Korean J Radiol.
2019 Jun;20(6):956-966. 10.3348/kjr.2018.0891.
Changes in Right Ventricular Volume, Volume Load, and Function Measured with Cardiac Computed Tomography over the Entire Time Course of Tetralogy of Fallot
- Affiliations
-
- 1Department of Radiology and Research Institute of Radiology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea. ghw68@hanmail.net
- KMID: 2447074
- DOI: http://doi.org/10.3348/kjr.2018.0891
Abstract
OBJECTIVE
To characterize the changes in right ventricular (RV) volume, volume load, and function measured with cardiac computed tomography (CT) over the entire time course of tetralogy of Fallot (TOF).
MATERIALS AND METHODS
In 374 patients with TOF, the ventricular volume, ventricular function, and RV volume load were measured with cardiac CT preoperatively (stage 1), after palliative operation (stage 2), after total surgical repair (stage 3), or after pulmonary valve replacement (PVR) (stage 4). The CT-measured variables were compared among the four stages. After total surgical repair, the postoperative duration (POD) and the CT-measured variables were correlated with each other. In addition, the demographic and CT-measured variables in the early postoperative groups were compared with those in the late postoperative and the preoperative group.
RESULTS
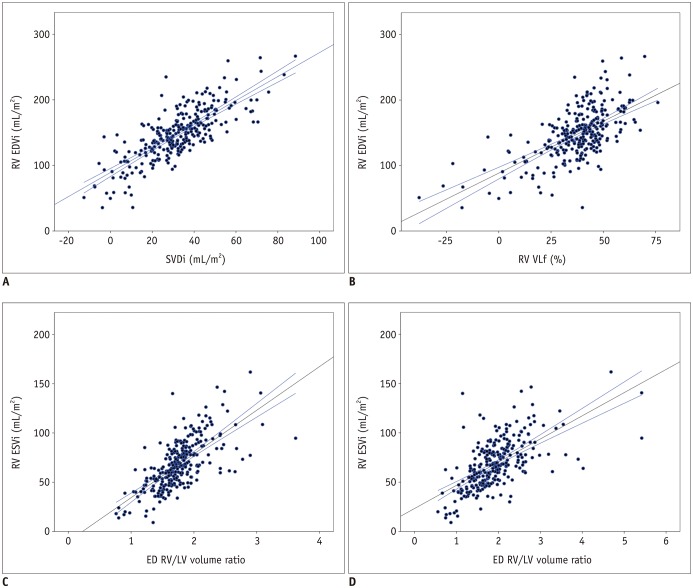
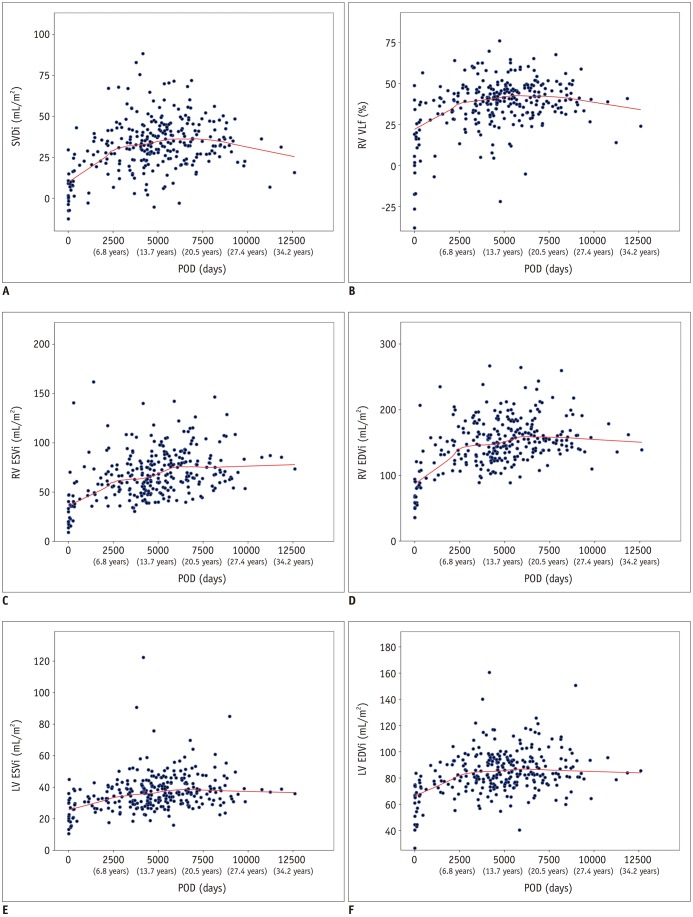
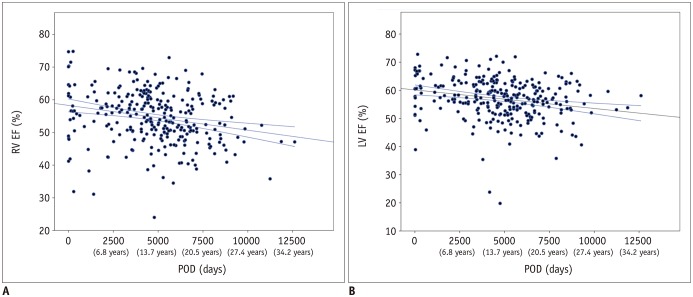
Significantly different CT-based measures were found between stages 1 and 3 (indexed RV end-diastolic volume [EDV], 63.6 ± 15.2 mL/m2 vs. 147.0 ± 38.5 mL/m2 and indexed stroke volume (SV) difference, 7.7 ± 10.3 mL/m2 vs. 32.2 ± 16.4 mL/m2; p < 0.001), and between stages 2 and 3 (indexed RV EDV, 72.4 ± 19.7 mL/m2 vs. 147.0 ± 38.5 mL/m2 and indexed SV difference, 5.7 ± 13.1 mL/m2 vs. 32.2 ± 16.4 mL/m2; p < 0.001). After PVR, the effect of RV volume load (i.e., indexed