Adopting Advance Directives Reinforces Patient Participation in End-of-Life Care Discussion
- Affiliations
-
- 1Department of Internal Medicine, Incheon St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Incheon, Korea.
- 2St. Vincent's Hospital Hospice Center, College of Medicine, The Catholic University of Korea, Suwon, Korea. miongsok@catholic.ac.kr
- 3Division of Hemato-oncology, Department of Internal Medicine, Hallym Universit Kangdong Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea.
- 4Department of Internal Medicine, St. Vincent's Hospital, College of Medicine, The Catholic University of Korea, Suwon, Korea.
- KMID: 2454353
- DOI: http://doi.org/10.4143/crt.2015.281
Abstract
- PURPOSE
In Korea, most terminal cancer patients have still not been included in end-of-life (EOL) discussions. The purpose of this study was to evaluate the proportion of patients participating in EOL discussions after adopting advance directives.
MATERIALS AND METHODS
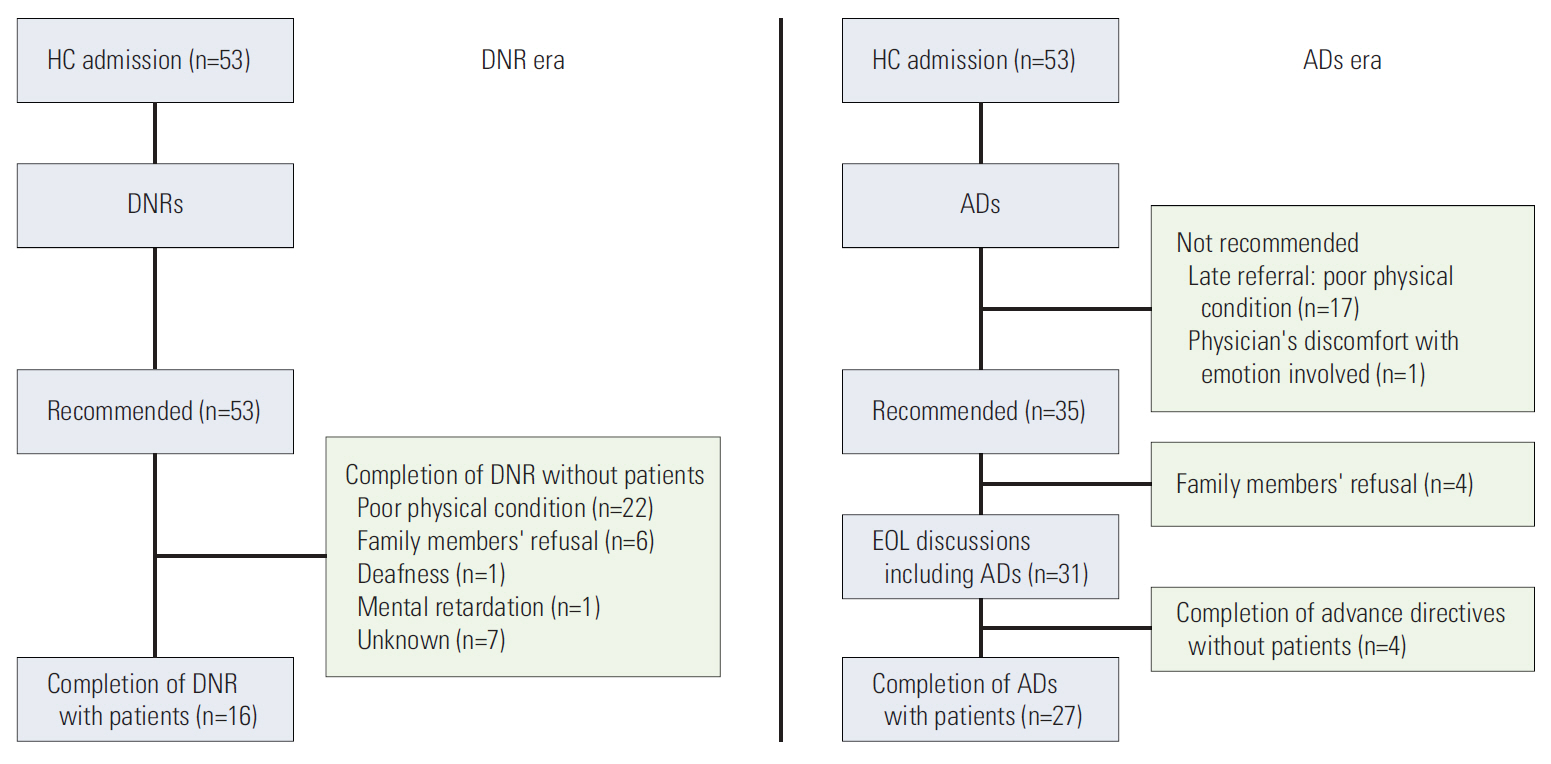
Medical records of 106 hospice patients between July 2012 and February 2013 were reviewed retrospectively. The proportion of patient participation in EOL discussions, barriers, and favorable factors for completion of advance directives, as well as outcomes of advance directives were evaluated.
