Clin Nutr Res.
2019 Apr;8(2):101-118. 10.7762/cnr.2019.8.2.101.
An Investigation of the Prevalence and Causes of Malnutrition in Iran: a Review Article and Meta-analysis
- Affiliations
-
- 1Department of Cardiology, Faculty of Medicine, Zanjan University of Medical Sciences, Zanjan 45156-13191, Iran.
- 2Department of Parasitology, Faculty of Medicine, Shiraz University of Medical Sciences, Fars 71348-14336, Iran.
- 3Student Research Committee, Proteomics Research Center, Shahid Beheshti University of Medical Sciences, Tehran 19839-63113, Iran.
- 4Social Determinants of Health Research Center, Yasuj University of Medical Sciences, Yasuj 75919-51176, Iran. pourmahmoudi@gmail.com
- 5Department of Nutrition, Yasuj University of Medical Sciences, Yasuj 75918-75114, Iran.
- KMID: 2444227
- DOI: http://doi.org/10.7762/cnr.2019.8.2.101
Abstract
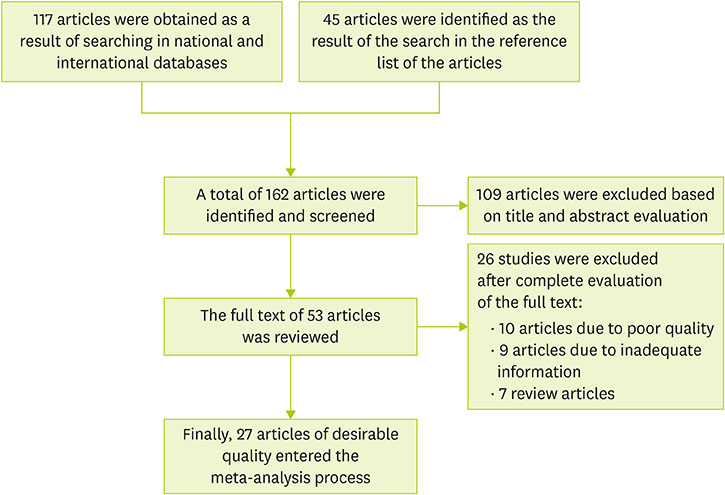
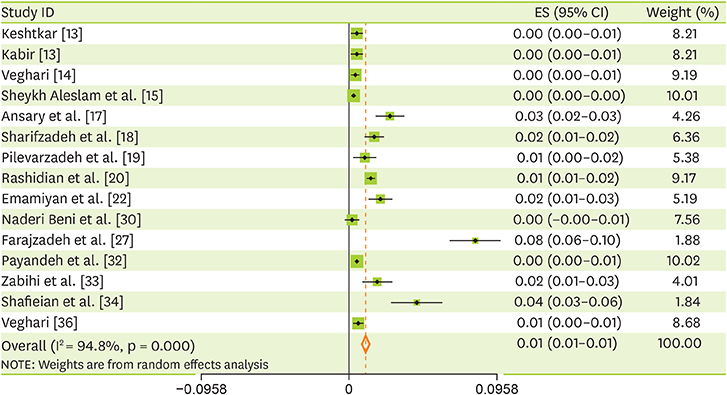
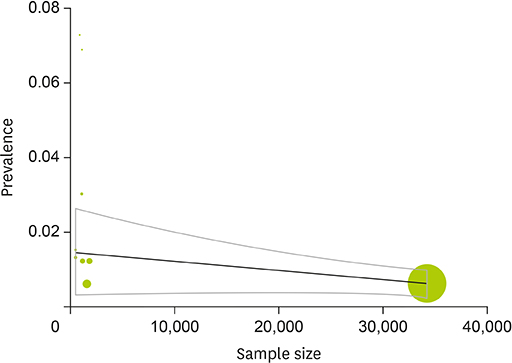
- Malnutrition is one of the most important health issues in developing countries, which might have adverse effects on the physical and intellectual health of children. The search process was started to find Persian and English articles published until September 2017 regarding the prevalence of malnutrition in children under the age of six in Iran using national and international databases including SID, Magiran, Irandoc, IranMedex, PubMed, Medline, Scopus, and ISI Web of Science. The data were analyzed using meta-analysis methods and the random effects model. The heterogeneity of studies was analyzed using the I² index. The data were analyzed using R and STATA software (ver. 11.2). Twenty seven articles conducted from 2002 to 2016 were collected to be included in the meta-analysis process. The total sample size was 161,941 patients in an age range of 0-6 years. The final estimate of the prevalence of different forms of malnutrition through meta-analysis of data extracted from studies in Iran was as follows: severe underweight (1%; 95% confidence interval [CI], 1-1), moderate underweight (6%; 95% CI, 5-7), mild underweight (25%; 95% CI, 21-28), severe short stature (3%; 95% CI, 2-3), moderate short stature (8%; 95% CI, 6-9), mild short stature (21%; 95% CI, 17-24), severe slimness (1%; 95% CI, 1-1), moderate slimness (5%; 95% CI, 4-5) and mild slimness (20%; 95% CI, 17-24). Considering that the prevalence of malnutrition is relatively high in Iran, health authorities should plan to improve the nutritional status of children.
