Endocrinol Metab.
2019 Mar;34(1):80-92. 10.3803/EnM.2019.34.1.80.
Effects of Dipeptidyl Peptidase-4 Inhibitors on Renal Outcomes in Patients with Type 2 Diabetes: A Systematic Review and Meta-Analysis
- Affiliations
-
- 1Department of Internal Medicine, Korea University College of Medicine, Seoul, Korea. pourlife@korea.ac.kr
- 2Interdisciplinary Program in Medical Informatics, Seoul National University College of Medicine, Seoul, Korea.
- 3Division of Medical Statistics, Medical Research Collaborating Center, Seoul National University Hospital, Seoul, Korea. hahns@snu.ac.kr
- 4Department of Medicine, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2441682
- DOI: http://doi.org/10.3803/EnM.2019.34.1.80
Abstract
- BACKGROUND
To investigate the effects of dipeptidyl peptidase-4 (DPP-4) inhibitors on renal outcomes in patients with type 2 diabetes.
METHODS
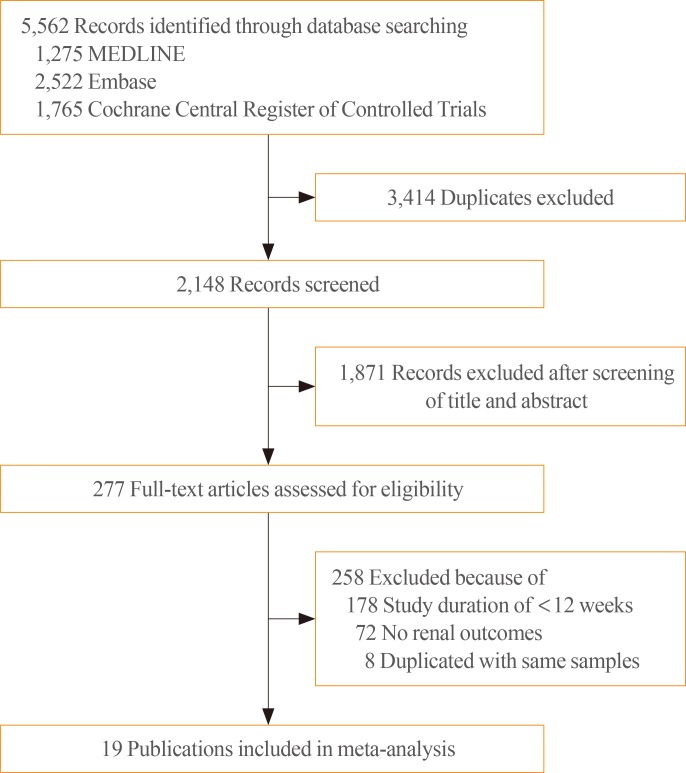
MEDLINE, Embase, and the Cochrane Central Register of Controlled Trials were searched to identify randomized controlled trials (RCTs) of DPP-4 inhibitors from inception to September 2017. We selected eligible RCTs comparing DPP-4 inhibitors with placebo or other antidiabetic agents and reporting at least one renal outcome. A meta-analysis was conducted to calculate standardized mean differences, weighted mean differences (WMDs), relative risks (RRs), and 95% confidence intervals (CIs) for each renal outcome.
