Korean J Radiol.
2016 Oct;17(5):664-673. 10.3348/kjr.2016.17.5.664.
Eye Globe Abnormalities on MR and CT in Adults: An Anatomical Approach
- Affiliations
-
- 1Department of Diagnostic Imaging, National University Health System, Singapore 119074. jim.hallinan@gmail.com
- 2National Healthcare Group Eye Institute, Tan Tock Seng Hospital, Level 1, TTSH Medical Centre, Singapore 308433.
- 3Yong Loo Lin School of Medicine, National University of Singapore, Singapore 117597.
- 4Dr. Goh Eye Neuro-Ophthalmic and Low Vision Specialist, Mount Elizabeth Novena Specialist Centre, Singapore 329563.
- 5Department of Neuroradiology, National Neuroscience Institute, Singapore 308433.
- KMID: 2458058
- DOI: http://doi.org/10.3348/kjr.2016.17.5.664
Abstract
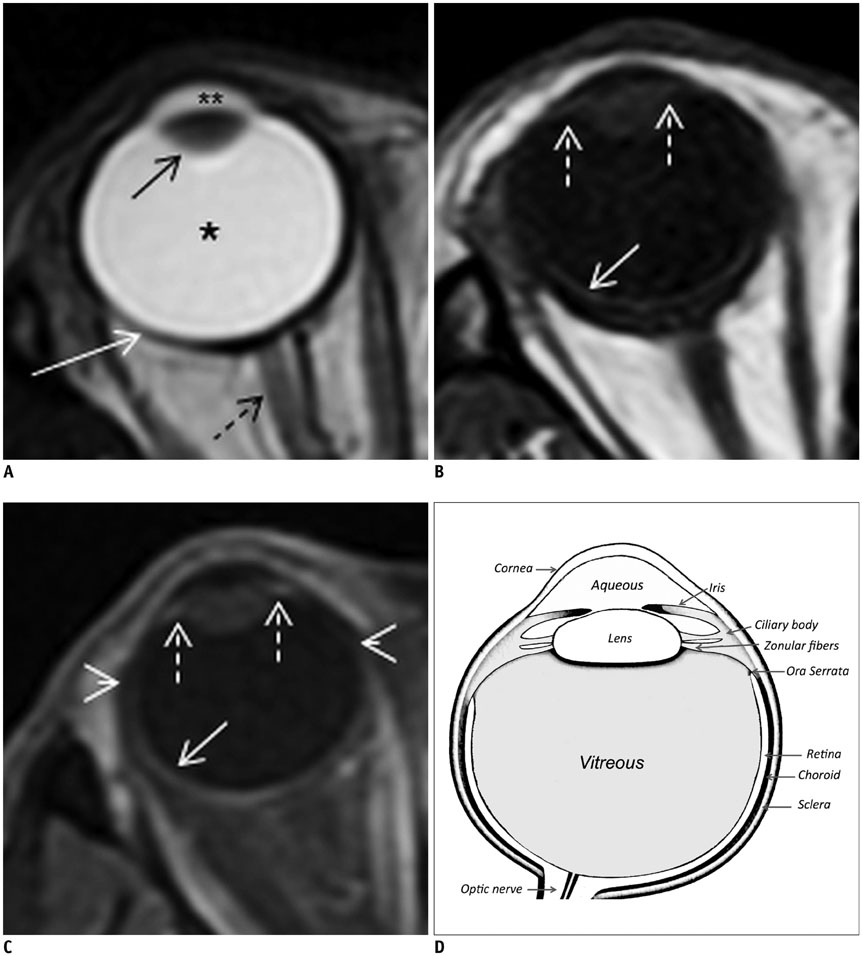
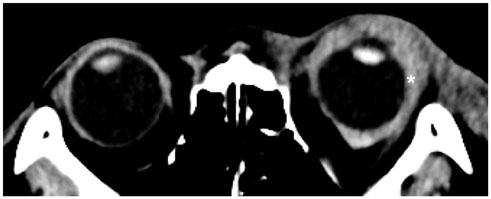
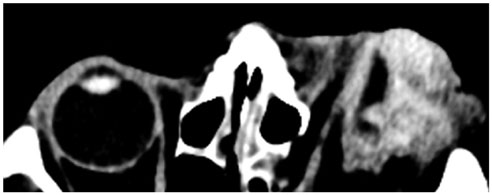
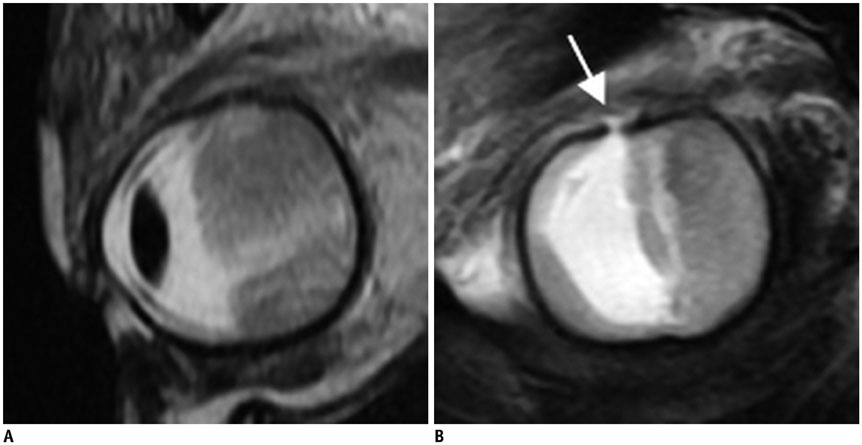
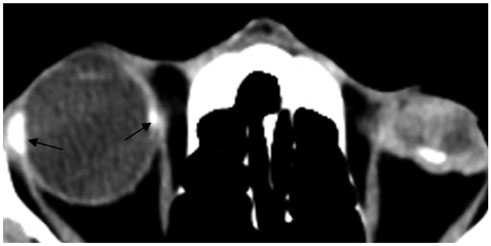
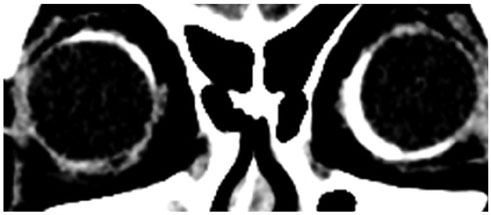
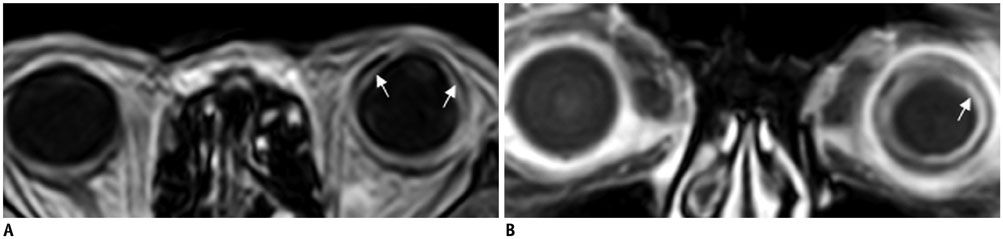
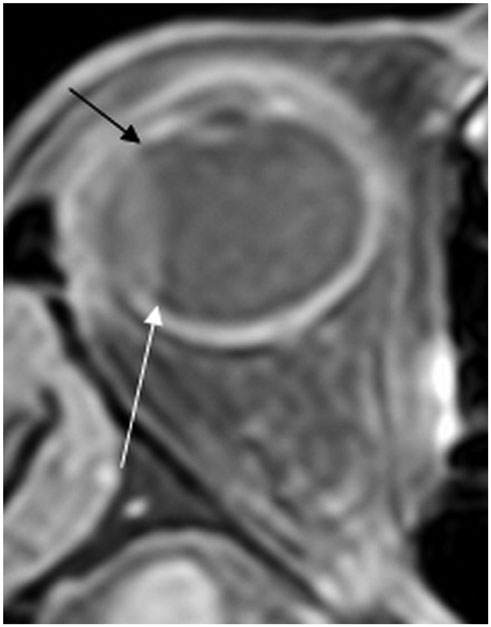
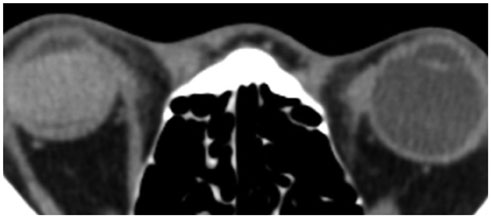
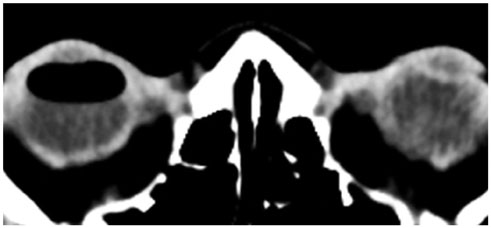
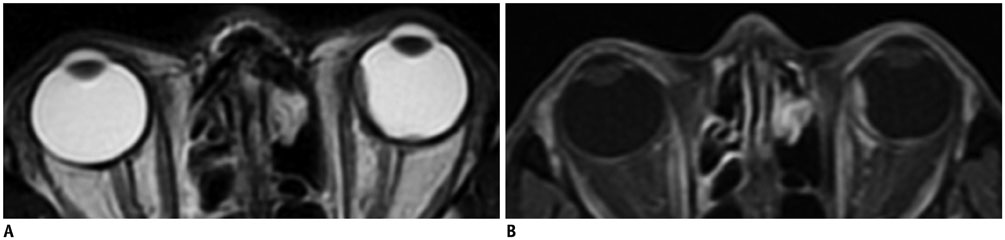
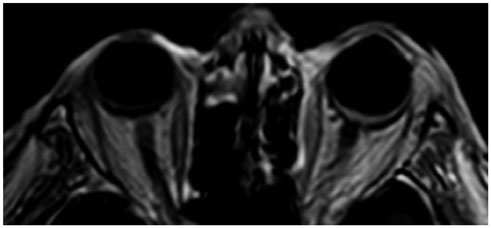
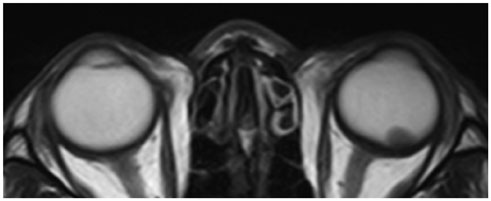
