Yonsei Med J.
2019 May;60(5):454-460. 10.3349/ymj.2019.60.5.454.
Comparison of Radiological and Histological Findings of Lung Parenchyma in Patients with Antineutrophil Cytoplasmic Antibody-Associated Vasculitis
- Affiliations
-
- 1Division of Rheumatology, Department of Internal Medicine, Catholic Kwandong University College of Medicine, International St. Mary's Hospital, Incheon, Korea.
- 2Division of Rheumatology, Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea. sangwonlee@yuhs.ac
- 3Department of Pathology, Catholic Kwandong University College of Medicine, International St. Mary's Hospital, Incheon, Korea. jsong@ish.ac.kr
- KMID: 2443249
- DOI: http://doi.org/10.3349/ymj.2019.60.5.454
Abstract
- PURPOSE
The present study investigated chest computed tomography (CT) patterns and lung histological features, as well as the consistency between radiological and histological features among patients with microscopic polyangiitis (MPA), granulomatosis with polyangiitis (GPA), and eosinophilic GPA (EGPA).
MATERIALS AND METHODS
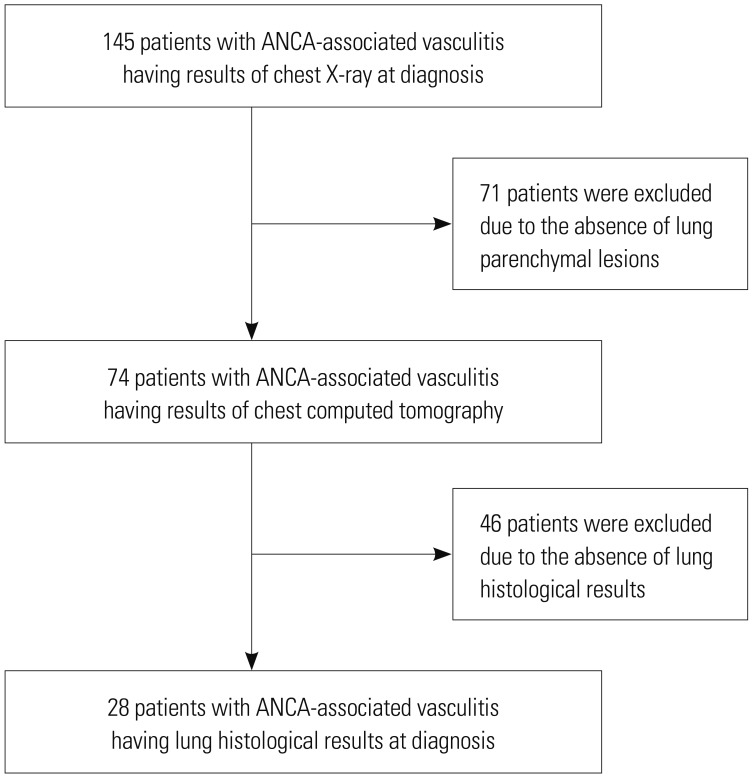
The medical records of 74 antineutrophil cytoplasmic antibody-associated vasculitis (AAV) patients with radiological lung parenchymal lesions were reviewed along with the histological results for 28 of them. Chest CT patterns were divided according 12 items mostly suggested by radiologists and histological features were divided according to necrotising granuloma, necrotising vasculitis, eosinophilic infiltration, and hemosiderin laden macrophages as defined by a pathologist.
RESULTS
The mean age was 57.1 years (22 men). The most common clinical manifestation other than lung manifestation was renal manifestation (62.2%), and the most common chest CT pattern was lung involvement of vasculitis (35.1%). In MPA patients, the major histological features were hemosiderin-laden macrophages in the alveolar space and vasculitis. In GPA patients, the major histological features were necrotizing vasculitis and necrotizing granuloma, while in EGPA patients, the major histological feature was only necrotising vasculitis. The consistency rate in GPA patients was the highest (100%), followed by that in MPA patients (66.7%) and EGPA patients (50.0%).
CONCLUSION
When lung involvement of AAV is suspected on chest CT, lung biopsy should be recommended for the proper classification of AAV, due to the discordance rate between radiological and histological findings in MPA and EGPA patients, but not GPA patients.
MeSH Terms
Figure
Reference
-
1. Jennette JC, Falk RJ, Bacon PA, Basu N, Cid MC, Ferrario F, et al. 2012 revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum. 2013; 65:1–11. PMID: 23045170.
Article2. Mukhtyar C, Lee R, Brown D, Carruthers D, Dasgupta B, Dubey S, et al. Modification and validation of the Birmingham Vasculitis Activity Score (version 3). Ann Rheum Dis. 2009; 68:1827–1832. PMID: 19054820.