RESULTS
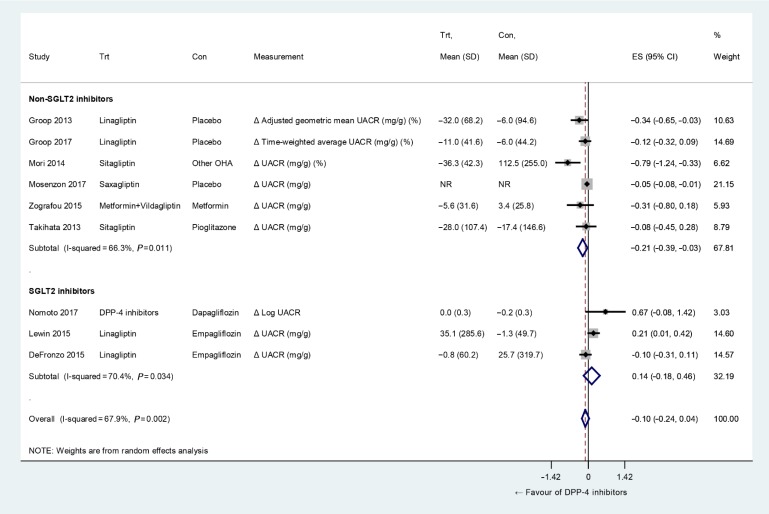
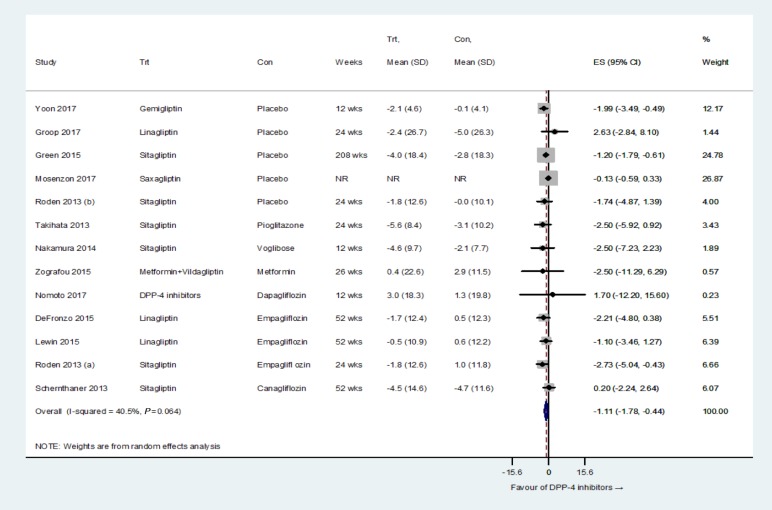
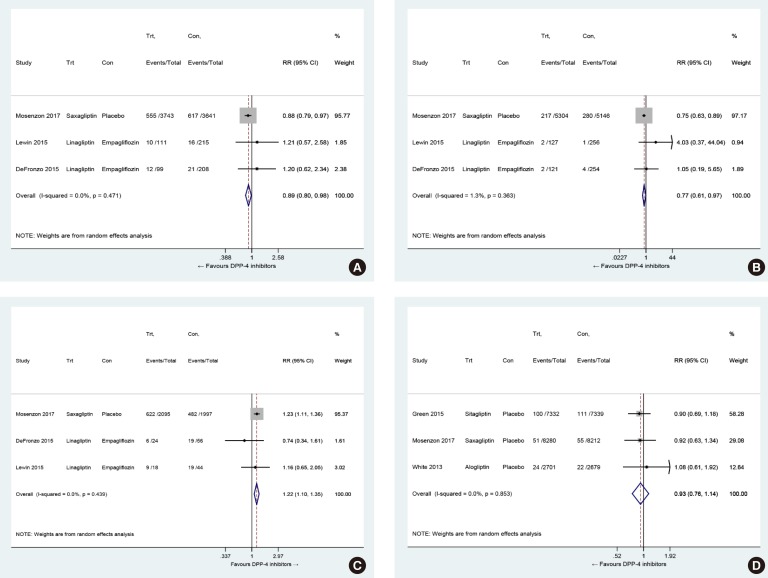
We included 23 RCTs with 19 publications involving 41,359 patients. Overall changes in urine albumin-to-creatinine ratio were comparable between DPP-4 inhibitors and controls (P=0.150). However, DPP-4 inhibitors were associated with significantly lower risk of incident microalbuminuria (RR, 0.89; 95% CI, 0.80 to 0.98; P=0.022) and macroalbuminuria (RR, 0.77; 95% CI, 0.61 to 0.97; P=0.027), as well as higher rates of regression of albuminuria (RR, 1.22; 95% CI, 1.10 to 1.35; P<0.001) compared with controls. Although DPP-4 inhibitors were associated with small but significantly lower estimated glomerular filtration rate (WMD, −1.11 mL/min/1.73 m2; 95% CI, −1.78 to −0.44; P=0.001), there was no difference in the risk of end-stage renal disease between two groups (RR, 0.93; 95% CI, 0.76 to 1.14; P=0.475).
