Chonnam Med J.
2019 Sep;55(3):144-149. 10.4068/cmj.2019.55.3.144.
Effects of Fimasartan/Amlodipine Fixed-Dose Combination on Left Ventricular Systolic Function and Infarct Size in Rat Myocardial Infarction Model
- Affiliations
-
- 1Division of Cardiology, Cardiovascular Convergence Research Center Nominated by Korea Ministry of Health and Welfare, Chonnam National University Hospital, Gwangju, Korea. hyj200@hanmail.net
- KMID: 2458566
- DOI: http://doi.org/10.4068/cmj.2019.55.3.144
Abstract
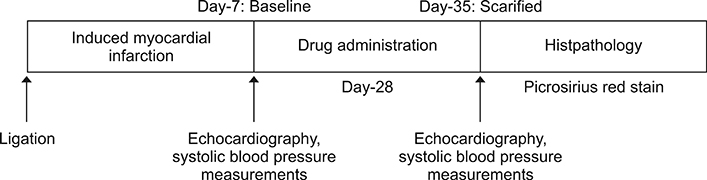
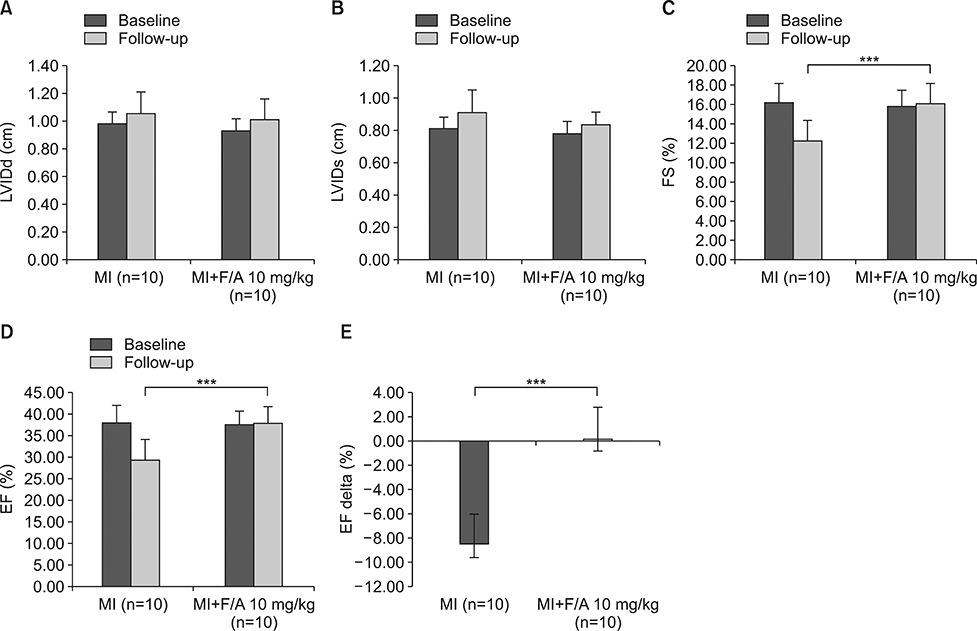
- The aim of this study was to evaluate the effects of fimasartan/amlodipine fixed-dosed combination (F/A) on left ventricle (LV) systolic function and infarct size in the rat myocardial infarction (MI) model. We induced MI in 20 rats by ligation of the left anterior descending coronary artery and they were divided into two groups [MI group (n=10) vs. MI+F/A 10 mg/kg group (n=10)]. F/A was administered for 28 days between day-7 and day-35 in the MI+F/A group and echocardiography was performed at day-7 and at day-35 after the induction of MI. Picrosirius red staining was performed to confirm the fibrotic tissue and infarct size was measured using image analysis program for Image J. At the 35-day follow-up, the LV ejection fraction (EF) was significantly higher (38.10±3.92% vs. 29.86±4.56%, p<0.001) and delta (day-35 minus day-7) EF was significantly higher (0.14±2.66% vs. −8.53±2.66%. p<0.001) in the MI+F/A group than the MI group. Systolic blood pressure was significantly lower in the MI+F/A group than the MI group (103.23±13.35 mmHg vs. 123.43±14.82 mmHg, p<0.01). The MI+F/A group had a smaller infarct size (26.84±5.31% vs. 36.79±3.10%, p<0.01) than the MI group at the 35-day follow-up. Oral administration of F/A 10 mg/kg could improve LV systolic function and reduce infarct size in a rat MI model.
