J Korean Assoc Oral Maxillofac Surg.
2019 Aug;45(4):192-198. 10.5125/jkaoms.2019.45.4.192.
Versatile midfacial degloving approach in oral and maxillofacial surgery
- Affiliations
-
- 1Department of Dentistry, ESIC Medical College, Gulbarga, India.
- 2Department of Oral and Maxillofacial Surgery, ESIC Dental College, Gulbarga, India.
- 3Department of Oral and Maxillofacial Surgery, Tamilnadu Government Dental College and Hospital, Chennai, India.
- 4Private Clinic, Bangalore, India.
- 5Department of Dental Surgery, Trinelveli Medical College and Hospital, Trinelveli, India. omfs007@yahoo.in
- 6Department of Periodontology, Navodaya Dental College, Raichur, India.
- KMID: 2456037
- DOI: http://doi.org/10.5125/jkaoms.2019.45.4.192
Abstract
OBJECTIVES
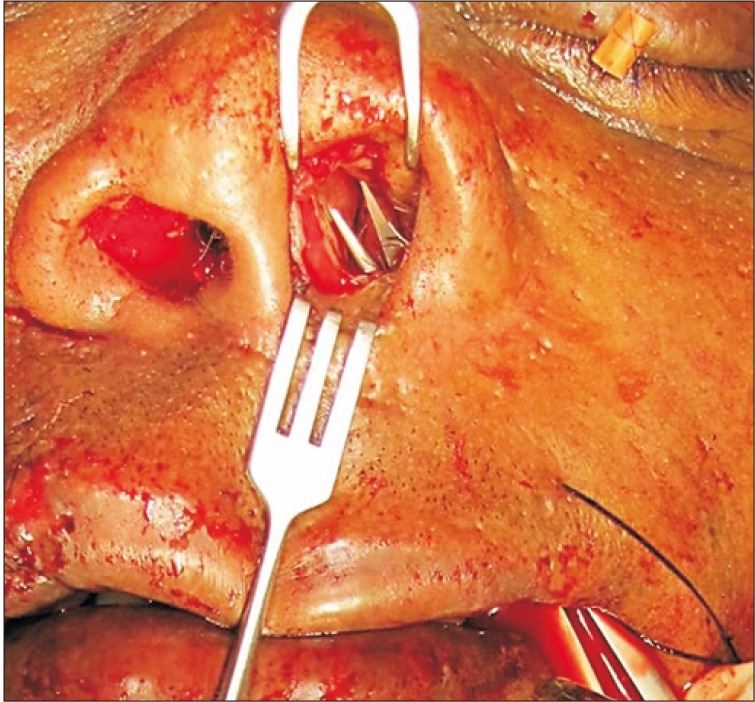
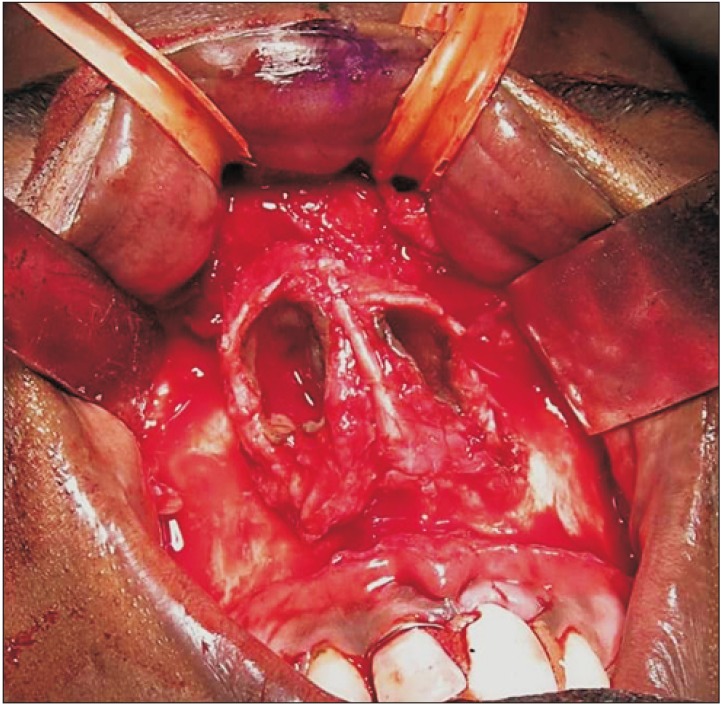
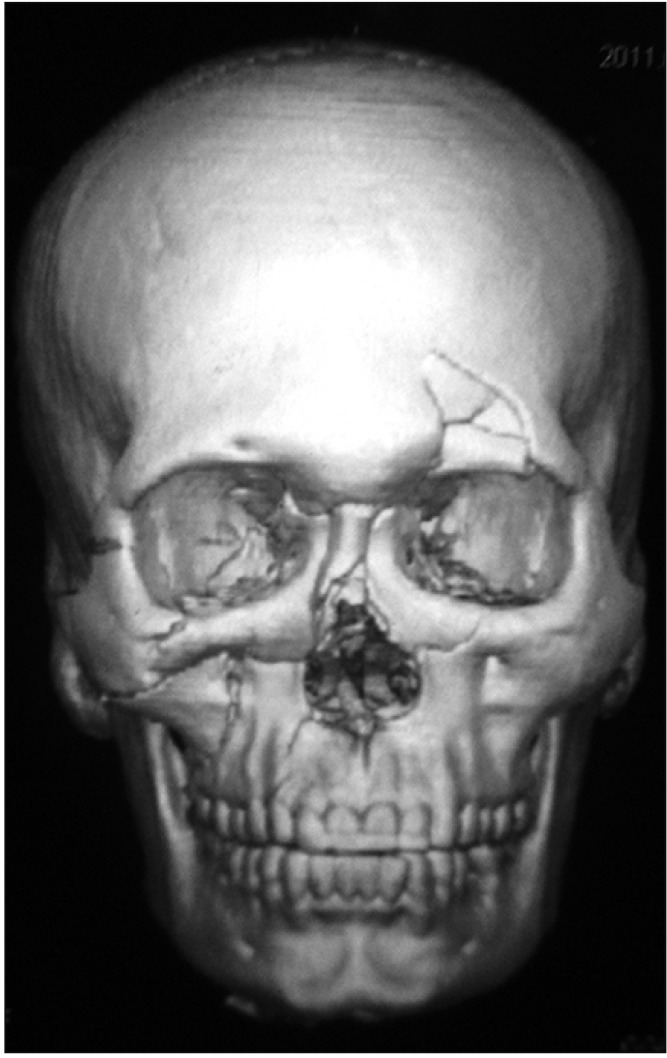
Oral and maxillofacial surgeons must gain mastery of various approaches to the midface due to the increasing incidence, complexity, and severity of presenting midfacial fractures. Unlike in the case of other body parts, the need to preserve facial aesthetics makes it more difficult for the surgeon to select an approach for managing the facial injuries. The midfacial degloving (MFD) approach is a combination of intraoral and intranasal incisions made to access the midface without any external incision. The aim of the present study was to evaluate the efficacy of MFD in maxillofacial surgery and to assess its advantages and complications.