CONCLUSION
DPP-4 inhibitors had beneficial renal effects mainly by reducing the risk of development or progression of albuminuria compared with placebo or other antidiabetic agents.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Comparative Renal Effects of Dipeptidyl Peptidase-4 Inhibitors and Sodium-Glucose Cotransporter 2 Inhibitors on Individual Outcomes in Patients with Type 2 Diabetes: A Systematic Review and Network Meta-Analysis
Jae Hyun Bae, Eun-Gee Park, Sunhee Kim, Sin Gon Kim, Seokyung Hahn, Nam Hoon Kim
Endocrinol Metab. 2021;36(2):388-400. doi: 10.3803/EnM.2020.912.
Reference
-
1. Zelnick LR, Weiss NS, Kestenbaum BR, Robinson-Cohen C, Heagerty PJ, Tuttle K, et al. Diabetes and CKD in the United States population, 2009-2014. Clin J Am Soc Nephrol. 2017; 12:1984–1990. PMID: 29054846.
Article2. Thomas MC, Cooper ME, Zimmet P. Changing epidemiology of type 2 diabetes mellitus and associated chronic kidney disease. Nat Rev Nephrol. 2016; 12:73–81. PMID: 26553517.
Article3. Thomas MC, Brownlee M, Susztak K, Sharma K, Jandeleit-Dahm KA, Zoungas S, et al. Diabetic kidney disease. Nat Rev Dis Primers. 2015; 1:15018. PMID: 27188921.
Article4. Reidy K, Kang HM, Hostetter T, Susztak K. Molecular mechanisms of diabetic kidney disease. J Clin Invest. 2014; 124:2333–2340. PMID: 24892707.
Article5. Stratton IM, Adler AI, Neil HA, Matthews DR, Manley SE, Cull CA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000; 321:405–412. PMID: 10938048.
Article6. UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998; 352:837–853. PMID: 9742976.7. Prischl FC, Wanner C. Renal outcomes of antidiabetic treatment options for type 2 diabetes: a proposed MARE definition. Kidney Int Rep. 2018; 3:1030–1038. PMID: 30197969.8. Mulvihill EE, Drucker DJ. Pharmacology, physiology, and mechanisms of action of dipeptidyl peptidase-4 inhibitors. Endocr Rev. 2014; 35:992–1019. PMID: 25216328.
Article9. Muskiet MH, Smits MM, Morsink LM, Diamant M. The gut-renal axis: do incretin-based agents confer renoprotection in diabetes? Nat Rev Nephrol. 2014; 10:88–103. PMID: 24375052.
Article10. Kang YM, Jung CH. Effects of incretin-based therapies on diabetic microvascular complications. Endocrinol Metab (Seoul). 2017; 32:316–325. PMID: 28956360.
Article11. Mosenzon O, Leibowitz G, Bhatt DL, Cahn A, Hirshberg B, Wei C, et al. Effect of saxagliptin on renal outcomes in the SAVOR-TIMI 53 trial. Diabetes Care. 2017; 40:69–76. PMID: 27797925.
Article12. Cornel JH, Bakris GL, Stevens SR, Alvarsson M, Bax WA, Chuang LM, et al. Effect of sitagliptin on kidney function and respective cardiovascular outcomes in type 2 diabetes: outcomes from TECOS. Diabetes Care. 2016; 39:2304–2310. PMID: 27742728.
Article13. Scirica BM, Bhatt DL, Braunwald E, Steg PG, Davidson J, Hirshberg B, et al. Saxagliptin and cardiovascular outcomes in patients with type 2 diabetes mellitus. N Engl J Med. 2013; 369:1317–1326. PMID: 23992601.
Article14. Green JB, Bethel MA, Armstrong PW, Buse JB, Engel SS, Garg J, et al. Effect of sitagliptin on cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2015; 373:232–242. PMID: 26052984.
Article15. Groop PH, Cooper ME, Perkovic V, Hocher B, Kanasaki K, Haneda M, et al. Linagliptin and its effects on hyperglycaemia and albuminuria in patients with type 2 diabetes and renal dysfunction: the randomized MARLINA-T2D trial. Diabetes Obes Metab. 2017; 19:1610–1619. PMID: 28636754.