RESULTS
Patient participation in EOL discussion had increased from 16/53 (30%) to 27/53 (51%) since adopting advance directives (p < 0.001). Median time between completion of an advance directive and death increased from 8 days (range, 0 to 22 days) to 14.5 days (range, 0 to 47 days). Patients' poor condition after late referral was the main barrier to missing EOL discussions; however, family members' concerns about patient's distress was also a main reason for excluding the patient from EOL discussions. In univariate analysis, patient age, education status, and time from diagnosis to completion of an advance directive influenced advance directive completion favorably. Following multivariate analysis, higher education and periods of more than 2 years from diagnosis to completion of an advance directive remained favorable (odds ratio [OR], 9.586, p=0.024 and OR, 70.312; p=0.002). Preferences of all patients regarding cardiopulmonary resuscitation or hemodialysis were carried out by physicians. Orders for nutrition and palliative sedation showed discordance, with concordance rates of 74.2% and 51.6%, respectively.
CONCLUSION
Our results suggested that the use of advance directive promote patient participation in EOL discussion.
MeSH Terms
Figure
Cited by 4 articles
-
Implication of the Life-Sustaining Treatment Decisions Act on End-of-Life Care for Korean Terminal Patients
Jung Sun Kim, Shin Hye Yoo, Wonho Choi, Yejin Kim, Jinui Hong, Min Sun Kim, Hye Yoon Park, Bhumsuk Keam, Dae Seog Heo
Cancer Res Treat. 2020;52(3):917-924. doi: 10.4143/crt.2019.740.A National Study of Life-Sustaining Treatments in South Korea: What Factors Affect Decision-Making?
So-Youn Park, Bomyee Lee, Jeong Yeon Seon, In-Hwan Oh
Cancer Res Treat. 2021;53(2):593-600. doi: 10.4143/crt.2020.803.Preparation and Practice of the Necessary Documents in Hospital for the “Act on Decision of Life-Sustaining Treatment for Patients at the End-of-Life”
Sun Kyung Baek, Hwa Jung Kim, Jung Hye Kwon, Ha Yeon Lee, Young-Woong Won, Yu Jung Kim, Sujin Baik, Hyewon Ryu
Cancer Res Treat. 2021;53(4):926-934. doi: 10.4143/crt.2021.326.The Situation of Life-Sustaining Treatment One Year after Enforcement of the Act on Decisions on Life-Sustaining Treatment for Patients at the End-of-Life in Korea: Data of National Agency for Management of Life-Sustaining Treatment
Ha Yeon Lee, Hwa Jung Kim, Jung Hye Kwon, Sun Kyung Baek, Young-Woong Won, Yu Jung Kim, Su Jin Baik, Hyewon Ryu
Cancer Res Treat. 2021;53(4):897-907. doi: 10.4143/crt.2021.327.
Reference
-
References
1. National Consensus Project for Quality Palliative Care. Clinical practice guidelines for quality palliative care, 3rd ed. [Internet]. Pittsburgh, PA: National Consensus Project for Quality Palliative Care;2013 [cited 2015 Oct 1]. Available from: http://www.nationalconsensusproject.org/NCP_Clinical_Practice_Guidelines_3rd_Edition.pdf.2. Heo DS. Patient autonomy and advance directives in Korea. J Korean Med Assoc. 2009; 52:865–70.
Article3. Keam B, Yun YH, Heo DS, Park BW, Cho CH, Kim S, et al. The attitudes of Korean cancer patients, family caregivers, oncologists, and members of the general public toward advance directives. Support Care Cancer. 2013; 21:1437–44.
Article4. Ngo-Metzger Q, McCarthy EP, Burns RB, Davis RB, Li FP, Phillips RS. Older Asian Americans and Pacific Islanders dying of cancer use hospice less frequently than older white patients. Am J Med. 2003; 115:47–53.
Article5. Andreis F, Rizzi A, Rota L, Meriggi F, Mazzocchi M, Zaniboni A. Chemotherapy use at the end of life: a retrospective single centre experience analysis. Tumori. 2011; 97:30–4.
