Korean J Ophthalmol.
2019 Jun;33(3):287-293. 10.3341/kjo.2017.0142.
Frequency of Ocular Diseases in Infants at a Tertiary Care Hospital
- Affiliations
-
- 1Department of Ophthalmology, Abbasi Shaheed Hospital, Karachi Medical and Dental College, Karachi, Pakistan. drerum007@yahoo.com
- KMID: 2448869
- DOI: http://doi.org/10.3341/kjo.2017.0142
Abstract
- PURPOSE
To determine the frequency of ocular diseases in infants visiting the ophthalmology department of a tertiary care hospital.
METHODS
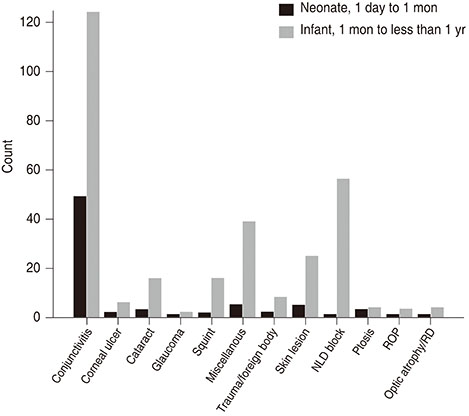
This was a cross-sectional descriptive study conducted in the department of ophthalmology, Abbasi Shaheed Hospital, from January 2015 to May 2016. The study included 377 infants ranging in age from 1 day to less than 1 year who were, selected by a nonprobability consecutive sampling technique. A detailed history was taken, and a complete ocular examination was performed. Descriptive statistics were used to calculate the mean and standard deviation for age. Frequencies were calculated for ocular diseases along with the percentages. Outcome variables included various congenital and acquired diseases such as conjunctivitis, congenital cataract, glaucoma, nasolacrimal duct blockage, squint, trauma, and fundus abnormalities.
RESULTS
The mean age of infants was 5.0 ± 3.7 months. There were 196 (52%) males and 181 (48%) females. The sample included 330 (87.5%) full term infants. Acquired ocular diseases occurred in 230 (61%) infants; and congenital diseases, in 147 (39%). The most common ocular disease was conjunctivitis, which occurred in 173 (46%) infants, followed by congenital blocked nasolacrimal duct, which occurred in 57 (15 %) infants. Conjunctivitis was more common among neonates than infants.
CONCLUSIONS
Acquired ocular diseases were more common than congenital ocular diseases. The most common ocular pathology was conjunctivitis, followed by congenital nasolacrimal duct obstruction, in infants. Conjunctivitis was more common in neonates than infants.
Keyword
MeSH Terms
Figure
Reference
-
1. Petrini J, Damus K, Russell R, et al. Contribution of birth defects to infant mortality in the United States. Teratology. 2002; 66:S3–S6.
Article2. Gilbert C, Foster A. Childhood blindness in the context of VISION 2020: the right to sight. Bull World Health Organ. 2001; 79:227–232.3. Li LH, Li N, Zhao JY, et al. Findings of perinatal ocular examination performed on 3573, healthy full-term newborns. Br J Ophthalmol. 2013; 97:588–591.
Article4. American Academy of Pediatrics. Section on Ophthalmology. American Association for Pediatric Ophthalmology and Strabismus. . Red reflex examination in neonates, infants, and children. Pediatrics. 2008; 122:1401–1404.5. Davidson S, Quinn GE. The impact of pediatric vision disorders in adulthood. Pediatrics. 2011; 127:334–339.
Article6. Rahi JS, Gilbert CE, Foster A, Minassian D. Measuring the burden of childhood blindness. Br J Ophthalmol. 1999; 83:387–388.
Article7. Kakar S, Bhalla P, Maria A, et al. Chlamydia trachomatis causing neonatal conjunctivitis in a tertiary care center. Indian J Med Microbiol. 2010; 28:45–47.
Article8. De Schryver A, Meheus A. Epidemiology of sexually transmitted diseases: the global picture. Bull World Health Organ. 1990; 68:639–654.9. Gilbert C, Fielder A, Gordillo L, et al. Characteristics of infants with severe retinopathy of prematurity in countries with low, moderate, and high levels of development: implications for screening programs. Pediatrics. 2005; 115:e518–e525.