Keyword
MeSH Terms
Figure
Reference
-
1. Moridi G, Fathi M. The prevalence of malnutrition and associated factors in children under 5 years age in Iran. J Nurse Midwifery. 2009; 19:47–53.2. Soheyli Azad AA, Zamaniyan M. Prevalence of malnutrition and its related factors among 0–36 month children of Nahavand, 2002. Res Med. 2004; 28:53–58.3. Malek M, Sharifiyan M. Malnutrition and failure to thrive. Iran J Pediatr. 1990; 3:203–231.4. Reshad A. Failure to thrive. Med Ther. 1991; 8:42–47.5. Berkman DS, Lescano AG, Gilman RH, Lopez SL, Black MM. Effects of stunting, diarrhoeal disease, and parasitic infection during infancy on cognition in late childhood: a follow-up study. Lancet. 2002; 359:564–571.
Article6. Gheyraie H. The state of the world's children 2003. New York (NY): United Nations International Children's Emergency Fund;2002.7. Keshavarz A. Translation nutrition and public health from the perspective of epidemiology and prevention policies. Tehran: University of Tehran;1994.8. World Health Organization. Investing in health research and development. Report of ad hoc committee on research. Geneva: World Health Organization;1996.9. Ministry of Health and Medical Education. Anthropometric nutrition indicator. Tehran: Ministry of Health and Medical Education;1383.10. Alaei F. Textbook of pediatric nursing (healthy child). Tehran: Tehran Salemi Publishing;2002.11. Nojomi M, Kafash A, Najmabadi SH. Study of frequency of malnutrition risk factors in under 5 years children in Karaj, 2001–2002. J Iran Univ Med Sci. 2003; 10:123–132.12. Eftekhari M, Mozaffari H. The prevalence of malnutrition in children under 5 years in Lar and its outskirts. J Yazd Univ Med Sci. 2006; 5:11–21.13. Kabir MJ, Keshtkar AA, Lashkar-Blueki F. Prevalence of malnutrition in children under 2 years old and its relationship with mothers background variables in Golestan province. J Gorgan Univ Med Sci. 2006; 8:32–39.14. Veghari G. The comparison of under-five-children's nutrition status among ethnic groups in North of Iran, 1998–2013; results of a three stages cross-sectional study. Iran J Pediatr. 2015; 25:e2004.
