Impact of the 2015 Middle East Respiratory Syndrome Outbreak on Emergency Care Utilization and Mortality in South Korea
- Affiliations
-
- 1Department of Health Policy and Management, Seoul National University College of Medicine, Seoul, Korea. sy2376@snu.ac.kr
- 2Department of Emergency Medicine, Seoul National University Hospital, Seoul, Korea.
- 3Institute of Health Policy and Management, Seoul National University Medical Research Center, Seoul, Korea.
- KMID: 2452962
- DOI: http://doi.org/10.3349/ymj.2019.60.8.796
Abstract
- PURPOSE
In May 2015, South Korea experienced an epidemic of Middle East respiratory syndrome (MERS). This study investigated the impacts of MERS epidemic on emergency care utilization and mortality in South Korea.
MATERIALS AND METHODS
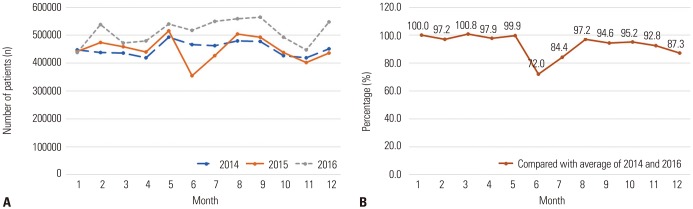
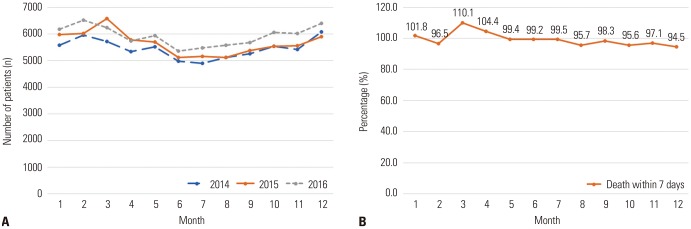
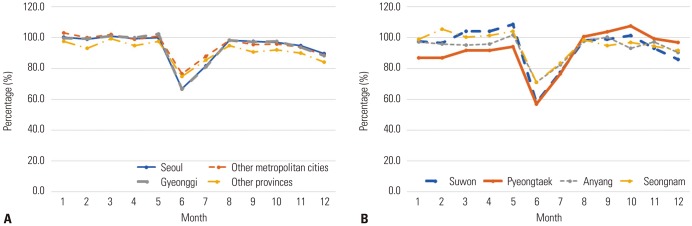
A natural experimental study was conducted using healthcare utilization and mortality data of the entire Korean population. The number of monthly emergency room (ER) visits was investigated to identify changes in emergency care utilization during the MERS epidemic; these trends were also examined according to patients' demographic factors, disease severity, and region. Deaths within 7 days after visiting an ER were analyzed to evaluate the impact of the reduction in ER visits on mortality.
RESULTS
The number of ER visits during the peak of the MERS epidemic (June 2015) decreased by 33.1% compared to the average figures from June 2014 and June 2016. The decrease was observed in all age, sex, and income groups, and was more pronounced for low-acuity diseases (acute otitis media: 53.0%; upper respiratory infections: 45.2%) than for high-acuity diseases (myocardial infarctions: 14.0%; ischemic stroke: 16.6%). No substantial changes were detected for the highest-acuity diseases, with increases of 3.5% for cardiac arrest and 2.4% for hemorrhagic stroke. The number of deaths within 7 days of an ER visit did not change significantly.
CONCLUSION
During the MERS epidemic, the number of ER visits decreased in all age, sex, and socioeconomic groups, and decreased most sharply for low-acuity diseases. Nonetheless, there was no significant change in deaths after emergency care.
Keyword
MeSH Terms
Figure
Cited by 4 articles
-
Pediatric Emergency Department Utilization and Coronavirus Disease in Daegu, Korea
Kyung Mi Jang, Ji Young Ahn, Hee Joung Choi, Sukhee Lee, Dongsub Kim, Dong Won Lee, Jae Young Choe
J Korean Med Sci. 2020;36(1):e11. doi: 10.3346/jkms.2021.36.e11.Impact of the COVID-19 Outbreak on Emergency Care Utilization in Patients with Acute Myocardial Infarction: a Nationwide Population-based Study
Ho Kyung Sung, Jin Hui Paik, Yu Jin Lee, Soo Kang
J Korean Med Sci. 2021;36(16):e111. doi: 10.3346/jkms.2021.36.e111.Impact of the Coronavirus Disease 2019 (COVID-19) Pandemic on Medical Use of Military Hospitals in Korea
Doran Yoon, Kyoung-Eun Kim, Ji Eun Lee, Mirang Kim, Jung-Hyun Kim
J Korean Med Sci. 2021;36(28):e204. doi: 10.3346/jkms.2021.36.e204.Long-term impact of coronavirus disease 2019 pandemic on emergency department utilization in a metropolitan emergency department in Korea
Seung Yeon Hwang, Jae Kwang Lee, Hyun Sik Ryu, Seong Soo Park, Jun Young Choi, Hye Ji Lee, Seung Ho Hur, Yeong Geun Park, Hyun Soo Choi
Pediatr Emerg Med J. 2021;8(2):57-65. doi: 10.22470/pemj.2021.00346.