Article10. Gul SS, Jamal M, Khan N. Ophthalmia neonatorum. J Coll Physicians Surg Pak. 2010; 20:595–598.11. Fatima K, Shahid E, Shaikh A. Frequency of common eye diseases in pediatric outpatient department of a tertiary care hospital. Pak J Ophthalmol. 2015; 31:154–157.12. Sethi S, Sethi MJ, Saeed N, Kundi NK. Pattern of common eye diseases in children attending outpatient eye department Khyber Teaching Hospital. Pak J Ophthalmol. 2008; 24:166–170.13. Fasih U, Rahman A, Shaikh A, et al. Pattern of common paediatric diseases at Spencer Eye Hospital. Pak J Ophthalmol. 2014; 30:10–14.14. Raosoft. Sample size calculator [Internet]. [place unknown]: Raosoft;2014. cited 2014 Dec 17. Available from: http://www.raosoft.com/samplesize.html.15. Bremond-Gignac D, Mariani-Kurkdjian P, Beresniak A, et al. Efficacy and safety of azithromycin 1.5% eye drops for purulent bacterial conjunctivitis in pediatric patients. Pediatr Infect Dis J. 2010; 29:222–226.
Article16. Smith AF, Waycaster C. Estimate of the direct and indirect annual cost of bacterial conjunctivitis in the United States. BMC Ophthalmol. 2009; 9:13.
Article17. Rose PW, Ziebland S, Harnden A, et al. Why do general practitioners prescribe antibiotics for acute infective conjunctivitis in children? Qualitative interviews with GPs and a questionnaire survey of parents and teachers. Fam Pract. 2006; 23:226–232.
Article18. Gogate P, Gilbert C, Zin A. Severe visual impairment and blindness in infants: causes and opportunities for control. Middle East Afr J Ophthalmol. 2011; 18:109–114.
Article19. Garg P, Qayum S, Dhingra P, Sidhu HK. Congenital ocular deformities-leading cause of childhood blindness: a clinical profile study. Indian J Clin Exp Ophthalmol. 2016; 2:21–26.20. Balmer A, Munier F. Leukokoria in a child: emergency and challenge. Klin Monbl Augenheilkd. 1999; 214:332–335.21. Lambert SR, Drack AV. Infantile cataracts. Surv Ophthalmol. 1996; 40:427–458.
Article22. Rahi JS, Dezateux C. British Congenital Cataract Interest Group. Measuring and interpreting the incidence of congenital ocular anomalies: lessons from a national study of congenital cataract in the UK. Invest Ophthalmol Vis Sci. 2001; 42:1444–1448.23. Adegbehingbe BO, Ajite KO, Adegbehingbe OO. Incidence of ocular congenital anomalies in a Nigerian Teaching Hospital. Orient J Med. 2005; 17:31–36.
Article24. Mehta S, Singh M, Chawla A, Agarwal A. Pattern of ocular diseases in children attending outpatient department of a rural medical college in Central India. Int J Sci Study. 2015; 3:57–60.25. Taqui AM, Syed R, Chaudhry TA, et al. Retinopathy of prematurity: frequency and risk factors in a tertiary care hospital in Karachi, Pakistan. J Pak Med Assoc. 2008; 58:186–190.26. National Institute of Population Studies. ICF International. Pakistan demographic and health survey 2012-13. Islamabad: National Institute of Population Studies;2013. p. 18–19.27. Darlow BA, Gilbert C, Quinn GE, et al. Promise and potential pitfalls of anti-VEGF drugs in retinopathy of prematurity. Br J Ophthalmol. 2009; 93:986.
Article28. Nizamani NB, Talpur KI, Awan F, et al. Results of a community-based screening programme for diabetic retinopathy and childhood blindness in district Hyderabad, Pakistan. BMJ Open Ophthalmol. 2017; 2:e000099.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Symptom Based Diagnosis of Infant under One Year in Outpatient Clinic
- Self-care and Physical Symptom by Gender in Korean Type2 Diabetic Patients
- Noise Level and Frequency Experienced by Premature Infants Receiving Incubator Care in the Neonatal Intensive Care Unit
- Ocular Manifestations of Venomous Snake Bite over a One-year Period in a Tertiary Care Hospital
- Functional Gastrointestinal Disorders in Patients with Gastrointestinal Symptoms