Article15. Sheykh Aleslam R, Naghavi M, Abd Elahi Z, Zarati M, Vaseghi S, Sadeghi Ghotbabadi F, Kolahdooz F, Samadpour K, Minaei M, Arabshahi S. Current status and the 10 years trend in the malnutrition indexes of children under 5 years in Iran. Iran J Epidemiol. 2008; 4:21–28.16. Hooshyarrad A, Dorosti Motlag AR, Kalantary N, Abdolahi M, Abtahi M. The prevalence of stunting, underweight, wasting and overweight in Iranian children under 5 years. J Nutr Sci Food Ind. 2008; 3:49–56.17. Ansary H, Zareban E, Norouzi M, Fallah S, Lotfi B. Predictors of malnutrition among Zahedan's children, age ranging from 2–5 years old in 2007–2008. J Shahrekord Univ Med Sci. 2009; 11:46–54.18. Sharifzadeh G, Raghebi S, Zeraatkar V, Moodi M. Prevalence of malnutrition in under 6 years old children in south Khorasan 2006. J Birjand Univ Med Sci. 2006; 15:73–80.19. Pilevarzadeh M, Salari S, Rafati F, Rezaie H, Shamsi A, Abootalebi A.. Prevalence of malnutrition based on anthropometric indices among 24–36 month children of Jiroft, 2009. J Health Care. 2010; 12:36–40.20. Rashidian A, Khosravi A, Khabiri R, Khodayari-Moez E, Elahi E, Arab M, Radaie Z. Islamic Republic of Iran's Multiple Indicator Demographic and Health Survey (IrMIDHS) 2010. Tehran: Ministry of Health and Medical Education;2012.21. Mahyar A, Ayazi P, Fallahi M, Haji Seiid Javadi T, Farkhondehmehr B, Javadi A, Kalantari Z. Prevalence of underweight, stunting and wasting among children in Qazvin, Iran. Iran J Pediatr Soc. 2010; 2:37–43.22. Emamiyan MH, Gorgani N, Fateh M. Malnutrition status in children of Shahroud, Iran. Knowl Health. 2011; 6:7–14.23. Fesharakinia A, Sharifzadeh G. Prevalence of malnutrition in under 5-year old children in Birjand city in 2011. J Birjand Univ Med Sci. 2013; 20:77–84.24. Nouri Saeidlou S, Babaei F, Ayremlou P. Prevalence of malnutrition in children under 5 years old in Salmas, and comparing to Ravansar and Samirom. Razi J Med Sci. 2014; 21:47–53.25. Mohammadinia N, Sharifi Poor H, Rezaei MA, Heydari Khayat N. The prevalence of malnutrition among children under 5 years old referred to health centers in Iranshahr during 2010–2011. J Occup Health Epidemiol. 2012; 1:139–149.
Article26. Sheykhi M, Eftekhari Nia M, Esmaillzadeh A. Prevalence of stunting, underweight and wasting according to National Center for Health Statistics criteria in rural children under 6 in Zahedan, Iran, in 2010. Health Syts Res. 2013; 9:153–158.27. Farajzadeh Z, Saadatjoo SA, Hosseini S, Hasani H, Taghizadeh M, Alahyari F. Prevalence of malnutrition in preschool children in Birjand City in 2010. Mod Care J. 2012; 9:122–128.28. Farrokh-Eslamlou H, Oshnouei S, Ahmadi N, Babaei F. Geografical distribution of nutrition deficiency among children under five years old in the west Azerbaijan Provience, Iran. J Urmia Univ Med Sci. 2013; 24:201–209.29. Ramezanpour M, Akabery A, Khoshnoud E, Shoraka H. Investigation into malnutrition prevalence rate and effective factors on under five year old children in Maneh Semelghan city (2012–2013). J North Khorasan Univ Med Sci. 2013; 5:365–373.30. Naderi Beni M, Lak R, Jazaeri SA, Eftekhar Ardebili H. Prevalence of malnutrition under five years in Chadegan (Area District City) Iran 2011. Iran J Epidemiol. 2013; 9:22–28.31. Gholami A, Shororzi L, Rastegsri A, Taghavi A. Prevalence of malnutrition among rural children aged 3 to 6 years old of Neyshabur. J Neyshabur Univ Med Sci. 2013; 1:10–13.32. Payandeh A, Saki A, Safarian M, Tabesh H, Siadat Z. Prevalence of malnutrition among preschool children in northeast of Iran, a result of a population based study. Glob J Health Sci. 2013; 5:208–212.