Reference
-
1. Lu TH, Chou YJ, Liou CS. Impact of SARS on healthcare utilization by disease categories: implications for delivery of healthcare services. Health Policy. 2007; 83:375–381. PMID: 17445942.
Article2. Chang HJ, Huang N, Lee CH, Hsu YJ, Hsieh CJ, Chou YJ. The impact of the SARS epidemic on the utilization of medical services: SARS and the fear of SARS. Am J Public Health. 2004; 94:562–564. PMID: 15054005.
Article3. Fagbuyi DB, Brown KM, Mathison DJ, Kingsnorth J, Morrison S, Saidinejad M, et al. A rapid medical screening process improves emergency department patient flow during surge associated with novel H1N1 influenza virus. Ann Emerg Med. 2011; 57:52–59. PMID: 20947207.
Article4. Costello BE, Simon HK, Massey R, Hirsh DA. Pandemic H1N1 influenza in the pediatric emergency department: a comparison with previous seasonal influenza outbreaks. Ann Emerg Med. 2010; 56:643–648. PMID: 20363533.
Article5. Cowling BJ, Park M, Fang VJ, Wu P, Leung GM, Wu JT. Preliminary epidemiological assessment of MERS-CoV outbreak in South Korea, May to June 2015. Euro Surveill. 2015; 20:7–13. PMID: 26132767.
Article6. Cho SY, Kang JM, Ha YE, Park GE, Lee JY, Ko JH, et al. MERS-CoV outbreak following a single patient exposure in an emergency room in South Korea: an epidemiological outbreak study. Lancet. 2016; 388:994–1001. PMID: 27402381.
Article7. Ro JS, Lee JS, Kang SC, Jung HM. Worry experienced during the 2015 Middle East Respiratory Syndrome (MERS) pandemic in Korea. PLoS One. 2017; 12:e0173234. PMID: 28273131.
Article8. Park GE, Ko JH, Peck KR, Lee JY, Lee JY, Cho SY, et al. Control of an outbreak of Middle East respiratory syndrome in a tertiary hospital in Korea. Ann Intern Med. 2016; 165:87–93. PMID: 27272273.
Article9. Kim EY, Liao Q, Yu ES, Kim JH, Yoon SW, Lam WW, et al. Middle East respiratory syndrome in South Korea during 2015: risk-related perceptions and quarantine attitudes. Am J Infect Control. 2016; 44:1414–1416. PMID: 27130900.
Article10. Chen TA, Lai KH, Chang HT. Impact of a severe acute respiratory syndrome outbreak in the emergency department: an experience in Taiwan. Emerg Med J. 2004; 21:660–662. PMID: 15496687.
Article11. Heiber M, Lou WY. Effect of the SARS outbreak on visits to a community hospital emergency department. CJEM. 2006; 8:323–328. PMID: 17338843.
Article12. Paek SH, Kim DK, Lee JH, Kwak YH. The impact of Middle East respiratory syndrome outbreak on trends in emergency department utilization patterns. J Korean Med Sci. 2017; 32:1576–1580. PMID: 28875599.
Article13. Jeong H, Jeong S, Oh J, Woo SH, So BH, Wee JH, et al. Impact of Middle East respiratory syndrome outbreak on the use of emergency medical resources in febrile patients. Clin Exp Emerg Med. 2017; 4:94–101. PMID: 28717779.
Article14. Song SO, Jung CH, Song YD, Park CY, Kwon HS, Cha BS, et al. Background and data configuration process of a nationwide population-based study using the Korean National Health Insurance system. Diabetes Metab J. 2014; 38:395–403. PMID: 25349827.
Article15. Park CS, Choi EK, Han KD, Lee HJ, Rhee TM, Lee SR, et al. Association between adult height, myocardial infarction, heart failure, stroke and death: a Korean nationwide population-based study. Int J Epidemiol. 2018; 47:289–298. PMID: 29025084.
Article16. National Emergency Medical Center. Statistical yearbook of emergency medical service [Internet]. Seoul: National Emergency Medical Center;c2015. accessed on 2019 March 19. Available at: https://www.e-gen.or.kr/nemc/statistics_annual_report.do.17. Lee YJ, Shin SD, Lee EJ, Cho JS, Cha WC. Emergency department overcrowding and ambulance turnaround time. PLoS One. 2015; 10:e0130758. PMID: 26115183.
Article18. Seong SC, Kim YY, Khang YH, Park JH, Kang HJ, Lee H, et al. Data resource profile: the National Health Information Database of the National Health Insurance Service in South Korea. Int J Epidemiol. 2017; 46:799–800. PMID: 27794523.19. Khang YH, Yang S, Cho HJ, Jung-Choi K, Yun SC. Decomposition of socio-economic differences in life expectancy at birth by age and cause of death among 4 million South Korean public servants and their dependents. Int J Epidemiol. 2010; 39:1656–1666. PMID: 20647268.