SV difference) was reduced from 32.2 mL/m2 to 1.7 mL/m2. Positive (0.2 to 0.8) or negative (−0.2 to −0.4) correlations were found among the CT-based measures except between the RV ejection fraction (EF) and the RV volume load parameters. With increasing POD, an early rapid increase was followed by a slow increase and a plateau in the indexed ventricular volumes and the RV volume load parameters. Compared with the preoperative data, larger ventricular volumes and lower EFs were observed in the early postoperative period.
CONCLUSION
Cardiac CT can be used to characterize RV volume, volume load, and function over the entire time course of TOF.
Keyword
MeSH Terms
Figure
Reference
-
1. Redington AN. Determinants and assessment of pulmonary regurgitation in tetralogy of Fallot: practice and pitfalls. Cardiol Clin. 2006; 24:631–639. viiPMID: 17098516.
Article2. Buechel ER, Dave HH, Kellenberger CJ, Dodge-Khatami A, Pretre R, Berger F, et al. Remodelling of the right ventricle after early pulmonary valve replacement in children with repaired tetralogy of Fallot: assessment by cardiovascular magnetic resonance. Eur Heart J. 2005; 26:2721–2727. PMID: 16214832.
Article3. Warnes CA, Williams RG, Bashore TM, Child JS, Connolly HM, Dearani JA, et al. ACC/AHA 2008 guidelines for the management of adults with congenital heart disease: a report of the American College of Cardiology/American Heart Association task force on practice guidelines (writing committee to develop guidelines on the management of adults with congenital heart disease). Circulation. 2008; 118:e714–e833. PMID: 18997169.
Article4. Kilner PJ, Geva T, Kaemmerer H, Trindade PT, Schwitter J, Webb GD. Recommendations for cardiovascular magnetic resonance in adults with congenital heart disease from the respective working groups of the European Society of Cardiology. Eur Heart J. 2010; 31:794–805. PMID: 20067914.