Keyword
MeSH Terms
Figure
Reference
-
1. Katz MG, Fargnoli AS, Gubara SM, Chepurko E, Bridges CR, Hajjar RJ. Surgical and physiological challenges in the development of left and right heart failure in rat models. Heart Fail Rev. 2019; 24:759–777.
Article2. Houser SR, Margulies KB, Murphy AM, Spinale FG, Francis GS, Prabhu SD, et al. American Heart Association Council on Basic Cardiovascular Sciences. Council on Clinical Cardiology. Council on Functional Genomics and Translational Biology. Animal models of heart failure: a scientific statement from the American Heart Association. Circ Res. 2012; 111:131–150.3. Emde B, Heinen A, Gödecke A, Bottermann K. Wheat germ agglutinin staining as a suitable method for detection and quantification of fibrosis in cardiac tissue after myocardial infarction. Eur J Histochem. 2014; 58:2448.
Article4. Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, et al. Authors/Task Force Members. Document Reviewers. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2016; 18:891–975.
Article5. Soumerai SB, McLaughlin TJ, Spiegelman D, Hertzmark E, Thibault G, Goldman L. Adverse outcomes of underuse of beta-blockers in elderly survivors of acute myocardial infarction. JAMA. 1997; 277:115–121.
Article6. Køber L, Torp-Pedersen C, Carlsen JE, Bagger H, Eliasen P, Lyngborg K, et al. A clinical trial of the angiotensin-converting-enzyme inhibitor trandolapril in patients with left ventricular dysfunction after myocardial infarction. Trandolapril Cardiac Evaluation (TRACE) Study Group. N Engl J Med. 1995; 333:1670–1676.
Article7. Pitt B, Remme W, Zannad F, Neaton J, Martinez F, Roniker B, et al. Eplerenone Post-Acute Myocardial Infarction Heart Failure Efficacy and Survival Study Investigators. Eplerenone, a selective aldosterone blocker, in patients with left ventricular dysfunction after myocardial infarction. N Engl J Med. 2003; 348:1309–1321.
Article8. Han J, Park SJ, Thu VT, Lee SR, Long le T, Kim HK, et al. Effects of the novel angiotensin II receptor type I antagonist, fimasartan on myocardial ischemia/reperfusion injury. Int J Cardiol. 2013; 168:2851–2859.
Article9. Owen AJ, Reid CM. Cardio classics revisited: focus on the role of amlodipine. Integr Blood Press Control. 2012; 5:1–7.
Article10. Fliss H, Gattinger D. Apoptosis in ischemic and reperfused rat myocardium. Circ Res. 1996; 79:949–956.
Article11. Sahn DJ, DeMaria A, Kisslo J, Weyman A. Recommendations regarding quantitation in M-mode echocardiography: results of a survey of echocardiographic measurements. Circulation. 1978; 58:1072–1083.
Article12. Gardin JM, Siri FM, Kitsis RN, Edwards JG, Leinwand LA. Echocardiographic assessment of left ventricular mass and systolic function in mice. Circ Res. 1995; 76:907–914.
Article13. Zhang Y, Köhler K, Xu J, Lu D, Braun T, Schlitt A, et al. Inhibition of p53 after acute myocardial infarction: reduction of apoptosis is counteracted by disturbed scar formation and cardiac rupture. J Mol Cell Cardiol. 2011; 50:471–478.
Article14. Buñag RD. Validation in awake rats of a tail-cuff method for measuring systolic pressure. J Appl Physiol. 1973; 34:279–282.
Article15. Sutton MG, Sharpe N. Left ventricular remodeling after myocardial infarction: pathophysiology and therapy. Circulation. 2000; 101:2981–2988.
Article16. Fishbein MC, Maclean D, Maroko PR. The histopathologic evolution of myocardial infarction. Chest. 1978; 73:843–849.
