J Korean Acad Community Health Nurs.
2019 Mar;30(1):47-56. 10.12799/jkachn.2019.30.1.47.
Effects of a Stim up Mat Walking Exercise Program on Balance, Gait Function and Joint Motion Range of the Frail Elderly
- Affiliations
-
- 1Doctorate Course, College of Nursing, Ajou University, Suwon, Korea.
- 2Professor, College of Nursing, Ajou University · Institute of Nursing Science, Suwon, Korea. msong@ajou.ac.kr
- KMID: 2442259
- DOI: http://doi.org/10.12799/jkachn.2019.30.1.47
Abstract
- PURPOSE
This study was performed to evaluate effects of a stim-up matt walking exercise program on balance and gait of the frail elderly.
METHODS
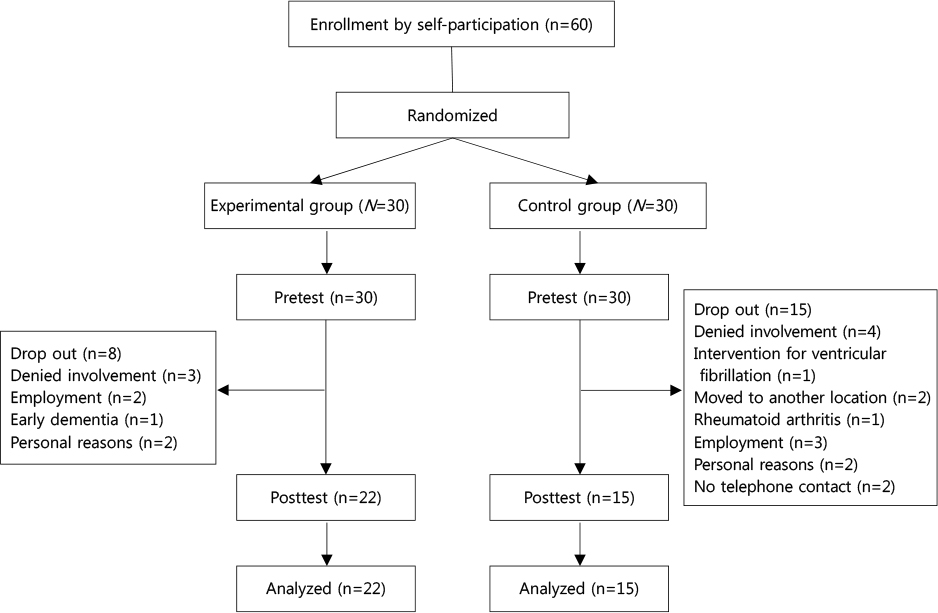
A total of 37 elderly people recruited from S city were randomly assigned to the experimental group (n=22) and control group (n=15). The stim-up matt walking exercise program was offered twice a week for 8 weeks. Data were analyzed by SPSS 21.0.
RESULTS
The dynamic balance ability Timed Up and Go test of the experimental group was significantly faster than that of the control group (t=21.72, p<.001). The static balance ability open-eye standing test (t=44.15, p<.001) and close-eye standing test (t=9.01, p=.005) also showed increase in effects of the experimental group. In the walking ability, gait cycle (t=2.48, p=.018), cadence (t=−2.21, p=.034) and gait speed (t=−2.78, p=.009), positive effects were on. However, no statistically significant differences were found in stride length and double support. At the ankle joint range left ankle plantar flexion (t=3.92, p<.001) and left ankle dorsal flexion (t=4.51, p<.001) were higher in the experimental group than in the control group, and also right ankle plantar flexion (t=2.79, p=.008) and right ankle dorsal flexion (t=2.92, p=.006) increased in the experimental group.
CONCLUSION
The significance of this study is that the stim-up matt walking exercise program for the frail elderly proves to be useful for improving balance and walking.
Keyword
Figure
Reference
-
1. Jung NS, Che GH. Cause and prevention of falling in the elderly. Journal of Korean Research Society of Physical Therapy: Physical Therapy Korea. 2001; 8(3):107–117.2. Rubenstein LZ. Falls in older people: Epidemiology, risk fac tors and strategies for prevention. Age and Ageing. 2006; 35(S2):ii37–ii41. DOI: 10.1093/ageing/afl084.3. Wipple RH, Wolfson LI, Amerman PM. The relationship of knee and ankle weakness to falls nursing home residents: An isokinetic study. Journal of the American Geriatrics Society. 1987; 35(1):13–20.4. Horak FB, Nashner LM. Central programming of postur al movements: Adaptation to altered support-surface configurations. Journal of Neurophysiology. 1986; 55(6):1369–1381. DOI: 10.1152/jn.1986.55.6.1369.5. Shumway-Cook A, Wollacott MH. Motor control: Theory and practical applications. Baltimore, Md. The Neurology Report. 1996; 20(1):64–65.6. Horak FB, Shupert CL, Mirka A. Components of postural dyscontrol in the elderly: A review. Neurobiology of Aging. 1989; 10(6):727–738.
Article7. Wolfson L, Whipple R, Judge J, Amerman P, Derby C, King M. Training balance and strength in the elderly to improve function. Journal of the American Geriatrics Society. 1993; 41(3):341–343.