Article16. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med. 2009; 151:W65–W94. PMID: 19622512.
Article17. Higgins JP, Green S. Chapter 7, Selecting studies and collecting data. Cochrane handbook for systematic reviews of interventions. Chichester: John Wiley & Sons Ltd.;2008. p. 151–185.18. Higgins JP, Green S. Chapter 8, Assessing risk of bias in included studies. Cochrane handbook for systematic reviews of interventions. Chichester: John Wiley & Sons Ltd.;2008. p. 187–242.19. Higgins JP, Green S. Chapter 9, Analysing data and undertaking meta-analyses. Cochrane handbook for systematic reviews of interventions. Chichester: John Wiley & Sons Ltd.;2008. p. 243–296.20. Cooper H, Hedges LV, Valentine JC. Chapter 12, Effect sizes for continuous data. The handbook of research synthesis and meta-analysis. 2nd ed. New York: Russell Sage Foundation;2009. p. 221–235.21. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997; 315:629–634. PMID: 9310563.
Article22. Sterne JA, Egger M. Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J Clin Epidemiol. 2001; 54:1046–1055. PMID: 11576817.23. Groop PH, Cooper ME, Perkovic V, Emser A, Woerle HJ, von Eynatten M. Linagliptin lowers albuminuria on top of recommended standard treatment in patients with type 2 diabetes and renal dysfunction. Diabetes Care. 2013; 36:3460–3468. PMID: 24026560.
Article24. Taskinen MR, Rosenstock J, Tamminen I, Kubiak R, Patel S, Dugi KA, et al. Safety and efficacy of linagliptin as add-on therapy to metformin in patients with type 2 diabetes: a randomized, double-blind, placebo-controlled study. Diabetes Obes Metab. 2011; 13:65–74. PMID: 21114605.
Article25. Del Prato S, Barnett AH, Huisman H, Neubacher D, Woerle HJ, Dugi KA. Effect of linagliptin monotherapy on glycaemic control and markers of β-cell function in patients with inadequately controlled type 2 diabetes: a randomized controlled trial. Diabetes Obes Metab. 2011; 13:258–267. PMID: 21205122.
Article26. Owens DR, Swallow R, Dugi KA, Woerle HJ. Efficacy and safety of linagliptin in persons with type 2 diabetes inadequately controlled by a combination of metformin and sulphonylurea: a 24-week randomized study. Diabet Med. 2011; 28:1352–1361. PMID: 21781152.27. Haak T, Meinicke T, Jones R, Weber S, von Eynatten M, Woerle HJ. Initial combination of linagliptin and metformin improves glycaemic control in type 2 diabetes: a randomized, double-blind, placebo-controlled study. Diabetes Obes Metab. 2012; 14:565–574. PMID: 22356132.
Article28. Mori H, Okada Y, Arao T, Tanaka Y. Sitagliptin improves albuminuria in patients with type 2 diabetes mellitus. J Diabetes Investig. 2014; 5:313–319.
Article29. Nomoto H, Miyoshi H, Sugawara H, Ono K, Yanagiya S, Oita M, et al. A randomized controlled trial comparing the effects of dapagliflozin and DPP-4 inhibitors on glucose variability and metabolic parameters in patients with type 2 diabetes mellitus on insulin. Diabetol Metab Syndr. 2017; 9:54. PMID: 28725273.
Article30. DeFronzo RA, Lewin A, Patel S, Liu D, Kaste R, Woerle HJ, et al. Combination of empagliflozin and linagliptin as second-line therapy in subjects with type 2 diabetes inadequately controlled on metformin. Diabetes Care. 2015; 38:384–393. PMID: 25583754.
Article31. Lavalle-Gonzalez FJ, Januszewicz A, Davidson J, Tong C, Qiu R, Canovatchel W, et al. Efficacy and safety of canagliflozin compared with placebo and sitagliptin in patients with type 2 diabetes on background metformin monotherapy: a randomised trial. Diabetologia. 2013; 56:2582–2592. PMID: 24026211.