Article5. Grothoff M, Hoffmann J, Lehmkuhl L, Abdul-Khaliq H, Nitzsche S, Mahler A, et al. Time course of right ventricular functional parameters after surgical correction of tetralogy of Fallot determined by cardiac magnetic resonance. Clin Res Cardiol. 2011; 100:343–350. PMID: 21088843.
Article6. Śpiewak M, Małek ŁA, Petryka J, Biernacka EK, Hoffman P, Demkow M, et al. Stable right ventricular size and function during short-term follow-up in patients with pulmonary regurgitation after tetralogy of Fallot repair. Clin Radiol. 2013; 68:1206–1211. PMID: 23942263.
Article7. Wald RM, Valente AM, Gauvreau K, Babu-Narayan SV, Assenza GE, Schreier J, et al. Cardiac magnetic resonance markers of progressive RV dilation and dysfunction after tetralogy of Fallot repair. Heart. 2015; 101:1724–1730. PMID: 26276804.
Article8. Buddhe S, Shah A, Lai WW. Progression of right ventricular dilation in repaired tetralogy of Fallot. J Magn Reson Imaging. 2015; 41:730–737. PMID: 24591270.
Article9. Wijesekera VA, Raju R, Precious B, Berger AJ, Kiess MC, Leipsic JA, et al. Sequential right and left ventricular assessment in posttetralogy of Fallot patients with significant pulmonary regurgitation. Congenit Heart Dis. 2016; 11:606–614. PMID: 27225732.
Article10. Bhat M, Mercer-Rosa L, Fogel MA, Harris MA, Paridon SM, McBride MG, et al. Longitudinal changes in adolescents with TOF: implications for care. Eur Heart J Cardiovasc Imaging. 2017; 18:356–363. PMID: 28363199.
Article11. Goo HW, Park IS, Ko JK, Kim YH, Seo DM, Yun TJ, et al. CT of congenital heart disease: normal anatomy and typical pathologic conditions. Radiographics. 2003; 23 Spec No:S147–S165. PMID: 14557509.
Article12. Goo HW, Yang DH. Coronary artery visibility in free-breathing young children with congenital heart disease on cardiac 64-slice CT: dual-source ECG-triggered sequential scan vs. single-source non-ECG-synchronized spiral scan. Pediatr Radiol. 2010; 40:1670–1680. PMID: 20464385.
Article13. Goo HW. Coronary artery anomalies on preoperative cardiac CT in children with tetralogy of Fallot or Fallot type of double outlet right ventricle: comparison with surgical findings. Int J Cardiovasc Imaging. 2018; 34:1997–2009. PMID: 30051301.
Article14. Hong SH, Goo HW, Maeda E, Choo KS, Tsai IC. Asian Society of Cardiovascular Imaging Congenital Heart Disease Study Group. User-Friendly, Vendor-specific guideline for pediatric cardiothoracic computed tomography provided by the Asian Society of Cardiovascular Imaging (ASCI) congenital heart disease study group: part 1. Imaging techniques. Korean J Radiol. 2019; 20:190–204. PMID: 30672159.15. Lee E, Goo HW, Lee JY. Age- and gender- specific estimates of cumulative CT dose over 5 years using real radiation dose tracking data in children. Pediatr Radiol. 2015; 45:1282–1292. PMID: 25801905.16. Goo HW, Park SH. Semiautomatic three-dimensional CT ventricular volumetry in patients with congenital heart disease: agreement between two methods with different user interaction. Int J Cardiovasc Imaging. 2015; 31(Suppl 2):223–232. PMID: 26319216.
Article17. Goo HW. Serial changes in anatomy and ventricular function on dual-source cardiac computed tomography after the Norwood procedure for hypoplastic left heart syndrome. Pediatr Radiol. 2017; 47:1776–1786. PMID: 28879411.