Article20. Health Insurance Review and Assessment Service. Statistics of the healthcare fee [Internet]. Wonju: Health Insurance Review and Assessment Service;c2015. accessed on 2019 March 19. Available at: https://www.hira.or.kr/bbsDummy.do?pgmid=HIRAA020045030000&brdScnBltNo=4&brdBltNo=2376&pageIndex=2#none.21. Kang CK, Song KH, Choe PG, Park WB, Bang JH, Kim ES, et al. Clinical and epidemiologic characteristics of spreaders of Middle East respiratory syndrome coronavirus during the 2015 outbreak in Korea. J Korean Med Sci. 2017; 32:744–749. PMID: 28378546.
Article22. Kim KH, Tandi TE, Choi JW, Moon JM, Kim MS. Middle East respiratory syndrome coronavirus (MERS-CoV) outbreak in South Korea, 2015: epidemiology, characteristics and public health implications. J Hosp Infect. 2017; 95:207–213. PMID: 28153558.
Article23. Cho KY, Yoo JS. Estimate of economic loss of MERS epidemic [Internet]. Seoul: Korea Economic Research Institute;c2015. accessed on 2019 March 19. Available at: https://www.keri.org/web/www/research_0201?p_p_id=EXT_BBS&p_p_lifecycle=0&p_p_state=normal&p_p_mode=view&_EXT_BBS_struts_action=%2Fext%2Fbbs%2Fview_message&_EXT_BBS_messageId=350282.24. Kellermann AL, Weinick RM. Emergency departments, Medicaid costs, and access to primary care--understanding the link. N Engl J Med. 2012; 366:2141–2143. PMID: 22591255.25. Writing Group Members. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, et al. Heart disease and stroke statistics-2016 update: a report from the American Heart Association. Circulation. 2016; 133:e38–e360. PMID: 26673558.26. Korean Statistical Information Service (KOSIS). Health insurance statistics: monthly population [Internet]. Daejeon: KOSIS;c2018. accessed on 2019 March 19. Available at: http://kosis.kr/statHtml/statHtml.do?orgId=350&tblId=TX_35001_A007&vw_cd=MT_ZTITLE&list_id=350_35001_B&seqNo=&lang_mode=ko&language=kor&obj_var_id=&itm_id=&conn_path=MT_ZTITLE.27. Korean Statistical Information Service (KOSIS). The estimated population [Internet]. Daejeon: KOSIS;c2019. accessed on 2019 March 19. Available at: http://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1BPA001&vw_cd=MT_ZTITLE&list_id=A41_10&seqNo=&lang_mode=ko&language=kor&obj_var_id=&itm_id=&conn_path=MT_ZTITLE.28. Jung H, Do YK, Kim Y, Ro J. The impact of an emergency fee increase on the composition of patients visiting emergency departments. J Prev Med Public Health. 2014; 47:309–316. PMID: 25475198.29. Lee JY, Jo MW, Yoo WS, Kim HJ, Eun SJ. Evidence of a broken healthcare delivery system in Korea: unnecessary hospital outpatient utilization among patients with a single chronic disease without complications. J Korean Med Sci. 2014; 29:1590–1596. PMID: 25469056.
Article30. Stukel TA, Schull MJ, Guttmann A, Alter DA, Li P, Vermeulen MJ, et al. Health impact of hospital restrictions on seriously ill hospitalized patients: lessons from the Toronto SARS outbreak. Med Care. 2008; 46:991–997. PMID: 18725855.31. Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, et al. 2015 ACC/AHA/SCAI focused update on primary percutaneous coronary intervention for patients with ST-elevation myocardial infarction: an update of the 2011 ACCF/AHA/SCAI Guideline for percutaneous coronary intervention and the 2013 ACCF/AHA Guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Circulation. 2016; 133:1135–1147. PMID: 26490017.32. Furie KL, Jayaraman MV. 2018 Guidelines for the early management of patients with acute ischemic stroke. Stroke. 2018; 49:509–510. PMID: 29367335.
Article33. National Emergency Medical Center. Statistical yearbook of National Emergency Department Information System (NEDIS) [Internet]. Seoul: National Emergency Medical Center;c2015. accessed on 2019 March 19. Available at: https://www.e-gen.or.kr/nemc/statistics_annual_report.do?brdclscd=02.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- An Unexpected Outbreak of Middle East Respiratory Syndrome Coronavirus Infection in the Republic of Korea, 2015
- The Same Middle East Respiratory Syndrome-Coronavirus (MERS-CoV) yet Different Outbreak Patterns and Public Health Impacts on the Far East Expert Opinion from the Rapid Response Team of the Republic of Korea
- Institutional preparedness for infectious diseases and improving care
- Emergency medical services in response to the middle east respiratory syndrome outbreak in Korea
- 2015 MERS outbreak in Korea: hospital-to-hospital transmission