Article6. Hong JH, Rho SY, Hong YS. Trends in the aggressiveness of end-of-life care for advanced stomach cancer patients. Cancer Res Treat. 2013; 45:270–5.
Article7. Keam B, Oh DY, Lee SH, Kim DW, Kim MR, Im SA, et al. Aggressiveness of cancer-care near the end-of-life in Korea. Jpn J Clin Oncol. 2008; 38:381–6.
Article8. Kim DY, Lee KE, Nam EM, Lee HR, Lee KW, Kim JH, et al. Do-not-resuscitate orders for terminal patients with cancer in teaching hospitals of Korea. J Palliat Med. 2007; 10:1153–8.
Article9. Oh DY, Kim JH, Kim DW, Im SA, Kim TY, Heo DS, et al. CPR or DNR? End-of-life decision in Korean cancer patients: a single center's experience. Support Care Cancer. 2006; 14:103–8.
Article10. Shim BY, Hong SI, Park JM, Cho HJ, Ok JS, Kim SY, et al. DNR (Do-Not-Resuscitate) order for terminal cancer patients at hospice ward. Korean J Hosp Palliat Care. 2004; 7:232–7.11. Kwon SH, Im SH, Cho KW, Cho E, Yoon SJ, Oh SY. Most advance directives written by patients with advanced cancer or their proxies request only minimally invasive treatments during end-of-life care. Am J Hosp Palliat Care. 2012; 29:622–6.
Article12. Park IK, Jun HJ, Park SJ, Lim GJ, Cho SJ, Song A, et al. Differences in end-of-life care decision making between patients with and without cancer. Am J Hosp Palliat Care. 2015; 32:797–801.
Article13. Anselm AH, Palda V, Guest CB, McLean RF, Vachon ML, Kelner M, et al. Barriers to communication regarding end-of-life care: perspectives of care providers. J Crit Care. 2005; 20:214–23.
Article14. Weiss GL, Hite CA. The do-not-resuscitate decision: the context, process, and consequences of DNR orders. Death Stud. 2000; 24:307–23.15. Danis M, Southerland LI, Garrett JM, Smith JL, Hielema F, Pickard CG, et al. A prospective study of advance directives for life-sustaining care. N Engl J Med. 1991; 324:882–8.
Article16. Heintz LL. Efficacy of advance directives in a general hospital. Hawaii Med J. 1997; 56:203–6.17. Brown BA. The history of advance directives: a literature review. J Gerontol Nurs. 2003; 29:4–14.
Article18. Nam YH, Seo IS, Lim JH, Choi JH, Kim JE, Choi JH, et al. Application of advance directives for patients with end stage renal disease. Korean J Nephrol. 2008; 27:85–93.19. Schmidt TA, Zive D, Fromme EK, Cook JN, Tolle SW. Physician orders for life-sustaining treatment (POLST): lessons learned from analysis of the Oregon POLST Registry. Resuscitation. 2014; 85:480–5.
Article20. Fromme EK, Zive D, Schmidt TA, Cook JN, Tolle SW. Association between physician orders for life-sustaining treatment for scope of treatment and in-hospital death in Oregon. J Am Geriatr Soc. 2014; 62:1246–51.
Article21. Schneiderman LJ, Kronick R, Kaplan RM, Anderson JP, Langer RD. Effects of offering advance directives on medical treatments and costs. Ann Intern Med. 1992; 117:599–606.
Article22. Reilly BM, Wagner M, Magnussen CR, Ross J, Papa L, Ash J. Promoting inpatient directives about life-sustaining treatments in a community hospital: results of a 3-year time-series intervention trial. Arch Intern Med. 1995; 155:2317–23.
Article23. Pautex S, Notaridis G, Derame L, Zulian GB. Preferences of elderly cancer patients in their advance directives. Crit Rev Oncol Hematol. 2010; 74:61–5.
Article24. Kong BH, An HJ, Kim HS, Ha SY, Kim IK, Lee JE, et al. Experience of advance directives in a hospice center. J Korean Med Sci. 2015; 30:151–4.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Current Status of End-of-Life Care in Korea and Legislation of Well-Dying Act
- Willingness to Write Advance Directives and Related Factors among Women University Students
- Effects of Awareness to Well-dying, Knowledge and Attitudes toward Advance-directives on Attitude toward End-of-life Care in Nursing Students
- Application of Advance Directives for Patients with End Stage Renal Disease
- Factors Affecting the End-of Life Care Competency of Tertiary Hospital Nurses