Article32. Lewin A, DeFronzo RA, Patel S, Liu D, Kaste R, Woerle HJ, et al. Initial combination of empagliflozin and linagliptin in subjects with type 2 diabetes. Diabetes Care. 2015; 38:394–402. PMID: 25633662.
Article33. Schernthaner G, Gross JL, Rosenstock J, Guarisco M, Fu M, Yee J, et al. Canagliflozin compared with sitagliptin for patients with type 2 diabetes who do not have adequate glycemic control with metformin plus sulfonylurea: a 52-week randomized trial. Diabetes Care. 2013; 36:2508–2515. PMID: 23564919.34. Tonneijck L, Smits MM, Muskiet MH, Hoekstra T, Kramer MH, Danser AH, et al. Renal effects of DPP-4 inhibitor sitagliptin or GLP-1 receptor agonist liraglutide in overweight patients with type 2 diabetes: a 12-week, randomized, double-blind, placebo-controlled trial. Diabetes Care. 2016; 39:2042–2050. PMID: 27585605.
Article35. Takihata M, Nakamura A, Tajima K, Inazumi T, Komatsu Y, Tamura H, et al. Comparative study of sitagliptin with pioglitazone in Japanese type 2 diabetic patients: the COMPASS randomized controlled trial. Diabetes Obes Metab. 2013; 15:455–462. PMID: 23279373.
Article36. Nomoto H, Miyoshi H, Furumoto T, Oba K, Tsutsui H, Inoue A, et al. A randomized controlled trial comparing the effects of sitagliptin and glimepiride on endothelial function and metabolic parameters: Sapporo Athero-Incretin Study 1 (SAIS1). PLoS One. 2016; 11:e0164255. PMID: 27711199.
Article37. Zografou I, Sampanis C, Gkaliagkousi E, Iliadis F, Papageorgiou A, Doukelis P, et al. Effect of vildagliptin on hsCRP and arterial stiffness in patients with type 2 diabetes mellitus. Hormones (Athens). 2015; 14:118–125. PMID: 25402372.
Article38. Nakamura K, Oe H, Kihara H, Shimada K, Fukuda S, Watanabe K, et al. DPP-4 inhibitor and alpha-glucosidase inhibitor equally improve endothelial function in patients with type 2 diabetes: EDGE study. Cardiovasc Diabetol. 2014; 13:110. PMID: 25074318.
Article39. White WB, Cannon CP, Heller SR, Nissen SE, Bergenstal RM, Bakris GL, et al. Alogliptin after acute coronary syndrome in patients with type 2 diabetes. N Engl J Med. 2013; 369:1327–1335. PMID: 23992602.
Article40. Yoon SA, Han BG, Kim SG, Han SY, Jo YI, Jeong KH, et al. Efficacy, safety and albuminuria-reducing effect of gemigliptin in Korean type 2 diabetes patients with moderate to severe renal impairment: a 12-week, double-blind randomized study (the GUARD Study). Diabetes Obes Metab. 2017; 19:590–598. PMID: 28019072.
Article41. Roden M, Weng J, Eilbracht J, Delafont B, Kim G, Woerle HJ, et al. Empagliflozin monotherapy with sitagliptin as an active comparator in patients with type 2 diabetes: a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Diabetes Endocrinol. 2013; 1:208–219. PMID: 24622369.
Article42. Cooper ME, Perkovic V, McGill JB, Groop PH, Wanner C, Rosenstock J, et al. Kidney disease end points in a pooled analysis of individual patient-level data from a large clinical trials program of the dipeptidyl peptidase 4 inhibitor linagliptin in type 2 diabetes. Am J Kidney Dis. 2015; 66:441–449. PMID: 25960304.
Article43. Alter ML, Ott IM, von Websky K, Tsuprykov O, Sharkovska Y, Krause-Relle K, et al. DPP-4 inhibition on top of angiotensin receptor blockade offers a new therapeutic approach for diabetic nephropathy. Kidney Blood Press Res. 2012; 36:119–130. PMID: 23171828.