Article3. Stone JH, Hoffman GS, Merkel PA, Min YI, Uhlfelder ML, Hellmann DB, et al. A disease-specific activity index for Wegener's granulomatosis: modification of the Birmingham Vasculitis Activity Score. International Network for the Study of the Systemic Vasculitides (INSSYS). Arthritis Rheum. 2001; 44:912–920. PMID: 11318006.4. Millet A, Pederzoli-Ribeil M, Guillevin L, Witko-Sarsat V, Mouthon L. Antineutrophil cytoplasmic antibody-associated vasculitides: is it time to split up the group? Ann Rheum Dis. 2013; 72:1273–1279. PMID: 23606701.
Article5. Alba MA, Flores-Suárez LF, Henderson AG, Xiao H, Hu P, Nachman PH, et al. Interstital lung disease in ANCA vasculitis. Autoimmun Rev. 2017; 16:722–729. PMID: 28479484.
Article6. Hervier B, Pagnoux C, Agard C, Haroche J, Amoura Z, Guillevin L, et al. French Vasculitis Study Group. Pulmonary fibrosis associated with ANCA-positive vasculitides. Retrospective study of 12 cases and review of the literature. Ann Rheum Dis. 2009; 68:404–407. PMID: 18957485.
Article7. Travis WD, Leslie KO, Beasley MB. Pulmonary vasculitis and pulmonary hemorrhage. In : Leslie KO, Wick MR, editors. Practical pulmonary pathology: a diagnostic approach. Philadelphia (PA): Elsevier;2018. p. 365.8. Tzelepis GE, Kokosi M, Tzioufas A, Toya SP, Boki KA, Zormpala A, et al. Prevalence and outcome of pulmonary fibrosis in microscopic polyangiitis. Eur Respir J. 2010; 36:116–121. PMID: 19926741.
Article9. Watts R, Lane S, Hanslik T, Hauser T, Hellmich B, Koldingsnes W, et al. Development and validation of a consensus methodology for the classification of the ANCA-associated vasculitides and polyarteritis nodosa for epidemiological studies. Ann Rheum Dis. 2007; 66:222–227. PMID: 16901958.
Article10. Leavitt RY, Fauci AS, Bloch DA, Michel BA, Hunder GG, Arend WP, et al. The American College of Rheumatology 1990 criteria for the classification of Wegener's granulomatosis. Arthritis Rheum. 1990; 33:1101–1107. PMID: 2202308.
Article11. Masi AT, Hunder GG, Lie JT, Michel BA, Bloch DA, Arend WP, et al. The American College of Rheumatology 1990 criteria for the classification of Churg-Strauss syndrome (allergic granulomatosis and angiitis). Arthritis Rheum. 1990; 33:1094–1100. PMID: 2202307.
Article12. Shin B, Koh WJ, Jeong BH, Yoo H, Park HY, Suh GY, et al. Serum galactomannan antigen test for the diagnosis of chronic pulmonary aspergillosis. J Infect. 2014; 68:494–499. PMID: 24462563.
Article13. Muldoon EG, Sharman A, Page I, Bishop P, Denning DW. Aspergillus nodules; another presentation of Chronic Pulmonary Aspergillosis. BMC Pulm Med. 2016; 16:123. PMID: 27538521.
Article14. Godoy MC, Viswanathan C, Marchiori E, Truong MT, Benveniste MF, Rossi S, et al. The reversed halo sign: update and differential diagnosis. Br J Radiol. 2012; 85:1226–1235. PMID: 22553298.
Article15. Shimon G, Yonit WW, Gabriel I, Naama BR, Nissim A. The “Tree-in-Bud” pattern on chest CT: radiologic and microbiologic correlation. Lung. 2015; 193:823–829. PMID: 26156310.
Article16. Egashira R, Kondo T, Hirai T, Kamochi N, Yakushiji M, Yamasaki F, et al. CT findings of thoracic manifestations of primary Sjögren syndrome: radiologic-pathologic correlation. Radiographics. 2013; 33:1933–1949. PMID: 24224588.
Article17. Watanabe M, Naniwa T, Hara M, Arakawa T, Maeda T. Pulmonary manifestations in Sjogren's syndrome: correlation analysis between chest computed tomographic findings and clinical subsets with poor prognosis in 80 patients. J Rheumatol. 2010; 37:365–373. PMID: 20008923.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- ANCA : The Marker Antibody of Vasculitis
- ANCA-Associated Vasculitis Presenting with Hypertrophic Pachymeningitis
- ANCA-Associated Vasculitic Neuropathy with Concurrent Pulmonary Tuberculosis
- A Case of Propylthiouracil-induced Lupus Erythematosus Accompanied by Antineutrophil Cytoplasmic Antibody-positive Vasculitis
- A case of Wegener's granulomatosis complicated by non-small cell lung cancer