Article33. Zabihi A, Rafati Rahimzadeh M, Jafarian Amiri SR, Sajadi P, Asgari S. Effect of growth indices on malnutrition in infants from health medical centers of Babol, Iran 2011–2012. J Babol Univ Med Sci. 2013; 15:59–66.34. Shafieian T, Rafati Rahimzadeh M, Jafarian Amiri SR, Sajadi P, Asgari S. Determinants of nutritional status in children living in Mashhad, Iran. Int J Pediatr. 2013; 1:9–18.35. Kavosi E, Hassanzadeh Rostami Z, Kavosi Z, Nasihatkon A, Moghadami M, Heidari M. Prevalence and determinants of under-nutrition among children under six: a cross-sectional survey in Fars province, Iran. Int J Health Policy Manag. 2014; 3:71–76.
Article36. Veghari G. The comparison of under-five-children's nutrition status among ethnic groups in north of Iran, 1998–2013; Results of a Three Stages Cross-Sectional Study. Iran J Pediatr. 2015; 25:e2004.
Article37. Ahmadipour H, Mirzaesmaeili S. The frequency of malnutrition and its related factors in 2–5-year old children of Kerman suburb area in-2014. J Health Dev. 2016; 5:188–194.38. Rollet SR, Gray ES, Previl H, Forrester JE. Prevalence of malnutrition in children under five and school-age children in Milot Valley, Haiti. Public Health. 2014; 128:1094–1098.
Article39. So M, Ellenikiotis YA, Husby HM, Paz CL, Seymour B, Sokal-Gutierrez K. Early childhood dental caries, mouth pain, and malnutrition in the Ecuadorian amazon region. Int J Environ Res Public Health. 2017; 14:550.
Article40. Akombi BJ, Agho KE, Merom D, Renzaho AM, Hall JJ. Child malnutrition in sub-Saharan Africa: a meta-analysis of demographic and health surveys (2006–2016). PLoS One. 2017; 12:e0177338.
Article41. Sawyer W, Ordinioha B, Abuwa P. Nutrition intervention program and childhood malnutrition: a comparative study of two rural riverine communities in bayelsa state, Nigeria. Ann Med Health Sci Res. 2013; 3:422–426.
Article42. Abdulahi A, Shab-Bidar S, Rezaei S, Djafarian K. Nutritional status of under five children in Ethiopia: a systematic review and meta-analysis. Ethiop J Health Sci. 2017; 27:175–188.
Article43. Kimani-Murage EW, Muthuri SK, Oti SO, Mutua MK, van de Vijver S, Kyobutungi C. Evidence of a double burden of malnutrition in urban poor settings in Nairobi, Kenya. PLoS One. 2015; 10:e0129943.
Article44. Juma OA, Enumah ZO, Wheatley H, Rafiq MY, Shekalaghe S, Ali A, Mgonia S, Abdulla S. Prevalence and assessment of malnutrition among children attending the Reproductive and Child Health clinic at Bagamoyo District Hospital, Tanzania. BMC Public Health. 2016; 16:1094.
Article45. Ewusie JE, Beyene J, Ahiadeke C, Hamid JS. Malnutrition in pre-school children across different geographic areas and socio-demographic groups in Ghana. Matern Child Health J. 2017; 21:797–808.
Article46. Chataut J, Khanal K. Assessment of nutritional status of children under five years of age in rural Nepal. Kathmandu Univ Med J (KUMJ). 2016; 14:73–77.47. Rohner F, Woodruff BA, Aaron GJ, Yakes EA, Lebanan MA, Rayco-Solon P, Saniel OP. Infant and young child feeding practices in urban Philippines and their associations with stunting, anemia, and deficiencies of iron and vitamin A. Food Nutr Bull. 2013; 34:Suppl. S17–S34.