Article44. Kodera R, Shikata K, Takatsuka T, Oda K, Miyamoto S, Kajitani N, et al. Dipeptidyl peptidase-4 inhibitor ameliorates early renal injury through its anti-inflammatory action in a rat model of type 1 diabetes. Biochem Biophys Res Commun. 2014; 443:828–833. PMID: 24342619.
Article45. Sharkovska Y, Reichetzeder C, Alter M, Tsuprykov O, Bachmann S, Secher T, et al. Blood pressure and glucose independent renoprotective effects of dipeptidyl peptidase-4 inhibition in a mouse model of type-2 diabetic nephropathy. J Hypertens. 2014; 32:2211–2223. PMID: 25215436.
Article46. Jung GS, Jeon JH, Choe MS, Kim SW, Lee IK, Kim MK, et al. Renoprotective effect of gemigliptin, a dipeptidyl peptidase-4 inhibitor, in streptozotocin-induced type 1 diabetic mice. Diabetes Metab J. 2016; 40:211–221. PMID: 27098503.
Article47. Kanasaki K, Shi S, Kanasaki M, He J, Nagai T, Nakamura Y, et al. Linagliptin-mediated DPP-4 inhibition ameliorates kidney fibrosis in streptozotocin-induced diabetic mice by inhibiting endothelial-to-mesenchymal transition in a therapeutic regimen. Diabetes. 2014; 63:2120–2131. PMID: 24574044.
Article48. Takashima S, Fujita H, Fujishima H, Shimizu T, Sato T, Morii T, et al. Stromal cell-derived factor-1 is upregulated by dipeptidyl peptidase-4 inhibition and has protective roles in progressive diabetic nephropathy. Kidney Int. 2016; 90:783–796. PMID: 27475229.49. Lovshin JA, Rajasekeran H, Lytvyn Y, Lovblom LE, Khan S, Alemu R, et al. Dipeptidyl peptidase 4 inhibition stimulates distal tubular natriuresis and increases in circulating SDF-1α(1-67) in patients with type 2 diabetes. Diabetes Care. 2017; 40:1073–1081. PMID: 28550195.
Article50. Cherney DZ, Perkins BA, Soleymanlou N, Maione M, Lai V, Lee A, et al. Renal hemodynamic effect of sodium-glucose cotransporter 2 inhibition in patients with type 1 diabetes mellitus. Circulation. 2014; 129:587–597. PMID: 24334175.
Article51. Rieg T, Gerasimova M, Murray F, Masuda T, Tang T, Rose M, et al. Natriuretic effect by exendin-4, but not the DPP-4 inhibitor alogliptin, is mediated via the GLP-1 receptor and preserved in obese type 2 diabetic mice. Am J Physiol Renal Physiol. 2012; 303:F963–F971. PMID: 22832924.
Article52. Yang L, Yuan J, Zhou Z. Emerging roles of dipeptidyl peptidase 4 inhibitors: anti-inflammatory and immunomodulatory effect and its application in diabetes mellitus. Can J Diabetes. 2014; 38:473–479. PMID: 25034244.
Article53. Shinjo T, Nakatsu Y, Iwashita M, Sano T, Sakoda H, Ishihara H, et al. DPP-IV inhibitor anagliptin exerts anti-inflammatory effects on macrophages, adipocytes, and mouse livers by suppressing NF-κB activation. Am J Physiol Endocrinol Metab. 2015; 309:E214–E223. PMID: 26015438.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Dipeptidyl Peptidase-4 Inhibitors on Cardiovascular Outcome
- Comparative Renal Effects of Dipeptidyl Peptidase-4 Inhibitors and Sodium-Glucose Cotransporter 2 Inhibitors on Individual Outcomes in Patients with Type 2 Diabetes: A Systematic Review and Network Meta-Analysis
- Emerging Safety Issues of Dipeptidyl Peptidase-4 Inhibitors and Sodium Glucose Cotransporter 2 Inhibitors: How to Interpret and Apply in Clinical Practice
- Novel Therapies for Type 2 Diabetes Mellitus
- Dipeptidyl Peptidase-4 Inhibitors and COVID-19-Related Deaths among Patients with Type 2 Diabetes Mellitus: A Meta-Analysis of Observational Studies