Preston MD, Guerra-Assunção JA, Warry A, Hill-Cawthorne G, et al. Rapid determination of anti-tuberculosis drug resistance from whole-genome sequences. Genome Med. 2015; 7:51.
Article80. Outhred AC, Jelfs P, Suliman B, Hill-Cawthorne GA, Crawford AB, Marais BJ, et al. Added value of whole-genome sequencing for management of highly drug-resistant TB. J Antimicrob Chemother. 2015; 70:1198–1202.
Article81. Xu HB, Jiang RH, Sha W, Li L, Xiao HP. PCR-single-strand conformational polymorphism method for rapid detection of rifampin- resistant Mycobacterium tuberculosis: systematic review and meta-analysis. J Clin Microbiol. 2010; 48:3635–3640.
Article82. Catanzaro A, Rodwell TC, Catanzaro DG, Garfein RS, Jackson RL, Seifert M, et al. Performance comparison of three rapid tests for the diagnosis of drug-resistant tuberculosis. PLoS One. 2015; 10:e0136861.
Article83. Molina-Moya B, Lacoma A, Prat C, Diaz J, Dudnyk A, Haba L, et al. AID TB resistance line probe assay for rapid detection of resistant Mycobacterium tuberculosis in clinical samples. J Infect. 2015; 70:400–408.
Article84. Li Q, Dong HY, Pang Y, Xia H, Ou XC, Zhang ZY, et al. Multicenter evaluation of the molecular line probe assay for multidrug resistant mycobacterium tuberculosis detection in China. Biomed Environ Sci. 2015; 28:464–467.85. Viveiros M, Leandro C, Rodrigues L, Almeida J, Bettencourt R, Couto I, et al. Direct application of the INNO-LiPA Rif.TB line-probe assay for rapid identification of Mycobacterium tuberculosis complex strains and detection of rifampin resistance in 360 smear-positive respiratory specimens from an area of high incidence of multidrug-resistant tuberculosis. J Clin Microbiol. 2005; 43:4880–4884.
Article86. Yadav RN, Singh BK, Sharma SK, Sharma R, Soneja M, Sreenivas V, et al. Comparative evaluation of GenoType MTBDRplus line probe assay with solid culture method in early diagnosis of multidrug resistant tuberculosis (MDR-TB) at a tertiary care centre in India. PLoS One. 2013; 8:e72036.
Article87. Raizada N, Sachdeva KS, Chauhan DS, Malhotra B, Reddy K, Dave PV, et al. A multi-site validation in India of the line probe assay for the rapid diagnosis of multi-drug resistant tuberculosis directly from sputum specimens. PLoS One. 2014; 9:e88626.
Article88. Kiet VS, Lan NT, An DD, Dung NH, Hoa DV, van Vinh, et al. Evaluation of the MTBDRsl test for detection of second- line-drug resistance in Mycobacterium tuberculosis. J Clin Microbiol. 2010; 48:2934–2939.
Article89. Molecular line probe assays for rapid screening of patients at risk of multi-drug resistant tuberculosis. World Health Organization Policy Statement. Geneva, Switzerland: World Health Organization;2008.90. Ritter C, Lucke K, Sirgel FA, Warren RW, van Helden PD, Böttger EC, et al. Evaluation of the AID TB resistance line probe assay for rapid detection of genetic alterations associated with drug resistance in Mycobacterium tuberculosis strains. J Clin Microbiol. 2014; 52:940–946.
Article91. Rufai SB, Kumar P, Singh A, Prajapati S, Balooni V, Singh S. Comparison of Xpert MTB/RIF with line probe assay for detection of rifampin-monoresistant Mycobacterium tuberculosis. J Clin Microbiol. 2014; 52:1846–1852.
Article92. Yin X, Zheng L, Liu Q, Lin L, Hu X, Hu Y, et al. High-resolution melting curve analysis for rapid detection of rifampin resistance in Mycobacterium tuberculosis: a meta-analysis. J Clin Microbiol. 2013; 51:3294–3299.
Article93. Chakravorty S, Kothari H, Aladegbami B, Cho EJ, Lee JS, Roh SS, et al. Rapid, high-throughput detection of rifampin resistance and heteroresistance in Mycobacterium tuberculosis by use of sloppy molecular beacon melting temperature coding. J Clin Microbiol. 2012; 50:2194–2202.
Article94. Martin A, Panaiotov S, Portaels F, Hoffner S, Palomino JC, Angeby K. The nitrate reductase assay for the rapid detection of isoniazid and rifampicin resistance in Mycobacterium tuberculosis: a systematic review and meta-analysis. J Antimicrob Chemother. 2008; 62:56–64.
Article95. Coban AY, Deveci A, Sunter AT, Martin A. Nitrate reductase assay for rapid detection of isoniazid, rifampin, ethambutol, and streptomycin resistance in Mycobacterium tuberculosis: a systematic review and meta-analysis. J Clin Microbiol. 2014; 52:15–19.
Article96. Gonzalez L, Sanchez R, Murcia MI. The usefulness of the nitrate reductase assay for detecting drug-resistant Mycobacterium tuberculosis. Biomedica. 2014; 34:Suppl 1. 232–238.97. Martin A, Portaels F, Palomino JC. Colorimetric redox-indicator methods for the rapid detection of multidrug resistance in Mycobacterium tuberculosis: a systematic review and meta-analysis. J Antimicrob Chemother. 2007; 59:175–183.