MATERIALS AND METHODS
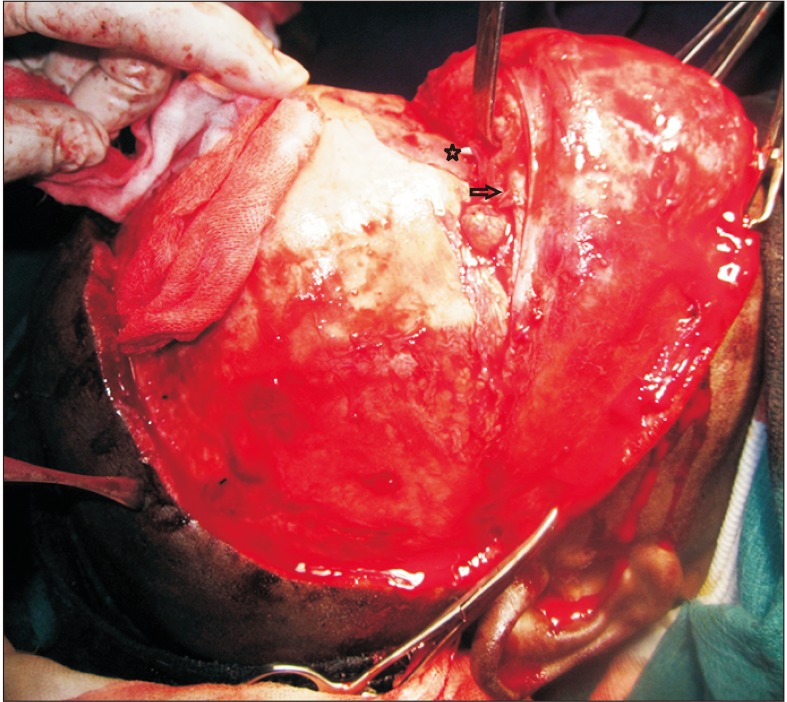
The MFD approach was used in five cases, with three cases treated with open reduction and internal fixation and two cases operated on for posttraumatic deformity. Nasal dorsum augmentation was completed in three cases and nasal osteotomy was performed in one case. The bicoronal flap technique was combined with MFD for frontal bone augmentation in one case. The intraoperative time required for flap completion and the ease of performing the planned procedures were noted. Postoperative evaluation was done for reduction, aesthetics, function, and complications.
RESULTS
Access was excellent for performing all planned procedures. Average time spent for flap elevation and exposure of the midface was 63 minutes. Complications like postoperative swelling, infraorbital nerve paresthesia, and intranasal crusting were all transient. No long-term complications like stenosis of the nose, sneer deformity, or weakness of the facial muscles were noticed. Additionally, no complications were noted when MFD was combined with bicoronal flap.
CONCLUSION
Though the MFD approach is technically demanding and takes more time than other facial approaches, it should be learned and applied by maxillofacial surgeons in selective cases, as it provides complete exposure of the midface without facial scarring.
MeSH Terms
Figure
Reference
-
1. Grover RS, Antonyshyn OM. (iv) Care of maxillofacial injuries in multiple trauma. Current Orthop. 2003; 17:274–286.
Article2. Price JC, Holliday MJ, Johns ME, Kennedy DW, Richtsmeier WJ, Mattox DE. The versatile midface degloving approach. Laryngoscope. 1988; 98:291–295. PMID: 2830446.
Article3. Har-El G. Medial maxillectomy via midfacial degloving approach. Oper Tech Otolaryngol Head Neck Surg. 1999; 10:82–86.
Article4. Casson PR, Bonanno PC, Converse JM. The midface degloving procedure. Plast Reconstr Surg. 1974; 53:102–103. PMID: 4809551.
Article5. Maniglia AJ. Indications and techniques of midfacial degloving. A 15-year experience. Arch Otolaryngol Head Neck Surg. 1986; 112:750–752. PMID: 3707738.
Article6. Kitagawa Y, Baur D, King S, Helman JI. The role of midfacial degloving approach for maxillary cysts and tumors. J Oral Maxillofac Surg. 2003; 61:1418–1422. PMID: 14663806.
Article7. Baumann A, Ewers R. Midfacial degloving: an alternative approach for traumatic corrections in the midface. Int J Oral Maxillofac Surg. 2001; 30:272–277. PMID: 11518347.
Article8. David DJ, Moore MH. Cantilever nasal bone grafting with miniscrew fixation. Plast Reconstr Surg. 1989; 83:728–732. PMID: 2648430.
Article9. Browne JD. The midfacial degloving procedure for nasal, sinus, and nasopharyngeal tumors. Otolaryngol Clin North Am. 2001; 34:1095–1104. viiiPMID: 11728935.
Article10. Lenarz T, Keiner S. [Midfacial degloving: an alternative approach to the frontobasal area, the nasal cavity and the paranasal sinuses]. Laryngorhinootologie. 1992; 71:381–387. German. PMID: 1388461.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Midfacial degloving approach in midfacial bone fracture : the report of cases
- Organized Hematoma of the Maxillary Sinus: Surgical Excision by Midfacial Degloving Approach
- Usefulness of midfacial degloving approach in oral & maxillofacial region
- Midfacial Degloving Approach
- Midfacial degloving approach for management of the maxillary fibrous dysplasia: a case report