Article48. Rahman MS, Howlader T, Masud MS, Rahman ML. Association of low-birth weight with malnutrition in children under five years in Bangladesh: do mother's education, socio-economic status, and birth interval matter? PLoS One. 2016; 11:e0157814.
Article49. Manjunath R, K JK, Kulkarni P, Begum K, R GM. Malnutrition among under-five children of kadukuruba tribe: need to reach the unreached. J Clin Diagn Res. 2014; 8:JC01–JC04.
Article50. Tsigga M, Grammatikopoulou MG. Assessing the silent epidemic of malnutrition in Palestinian preschool children. J Epidemiol Glob Health. 2012; 2:181–191.
Article51. United Nations International Children's Emergency Fund. The state of world's children 2012. Children in an urban world. 2012. cited 2012 February. Available from http://www.unicef.org/sowc2012/pdfs/SOWC%202012-.52. de Onis M, Blössner M. The World Health organization global database on child growth and malnutrition: methodology and applications. Int J Epidemiol. 2003; 32:518–526.
Article53. United Nations International Children's Emergency Fund. Levels and trends in child malnutrition. 2015. cited 2015 September. Available from www.unicef.org/media/files/JME_2015_edition_Sept_2015.54. Das SK, Chisti MJ, Sarker MH, Das J, Ahmed S, Shahunja KM, Nahar S, Gibbons N, Ahmed T, Faruque AS, Rahman M, J Fuchs G 3rd, Al Mamun A, John Baker P. Long-term impact of changing childhood malnutrition on rotavirus diarrhoea: two decades of adjusted association with climate and socio-demographic factors from urban Bangladesh. PLoS One. 2017; 12:e0179418.
Article55. Loret de Mola C, Quispe R, Valle GA, Poterico JA. Nutritional transition in children under five years and women of reproductive age: a 15-years trend analysis in Peru. PLoS One. 2014; 9:e92550.
Article56. United Nations International Children's Emergency Fund. Progress for children report–a statistical review. 2007. cited 2007 December. Available from http://www.unicef.org/india/media_3766.htm.57. Subramanyam MA, Kawachi I, Berkman LF, Subramanian SV. Socioeconomic inequalities in childhood undernutrition in India: analyzing trends between 1992 and 2005. PLoS One. 2010; 5:e11392.
Article58. United Nations International Children's Emergency Fund. Multiple Indicator Cluster Survey (MICS) in the Islamic Republic of Iran. New York (NY): United Nations International Children's Emergency Fund;1995.59. Ministry of Health and Medical Education. The first national Anthropometric Nutritional Indicators Survey (ANIS) among children under 5 years. Tehran: Ministry of Health and Medical Education;1998.60. Sheikholeslam R, Naghavi M, Abdollahi Z, Zarati M, Vaseghi S, Sadeghi Ghotbabadi F, Kolahdooz F, Samadpour K, Minaei M, Arabshahi S. Current status and the 10 years trend in the malnutrition indexes of children under 5 years in Iran. Iran J Epidemiol. 2008; 4:21–28.61. United Nations International Children's Emergency Fund. Progress for children: a report card on nutrition. 2006. cited 2006 May. Available from http://www.childinfo.org/malnutrition.html/.62. Fotso JC. Urban-rural differentials in child malnutrition: trends and socioeconomic correlates in sub-Saharan Africa. Health Place. 2007; 13:205–223.
Article63. Smith LC, Ruel MT, Ndiaye A. Why is child malnutrition lower in urban than in rural areas? Evidence from 36 developing countries. World Dev. 2005; 33:1285–1305.
Article64. Sahn DE, Stifel DC. Urban–rural inequality in living standards in Africa. J Afr Econ. 2003; 12:564–597.
Article65. Ghana Health Service. Ghana health service nutrition and malaria control for child survival project. 2006. cited 2013 October. Available from http://www.ghanahealthservice.org.66. Akhtar S. Malnutrition in South Asia-a critical reappraisal. Crit Rev Food Sci Nutr. 2016; 56:2320–2330.