Article98. Coban AY, Akbal AU, Uzun M, Durupinar B. Evaluation of four colourimetric susceptibility tests for the rapid detection of multidrug- resistant Mycobacterium tuberculosis isolates. Mem Inst Oswaldo Cruz. 2015; 110:649–654.
Article99. Cheng X, Zhang J, Yang L, Xu X, Liu J, Yu W, et al. A new Multi-PCR-SSCP assay for simultaneous detection of isoniazid and rifampin resistance in Mycobacterium tuberculosis. J Microbiol Methods. 2007; 70:301–305.
Article100. Cabibbe AM, Miotto P, Moure R, Alcaide F, Feuerriegel S, Pozzi G, et al. Lab-on-chip-based platform for fast molecular diagnosis of multidrug-resistant tuberculosis. J Clin Microbiol. 2015; 53:3876–3880.
Article101. Pérez-Osorio AC, Boyle DS, Ingham ZK, Ostash A, Gautom RK, Colombel C, et al. Rapid identification of mycobacteria and drug-resistant Mycobacterium tuberculosis by use of a single multiplex PCR and DNA sequencing. J Clin Microbiol. 2012; 50:326–336.
Article102. Chia BS, Lanzas F, Rifat D, Herrera A, Kim EY, Sailer C, et al. Use of multiplex allele-specific polymerase chain reaction (MAS-PCR) to detect multidrug-resistant tuberculosis in Panama. PLoS One. 2012; 7:e40456.
Article103. Choi JH, Lee KW, Kang HR, Hwang YI, Jang S, Kim DG, et al. Clinical efficacy of direct DNA sequencing analysis on sputum specimens for early detection of drug-resistant Mycobacterium tuberculosis in a clinical setting. Chest. 2010; 137:393–400.
Article104. Engström A, Juréen P. Detection of Drug-Resistant Mycobacterium tuberculosis. Methods Mol Biol. 2015; 1315:349–362.
Article105. Lacoma A, Molina-Moya B, Prat C, Pimkina E, Diaz J, Dudnyk A, et al. Pyrosequencing for rapid detection of Mycobacterium tuberculosis second-line drugs and ethambutol resistance. Diagn Microbiol Infect Dis. 2015; 83:263–269.
Article106. Lin SY, Rodwell TC, Victor TC, Rider EC, Pham L, Catanzaro A, et al. Pyrosequencing for rapid detection of extensively drug-resistant Mycobacterium tuberculosis in clinical isolates and clinical specimens. J Clin Microbiol. 2014; 52:475–482.
Article107. Theron G, Peter J, Richardson M, Barnard M, Donegan S, Warren R, et al. The diagnostic accuracy of the GenoType(®) MTBDRsl assay for the detection of resistance to second-line anti- tuberculosis drugs. Cochrane Database Syst Rev. 2014; (10):CD010705.
Article108. Barnard M, Warren R, Gey Van, van Helden P, Bosman M, Streicher E, et al. GenoType MTBDRsl line probe assay shortens time to diagnosis of extensively drug-resistant tuberculosis in a high-throughput diagnostic laboratory. Am J Respir Crit Care Med. 2012; 186:1298–1305.
Article109. Lacoma A, Garcìa-Sierra N, Prat C, Maldonado J, Ruiz-Manzano J, Haba L, et al. GenoType MTBDRsl for molecular detection of second-line-drug and ethambutol resistance in Mycobacterium tuberculosis strains and clinical samples. J Clin Microbiol. 2012; 50:30–36.
Article110. Brossier F, Veziris N, Aubry A, Jarlier V, Sougakoff W. Detection by GenoType MTBDRsl test of complex mechanisms of resistance to second-line drugs and ethambutol in multidrug-resistant Mycobacterium tuberculosis complex isolates. J Clin Microbiol. 2010; 48:1683–1689.
Article111. Feng Y, Liu S, Wang Q, Wang L, Tang S, Wang J, et al. Rapid diagnosis of drug resistance to fluoroquinolones, amikacin, capreomycin, kanamycin and ethambutol using genotype MTBDRsl assay: a meta-analysis. PLoS One. 2013; 8:e55292.
Article112. Mahendradhata Y, Probandari A, Widjanarko B, Riono P, Mustikawati D, Tiemersma EW, et al. Embedding operational research into national disease control programme: lessons from 10 years of experience in Indonesia. Glob Health Action. 2014; 7:25412.
Article113. Kaul KL. Molecular detection of Mycobacterium tuberculosis: impact on patient care. Clin Chem. 2001; 47:1553–1558.
Article114. Dowdy DW, Houben R, Cohen T, Pai M, Cobelens F, Vassall A, et al. Impact and cost-effectiveness of current and future tuberculosis diagnostics: the contribution of modelling. Int J Tuberc Lung Dis. 2014; 18:1012–1018.
Article115. Lawn SD. Advances in diagnostic assays for tuberculosis. Cold Spring Harb Perspect Med. 2015; 5:a017806.
Article