- Eye globe abnormalities can be readily detected on dedicated and non-dedicated CT and MR studies. A primary understanding of the globe anatomy is key to characterising both traumatic and non-traumatic globe abnormalities. The globe consists of three primary layers: the sclera (outer), uvea (middle), and retina (inner layer). The various pathological processes involving these layers are highlighted using case examples with fundoscopic correlation where appropriate. In the emergent setting, trauma can result in hemorrhage, retinal/choroidal detachment and globe rupture. Neoplasms and inflammatory/infective processes predominantly occur in the vascular middle layer. The radiologist has an important role in primary diagnosis contributing to appropriate ophthalmology referral, thereby preventing devastating consequences such as vision loss.
MeSH Terms
Figure
Reference
-
1. Roy AA, Davagnanam I, Evanson J. Abnormalities of the globe. Clin Radiol. 2012; 67:1011–1022.2. Van Tassel P, Mafee MF, Atlas SW, Galetta SL. Chapter 23. Eye, orbit and visual system. In : Atlas SW, editor. Magnetic resonance imaging of the brain and spine. 4th ed. Philadelphia: Lippincott Williams & Wilkins;2009. Volume 2:p. 1258–1363.3. Mafee MF, Karimi A, Shah J, Rapoport M, Ansari SA. Anatomy and pathology of the eye: role of MR imaging and CT. Neuroimaging Clin N Am. 2005; 15:23–47.4. Goh PS, Gi MT, Charlton A, Tan C, Gangadhara Sundar JK, Amrith S. Review of orbital imaging. Eur J Radiol. 