Article67. Akombi B, Agho KE, Hall JJ, Wali N, Renzaho A, Merom D. Stunting, wasting and underweight in sub-saharan Africa: a systematic review. Int J Environ Res Public Health. 2017; 14:863.
Article68. Arthur SS, Nyide B, Soura AB, Kahn K, Weston M, Sankoh O. Tackling malnutrition: a systematic review of 15-year research evidence from INDEPTH health and demographic surveillance systems. Glob Health Action. 2015; 8:28298.
Article69. Ergin F, Okyay P, Atasoylu G, Beşer E. Nutritional status and risk factors of chronic malnutrition in children under five years of age in Aydin, a western city of Turkey. Turk J Pediatr. 2007; 49:283–289.70. Renzaho AM, Gibbons C, Swinburn B, Jolley D, Burns C. Obesity and undernutrition in sub-Saharan African immigrant and refugee children in Victoria, Australia. Asia Pac J Clin Nutr. 2006; 15:482–490.71. Belachew T, Hadley C, Lindstrom D, Gebremariam A, Lachat C, Kolsteren P. Food insecurity, school absenteeism and educational attainment of adolescents in Jimma Zone Southwest Ethiopia: a longitudinal study. Nutr J. 2011; 10:29.
Article72. Ali D, Saha KK, Nguyen PH, Diressie MT, Ruel MT, Menon P, Rawat R. Household food insecurity is associated with higher child undernutrition in Bangladesh, Ethiopia, and Vietnam, but the effect is not mediated by child dietary diversity. J Nutr. 2013; 143:2015–2021.
Article73. Rimaz S, Moghtaderi A, Shidfar F, Poor Malek F. Prevalence and determiants of proten energymalnutriton among children under the age of 5 in Savojbolagh, 2002–2003. J Iran Univ Med Sci. 2005; 12:97–105.74. Akombi BJ, Agho KE, Merom D, Hall JJ, Renzaho AM. Multilevel analysis of factors associated with wasting and underweight among children under-five years in Nigeria. Nutrients. 2017; 9:44.
Article75. Joshi HS, Gupta R, Joshi MC, Mahajan V. Determinants of nutritional status of schoolchildren, a cross sectional study in the western region of Nepal. Natl J Integr Res Med. 2011; 2:10–15.76. Emina JB, Kandala NB, Inungu J, Ye Y. Maternal education and child nutritional status in the Democratic Republic of Congo. Glob J Gynecol Obstet. 2013; 1:23–39.77. Ricci JA, Becker S. Risk factors for wasting and stunting among children in Metro Cebu, Philippines. Am J Clin Nutr. 1996; 63:966–975.
Article78. Senbanjo IO, Oshikoya KA, Odusanya OO, Njokanma OF. Prevalence of and risk factors for stunting among school children and adolescents in Abeokuta, southwest Nigeria. J Health Popul Nutr. 2011; 29:364–370.
Article79. Babar NF, Muzaffar R, Khan MA, Imdad S. Impact of socioeconomic factors on nutritional status in primary school children. J Ayub Med Coll Abbottabad. 2010; 22:15–18.80. Sommerfelt AE, Stewart MK. Children's nutritional status. Demographic and health survey comparative studies. Calverton (MD): Macro International Inc.;1994.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prevalence of underweight and wasting in Iranian children aged below 5 years: a systematic review and meta-analysis
- Prevalence of Workplace Microaggressions and Racial Discrimination: A Systematic Review and Meta-analysis
- The Prevalence of Post-Traumatic Stress Disorder in the General Population during the COVID-19 Pandemic: A Systematic Review and Single-Arm Meta-Analysis
- A Report of Health Related Anthropometric Indices in 2–5 Years Old Children of Golestan Province of Iran in 2015
- Global prevalence of enterobiasis in young children over the past 20 years: a systematic review and metaanalysis