Ann Surg Treat Res.
2019 May;96(5):216-222. 10.4174/astr.2019.96.5.216.
Negative pressure is not necessary for using fine-needle aspiration biopsy to diagnose suspected thyroid nodules: a prospective randomized study
- Affiliations
-
- 1Department of Surgery, Daejeon St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Daejeon, Korea. sun2729@naver.com
- 2Department of Pathology, Daejeon St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Daejeon, Korea.
- KMID: 2443584
- DOI: http://doi.org/10.4174/astr.2019.96.5.216
Abstract
- PURPOSE
Fine-needle aspiration biopsy (FNAB) can be used to diagnose thyroid cancer and other tumors. Although FNAB without negative pressure (FNAB−P) reduces the risk of blood contamination, FNAB with negative pressure (FNAB+P) increases the sensitivity of the biopsy results. Therefore, we performed a randomized study of FNAB with or without negative pressure to identify the better diagnostic method.
METHODS
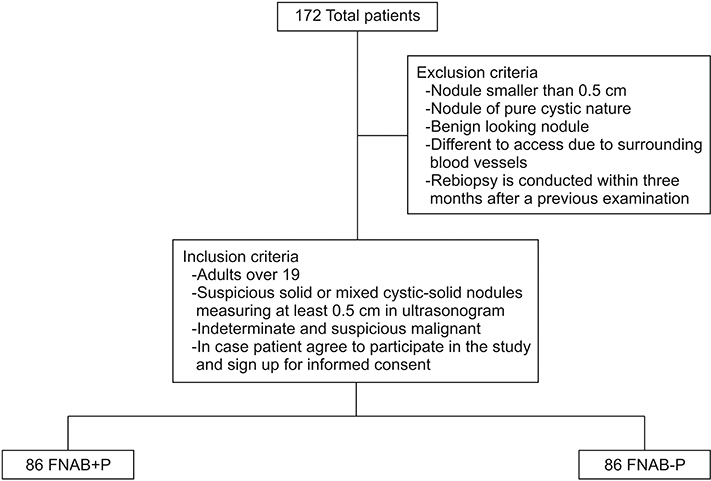
Between March 2016 and February 2017, 172 consecutive patients were enrolled to investigate >0.5 cm nodules with indeterminate or suspicious malignant features. Patients were randomly assigned to the FNAB+P group (a 50 mL syringe was used to provide negative pressure) or to the FNAB−P group (passive collection of blood in the needle's hub). The 2 methods' diagnostic adequacy and quality were evaluated using an objective scoring system. The study's protocol was registered with the World Health Organization Clinical Research Information Service (http://cris.nih.go.kr/cris, KCT0001857).
RESULTS
The patients were randomly assigned to the FNAB+P group (n = 86) or the FNAB−P group (n = 86). There were no significant intergroup differences in nodule position, size, age, consistency, calcification, BRAF mutation, or pathology. Evaluation of diagnostic adequacy parameters revealed no significant differences in background blood/clot (P = 0.728), amount of cellular material (P = 0.052), degree of cellular degeneration (P = 0.622), degree of cellular trauma (P = 0.979), or retention of appropriate architecture (P = 0.487). Furthermore, there was no significant intergroup difference in the diagnostic quality (P = 0.634).
CONCLUSION
This prospective randomized study failed to detect significant differences in the diagnostic adequacy and quality of FNAB with or without negative pressure. Therefore, the examiner may select whichever FNAB method they prefer.
MeSH Terms
Figure
Reference
-
1. Chowhan AK, Babu KV, Sachan A, Rukmangdha N, Patnayak R, Radhika K, et al. Should we apply suction during fine needle cytology of thyroid lesions? A prospective study of 200 cases. J Clin Diagn Res. 2014; 8:FC19–FC22.