Article17. Pfeffer MA, Braunwald E. Ventricular remodeling after myocardial infarction. Experimental observations and clinical implications. Circulation. 1990; 81:1161–1172.
Article18. de Gasparo M, Catt KJ, Inagami T, Wright JW, Unger T. International union of pharmacology. XXIII. The angiotensin II receptors. Pharmacol Rev. 2000; 52:415–472.19. Rompe F, Artuc M, Hallberg A, Alterman M, Ströder K, Thöne-Reineke C, et al. Direct angiotensin II type 2 receptor stimulation acts anti-inflammatory through epoxyeicosatrienoic acid and inhibition of nuclear factor kappaB. Hypertension. 2010; 55:924–931.
Article20. Steckelings UM, Paulis L, Namsolleck P, Unger T. AT2 receptor agonists: hypertension and beyond. Curr Opin Nephrol Hypertens. 2012; 21:142–146.21. Lee SE, Kim YJ, Lee HY, Yang HM, Park CG, Kim JJ, et al. Investigators. Efficacy and tolerability of fimasartan, a new angiotensin receptor blocker, compared with losartan (50/100 mg): a 12-week, phase III, multicenter, prospective, randomized, double-blind, parallel-group, dose escalation clinical trial with an optional 12-week extension phase in adult Korean patients with mild-to-moderate hypertension. Clin Ther. 2012; 34:552–568. 568.e1–568.e9.
Article22. Lee H, Yang HM, Lee HY, Kim JJ, Choi DJ, Seung KB, et al. Efficacy and tolerability of once-daily oral fimasartan 20 to 240 mg/d in Korean Patients with hypertension: findings from Two Phase II, randomized, double-blind, placebo-controlled studies. Clin Ther. 2012; 34:1273–1289.
Article23. Park JB, Sung KC, Kang SM, Cho EJ. Safety and efficacy of fimasartan in patients with arterial hypertension (Safe-KanArb study): an open-label observational study. Am J Cardiovasc Drugs. 2013; 13:47–56.
Article24. Lee H, Kim KS, Chae SC, Jeong MH, Kim DS, Oh BH. Ambulatory blood pressure response to once-daily fimasartan: an 8-week, multicenter, randomized, double-blind, active-comparator, parallel-group study in Korean patients with mild to moderate essential hypertension. Clin Ther. 2013; 35:1337–1349.
Article25. Lim BK, Park JJ, Park SJ, Lee YJ, Kwon JS, Kim EJ, et al. Fimasartan for remodeling after myocardial infarction. J Clin Med. 2019; 8:E366.
Article26. Nissen SE, Tuzcu EM, Libby P, Thompson PD, Ghali M, Garza D, et al. CAMELOT Investigators. Effect of antihypertensive agents on cardiovascular events in patients with coronary disease and normal blood pressure: the CAMELOT study: a randomized controlled trial. JAMA. 2004; 292:2217–2225.
Article27. Mason RP, Kubant R, Heeba G, Jacob RF, Day CA, Medlin YS, et al. Synergistic effect of amlodipine and atorvastatin in reversing LDL-induced endothelial dysfunction. Pharm Res. 2008; 25:1798–1806.
Article28. Khan NA, Chattopadhyay P, Abid M, Pawdey A, Kishore K, Wahi AK. Protective effects of amlodipine on mitochondrial injury in ischemic reperfused rat heart. J Environ Biol. 2012; 33:591–595.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pharmacokinetic comparison between fixed-dose combination of fimasartan/amlodipine 60/10 mg and the corresponding loose combination through partial replicated crossover study in healthy subjects
- Pharmacokinetic comparison between a fixed-dose combination of fimasartan/amlodipine/ hydrochlorothiazide 60/10/25 mg and a corresponding loose combination of fimasartan/amlodipine 60/25 mg and hydrochlorothiazide 25 mg in healthy subjects
- Peiminine inhibits myocardial injury and fibrosis after myocardial infarction in rats by regulating mitogen-activated protein kinase pathway
- Differences in Left and Right Ventricular Function between Different Infarct Sites: An ECG-Gated Blood Pool Study
- The Effects of Carvedilol on Ventricular Remodeling after Myocardial Infarction in Rats