Article8. Lee KJ, Lee SW, Song CH. The effect of low extremity strengthening enhanced gait mat training on unstable surface on gait parameter and low extremity strength in elderly. Journal of Special Education & Rehabilitation Science. 2011; 50(4):419–435.9. Sun WD, Song HJ, Lee YH, Kim DJ. Study on development of health care services and coordinated system for frail elderly people. Research Report. Sejong: Korea Institute for Health and Social Affairs;2004. 12. Report No: 2004-02.10. Ministry of Health and Welfare. 2013 the guideline for community community integration health promotion program: Visit health care. Guideline. Seoul: Ministry of Health and Welfare;2013. 01. Report No.: 11-1352000-000874-10.11. Horak FB. Postural orientation and equilibrium: What do we need to know about neural control of balance to prevent falls? Age and Ageing. 2006; 35(S2):ii7–ii11. DOI: 10.1093/ageing/afl077.
Article12. Podsiadlo D, Richardson S. The timed “up & go”: A test of basic functional mobility for frail elderly persons. Journal of the American Geriatrics Society. 1991; 39(2):142–148.13. Scott SH, Winter DA. Interval forces at chronic running injury sites. Medicine & Science in Sports & Exercise. 1990; 22(3):357–369.14. Yoo JS, Jeon MY, Kim CG. Effects of a fall prevention program on falls in frail elders living at home in rural communities. Journal of Korean Academy of Nursing. 2013; 43(5):613–625. DOI: 10.4040/jkan.2013.43.5.613.
Article15. O'Sullivan PB, Phyty GD, Twomey LT, Allison GT. Evaluation of specific stabilizing exercise in the treatment of chronic low back pain with radiologic diagnosis of spondylolysis or spondylolisthesis. Spine(Phila Pa 1976). 1997; 22(24):2959–2967.16. Sohn YJ. A systematic review and meta-analysis of the effects of exercise for fall prevention in the elderly [master's thesis]. [Suwon]: Ajou University;2013. 57.17. Dorey G, Glazener C, Buckley B, Cochran C, Moore K. Developing a pelvic floor muscle training regimen for use in a trial intervention. Physiotherapy. 2009; 95(3):199–209. DOI: 10.1016/j.physio.2009.03.003.
Article18. Bae YS, Um KM, Kim NS. The effect of proprioceptive exercise of ankle joint on postural alignment in woman elderly person. The Journal of Korean Society of Physical Therapy. 2009; 21(3):53–59.19. Park JM, Lee KL. Effects of functional Gait Exercise on Balance Ability and Gait Ability in Female Elderly with Chronic Arthritis. Exercise Science. 2017; 26(4):281–287.
Article20. Hess RJ, Brach JS, Piva SR, VanSwearingen JM. Walking skill can be assessed in older adults Validity of the Figure-of-8 Walk Test. Physical Therapy. 2010; 90(1):89–99. DOI: 10.2522/ptj.20080121.
Article21. Jang IS, Park EO. The prevalence and factors of falls among the community-dwelling elderly. Journal of Korean Public Health Nursing. 2013; 27(1):89–101. DOI: 10.5932/JKPHN.2013.27.1.89.
Article22. Ferrell WR, Gandevia SC, McCloskey DI. The role of joint receptors in human kinaesthesia when intramuscular receptors cannot contribute. Journal of Physiology. 1987; 386:63–71.
Article23. Magnusson M, Enbom H, Johansson R, Pyykkö I. Significance of pressor input from human feet on anterior posterior postural control: The effect of hypothermia on vibration-induced body-sway. Acta Oto-Laryngologica. 1990; 110(3-4):182–188.24. Shumway-Cook A, Wollacott MH. Motor control: Theory and practical application. 2nd ed. Boltimore: Lippincott Williams & Wilkins;2001.25. Demura S, Yamada T, Shin S. Age and sex differences in various stepping movements of the elderly. Geriatrics and Gerontology International. 2008; 8(3):180–187. DOI: 10.1111/j.1447-0594.2008.00468.x.
Article26. Kim IJ, Lee EO, Choi HJ. Perceived barriers to exercise of adults: Difference by age, gender and residence. Korean Journal of Adult Nursing. 2003; 15(2):193–204.27. Kwon MS. Effects of a fall prevention program on physical fitness and psychological functions in community dwelling elders. Journal of Korean Academy of Nursing. 2011; 41(2):165–174.
Article28. Yoo JS, Jeon MY, Kim CG. Effects of a fall prevention program on falls in frail elders living at home in rural communities. Journal of Korean Academy of Nursing. 2013; 43(5):613–625. DOI: 10.4040/jkan.2011.41.2.165.
Article29. Campbell DT, Stanley JC. Experimental and quasi-experimental designs for research. Houghton Mifflin Company;1963. p. 84.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparisons of the Exercise Types on Leg Muscle Strength, Balance and Walking ability in Elders
- Effect of Exercise Program on Physical Strength and Function in Elderly
- Variations in gait features in elderly adults during walking considering their balance
- Exercise Rehabilitation for Frail Elderly
- Responsiveness of Gait Speed to Physical Exercise Interventions in At-risk Older Adults: A Systematic Review and Meta-Analysis