Article2. Santos JE, Leiman G. Nonaspiration fine needle cytology. Application of a new technique to nodular thyroid disease. Acta Cytol. 1988; 32:353–356.3. Rizvi SA, Husain M, Khan S, Mohsin M. A comparative study of fine needle aspiration cytology versus non-aspiration technique in thyroid lesions. Surgeon. 2005; 3:273–276.
Article4. Tublin ME, Martin JA, Rollin LJ, Pealer K, Kurs-Lasky M, Ohori NP. Ultrasoundguided fine-needle aspiration versus fine-needle capillary sampling biopsy of thyroid nodules: does technique matter? J Ultrasound Med. 2007; 26:1697–1701.5. Romitelli F, Di Stasio E, Santoro C, Iozzino M, Orsini A, Cesareo R. A comparative study of fine needle aspiration and fine needle non-aspiration biopsy on suspected thyroid nodules. Endocr Pathol. 2009; 20:108–113.
Article6. Ramachandra L, Kudva R, Rao BH, Agrawal S. A comparative study of fine needle aspiration cytology (FNAC) and fine needle non-aspiration cytology (FNNAC) technique in lesions of thyroid gland. Indian J Surg. 2011; 73:287–290.
Article7. de Carvalho GA, Paz-Filho G, Cavalcanti TC, Graf H. Adequacy and diagnostic accuracy of aspiration vs. capillary fine needle thyroid biopsies. Endocr Pathol. 2009; 20:204–208.
Article8. Maurya AK, Mehta A, Mani NS, Nijhawan VS, Batra R. Comparison of aspiration vs non-aspiration techniques in fine-needle cytology of thyroid lesions. J Cytol. 2010; 27:51–54.
Article9. Malik NP, Jain M, Sharma C, Verma N, Singh A, Singh G, et al. Comparison of aspiration versus non-aspiration technique of cytodiagnosis in thyroid lesions. J Indian Acad Clin Med. 2013; 14:20–22.10. Mair S, Dunbar F, Becker PJ, Du Plessis W. Fine needle cytology--is aspiration suction necessary? A study of 100 masses in various sites. Acta Cytol. 1989; 33:809–813.11. Kamal MM, Arjune DG, Kulkarni HR. Comparative study of fine needle aspiration and fine needle capillary sampling of thyroid lesions. Acta Cytol. 2002; 46:30–34.
Article12. Tabaqchali MA, Hanson JM, Johnson SJ, Wadehra V, Lennard TW, Proud G. Thyroid aspiration cytology in Newcastle: a six year cytology/histology correlation study. Ann R Coll Surg Engl. 2000; 82:149–155.13. Tauro LF, Lobo GJ, Fernandes H, George C, Aithala PS, Shenoy D, et al. A comparative study on fine needle aspiration cytology versus fine needle capillary cytology in thyroid nodules. Oman Med J. 2012; 27:151–156.
Article14. Bajaj Y, De M, Thompson A. Fine needle aspiration cytology in diagnosis and management of thyroid disease. J Laryngol Otol. 2006; 120:467–469.
Article15. Orija IB, Pineyro M, Biscotti C, Reddy SS, Hamrahian AH. Value of repeating a nondiagnostic thyroid fine-needle aspiration biopsy. Endocr Pract. 2007; 13:735–742.
Article16. Naïm C, Karam R, Edde D. Ultrasound-guided fine-needle aspiration biopsy of the thyroid: methods to decrease the rate of unsatisfactory biopsies in the absence of an on-site pathologist. Can Assoc Radiol J. 2013; 64:220–225.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Indications for Fine Needle Aspiration in Thyroid Nodules
- Thyroid nodules with discordant results of ultrasonographic and fine-needle aspiration findings
- Thyroid Nodules with Nondiagnostic FNA Results: Role of Core Needle Biopsy
- Natural Course of Cytologically Diagnosed Benign Thyroid Nodules
- Arterial Bleeding of a Thyroid Mass After Thyroid Fine-Needle Aspiration Biopsy: A Case Report