Article18. Goo HW, Park SH. Computed tomography-based ventricular volumes and morphometric parameters for deciding the treatment strategy in children with a hypoplastic left ventricle: preliminary results. Korean J Radiol. 2018; 19:1042–1052. PMID: 30386136.
Article19. Goo HW. Semiautomatic three-dimensional threshold-based cardiac CT ventricular volumetry in repaired tetralogy of Fallot: comparison with cardiac magnetic resonance imaging. Korean J Radiol. 2019; 20:102–113. PMID: 30627026.20. Hui PKT, Goo HW, Du J, Ip JJK, Kanzaki S, Kim YJ, et al. Asian consortium on radiation dose of pediatric cardiac CT (ASCI-REDCARD). Pediatr Radiol. 2017; 47:899–910. PMID: 28435986.
Article21. Goo HW. Comparison of chest pain protocols for electrocardiography-gated dual-source cardiothoracic CT in children and adults: the effect of tube current saturation on radiation dose reduction. Korean J Radiol. 2018; 19:23–31. PMID: 29353996.
Article22. Goo HW, Allmendinger T. Combined electrocardiography- and respiratory-triggered CT of the lung to reduce respiratory misregistration artifacts between imaging slabs in free-breathing children: initial experience. Korean J Radiol. 2017; 18:860–866. PMID: 28860904.
Article23. Goo HW. Combined prospectively electrocardiography- and respiratory-triggered sequential cardiac CT in free-breathing children: success rate and image quality. Pediatr Radiol. 2018; 48:923–931. PMID: 29589058.24. Goo HW. Individualized volume CT dose index determined by cross-sectional area and mean density of the body to achieve uniform image noise of contrast-enhanced pediatric chest CT obtained at variable kV levels and with combined tube current modulation. Pediatr Radiol. 2011; 41:839–847. PMID: 21656275.
Article25. Goo HW. Is it better to enter a volume CT dose index value before or after scan range adjustment for radiation dose optimization of pediatric cardiothoracic CT with tube current modulation? Korean J Radiol. 2018; 19:692–703. PMID: 29962875.
Article26. Goo HW. CT radiation dose optimization and estimation: an update for radiologists. Korean J Radiol. 2012; 13:1–11. PMID: 22247630.
Article27. Sakrana AA, Al-Zubaidi SA, Nasr MM, Helmy EM, Al Ghamdi SS, Tahlawi ME. Cardiac magnetic resonance indices reflecting pulmonary regurgitation burden after tetralogy of Fallot repair. Clin Radiol. 2017; 72:900.e9–900.e15.28. Wald RM, Redington AN, Pereira A, Provost YL, Paul NS, Oechslin EN, et al. Refining the assessment of pulmonary regurgitation in adults after tetralogy of Fallot repair: should we be measuring regurgitant fraction or regurgitant volume? Eur Heart J. 2009; 30:356–361. PMID: 19164336.
Article29. DiLorenzo MP, Goldmuntz E, Nicolson SC, Fogel MA, Mercer-Rosa L. Early postoperative remodelling following repair of tetralogy of Fallot utilising unsedated cardiac magnetic resonance: a pilot study. Cardiol Young. 2018; 28:697–701. PMID: 29444724.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Volumetric Quantitation of Pulmonary Regurgitation and Right Ventricular Function in Postoperative Tetralogy of Fallot by Echocardiography and Magnetic Resonance Imaging
- Use of Cardiac Computed Tomography for Ventricular Volumetry in Late Postoperative Patients with Tetralogy of Fallot
- Echocardiographic Findings in Tetralogy of Fallot
- Assessment of Left Ventricular Volume and Function Using Real-Time 3D Echocardiography versus Angiocardiography in Children with Tetralogy of Fallot
- Semiautomatic Three-Dimensional Threshold-Based Cardiac Computed Tomography Ventricular Volumetry in Repaired Tetralogy of Fallot: Comparison with Cardiac Magnetic Resonance Imaging