Clin Endosc.
2019 Mar;52(2):186-190. 10.5946/ce.2018.083.
First Characterization with Ultrasound Contrast Agent of a Fibrovascular Polyp Before Its Endoscopic Resection: A Case Report (with Videos)
- Affiliations
-
- 1Department of Hepatogastroenterology, University Hospital of Saint-Etienne, Saint-Priest en Jarez, France. nwilliet@yahoo.fr
- 2Department of General Surgery, University Hospital of Saint-Etienne, Saint-Priest en Jarez, France.
- 3Department of Pathology, University Hospital of Saint-Etienne, Saint-Priest en Jarez, France.
- KMID: 2447677
- DOI: http://doi.org/10.5946/ce.2018.083
Abstract
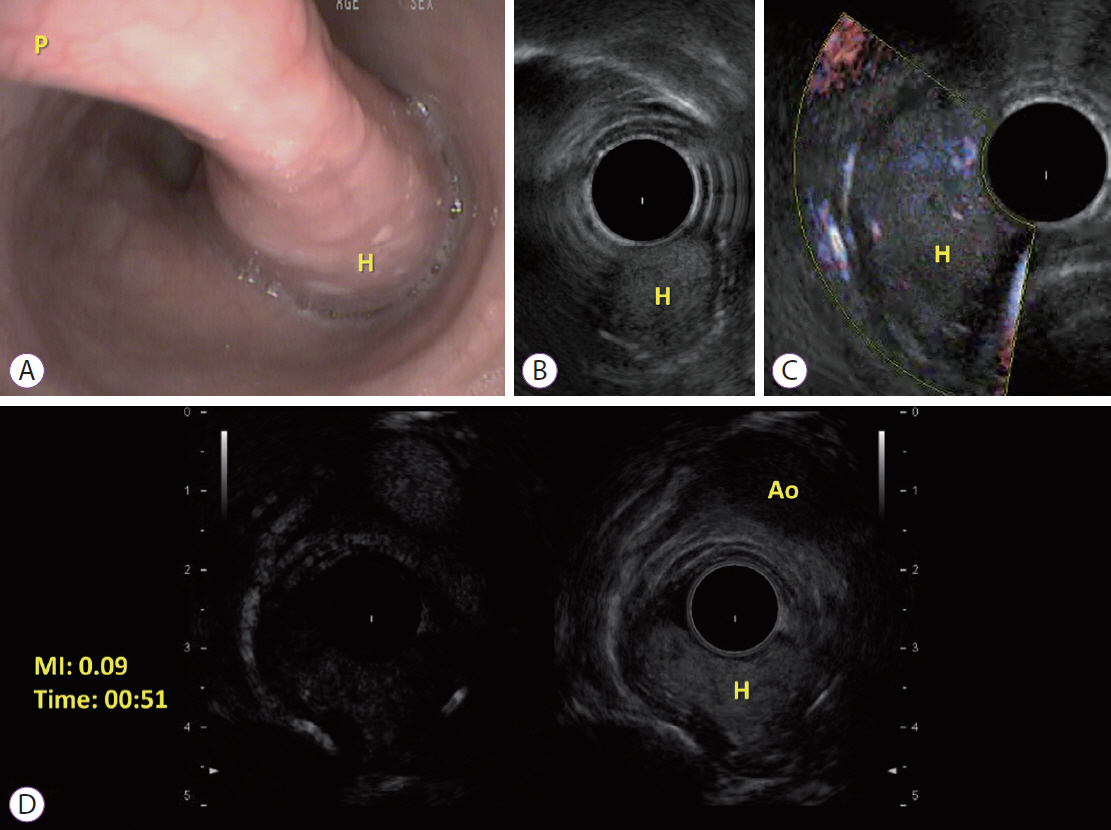
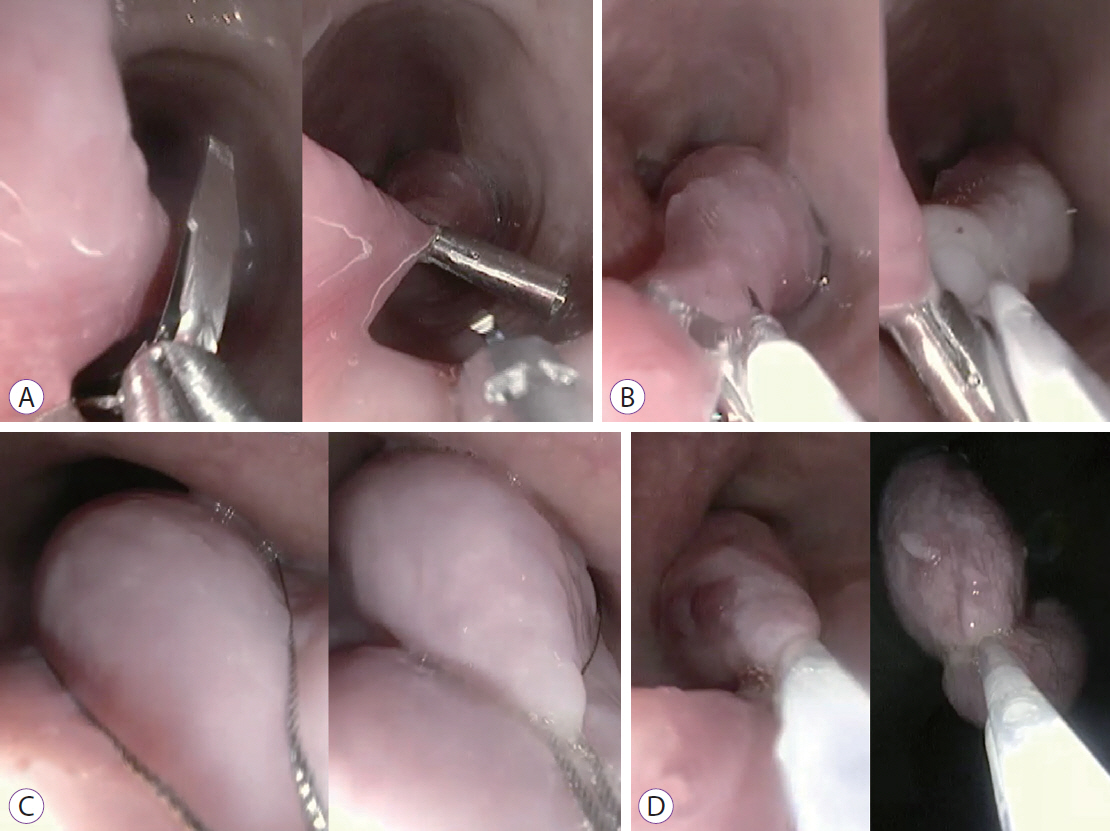
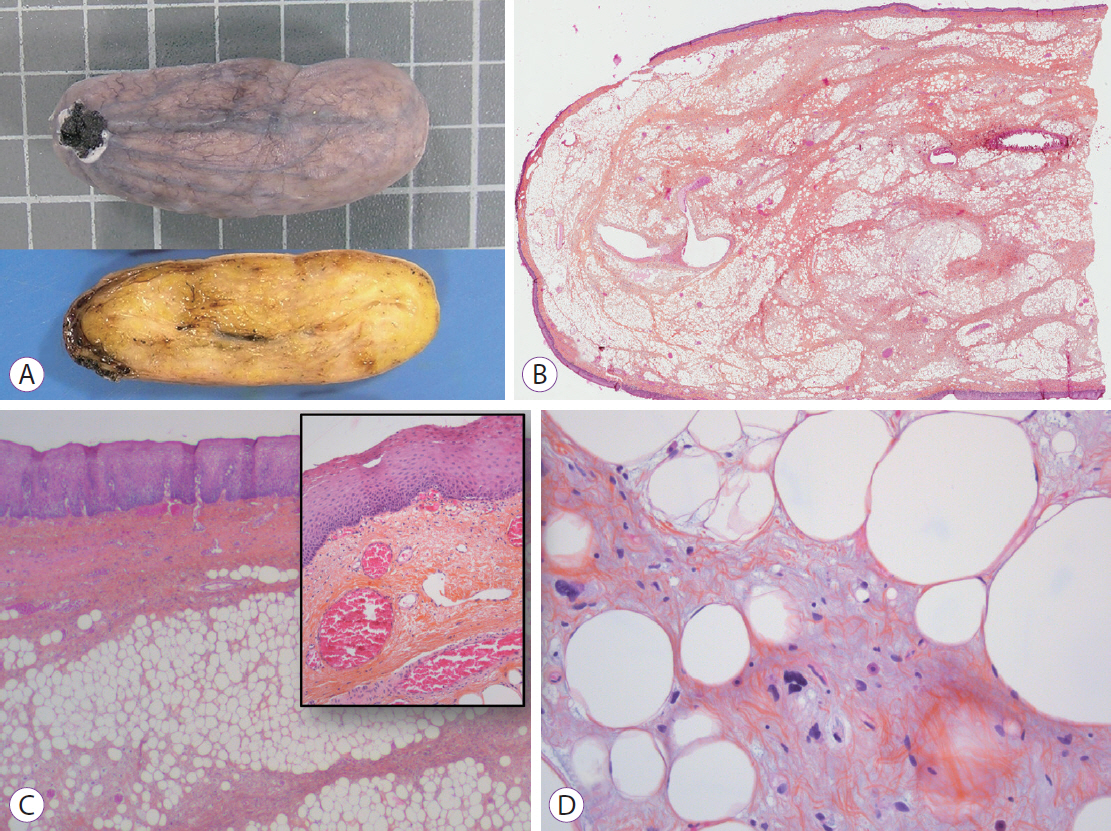
- We described for the first time the contrast enhancement of a giant fibrovascular esophageal polyp using ultrasound contrast agent, Sonovue® (Bracco, Milan, Italy) during echoendoscopy. Fine Doppler was unsuccessful in showing vascularization due to the mobile characteristic of the tumor. In contrast, via Sonovue®, tissue microcirculation was highlighted inside the entire head of the polyp, leading to better appreciate the risk of bleeding related to its resection. In a second part, we showed the feasibility of classic polypectomy for this giant polyp (5×5 cm) without complication and results of control endoscopy at 3 months. The present case is summarized in a video.