2008; 66:387–395.5. Lane JI, Watson RE Jr, Witte RJ, McCannel CA. Retinal detachment: imaging of surgical treatments and complications. Radiographics. 2003; 23:983–994.6. Ahmad SM, Esmaeli B. Metastatic tumors of the orbit and ocular adnexa. Curr Opin Ophthalmol. 2007; 18:405–413.7. Laver NV, McLaughlin ME, Duker JS. Ocular melanoma. Arch Pathol Lab Med. 2010; 134:1778–1784.8. Smoker WR, Gentry LR, Yee NK, Reede DL, Nerad JA. Vascular lesions of the orbit: more than meets the eye. Radiographics. 2008; 28:185–204. quiz 325.9. LeBedis CA, Sakai O. Nontraumatic orbital conditions: diagnosis with CT and MR imaging in the emergent setting. Radiographics. 2008; 28:1741–1753.10. Kubal WS. Imaging of orbital trauma. Radiographics. 2008; 28:1729–1739.11. Rumboldt Z, Moses C, Wieczerzynski U, Saini R. Diffusion-weighted imaging, apparent diffusion coefficients, and fluid-attenuated inversion recovery MR imaging in endophthalmitis. AJNR Am J Neuroradiol. 2005; 26:1869–1872.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Role of Orbital Computed Tomography as a Prognostic Indicator for Open Globe Injury
- A Case of Traumatic Globe Luxation
- Traumatic Displacement of the Globe into the Ethmoid Sinus: Case Report
- Traumatic Displacement of the Globe into the Maxillary Sinus: Case Report
- CT and MR Findings of Persistent Hyperplastic Primary Vitreous(PH PV)