Keyword
Figure
Reference
-
1. Kitano M, Kudo M, Yamao K, et al. Characterization of small solid tumors in the pancreas: the value of contrast-enhanced harmonic endoscopic ultrasonography. Am J Gastroenterol. 2012; 107:303–310.
Article2. Fusaroli P, Spada A, Mancino MG, Caletti G, et al. Contrast harmonic echo-endoscopic ultrasound improves accuracy in diagnosis of solid pancreatic masses. Clin Gastroenterol Hepatol. 2010; 8:629–634. e1-e2.
Article3. Fusaroli P, Eloubeidi MA. Diagnosis of pancreatic cancer by contrast-harmonic endoscopic ultrasound (EUS): complementary and not competitive with EUS-guided fine-needle aspiration. Endoscopy. 2014; 46:380–381.
Article4. Gincul R, Palazzo M, Pujol B, et al. Contrast-harmonic endoscopic ultrasound for the diagnosis of pancreatic adenocarcinoma: a prospective multicenter trial. Endoscopy. 2014; 46:373–379.
Article5. Claudon M, Cosgrove D, Albrecht T, et al. Guidelines and good clinical practice recommendations for contrast enhanced ultrasound (CEUS) - update 2008. Ultraschall Med. 2008; 29:28–44.
Article6. Kannengiesser K, Mahlke R, Petersen F, et al. Contrast-enhanced harmonic endoscopic ultrasound is able to discriminate benign submucosal lesions from gastrointestinal stromal tumors. Scand J Gastroenterol. 2012; 47:1515–1520.
Article7. Fusaroli P, Kypraios D, Mancino MG, et al. Interobserver agreement in contrast harmonic endoscopic ultrasound. J Gastroenterol Hepatol. 2012; 27:1063–1069.
Article8. Park JS, Bang BW, Shin J, et al. A case of esophageal fibrovascular polyp that induced asphyxia during sleep. Clin Endosc. 2014; 47:101–103.
Article9. Lee SY, Chan WH, Sivanandan R, Lim DT, Wong WK. Recurrent giant fibrovascular polyp of the esophagus. World J Gastroenterol. 2009; 15:3697–3700.
Article10. Lorenzo D, Gonzalez JM, Barthet M. Endoscopic resection of a giant esophageal fibrovascular polyp. Endoscopy. 2016; 48 Suppl 1 UCTN:E69–E70.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Giant Fibrovascular Polyp of the Esophagus, Treated Successfully by Endoscopic Resection
- A Case of Fibrovascular Polyp in the Esophagus
- A Case of Large Fibrovascular Polyp of the Stomach
- Less invasive transoral resection of esophageal fibrovascular polyps: case reports
- A Case of Giant Fibrovascular Polyp of the Hypopharynx Removed by Transoral Approach