Neonatal Med.
2019 Feb;26(1):67-71. 10.5385/nm.2019.26.1.67.
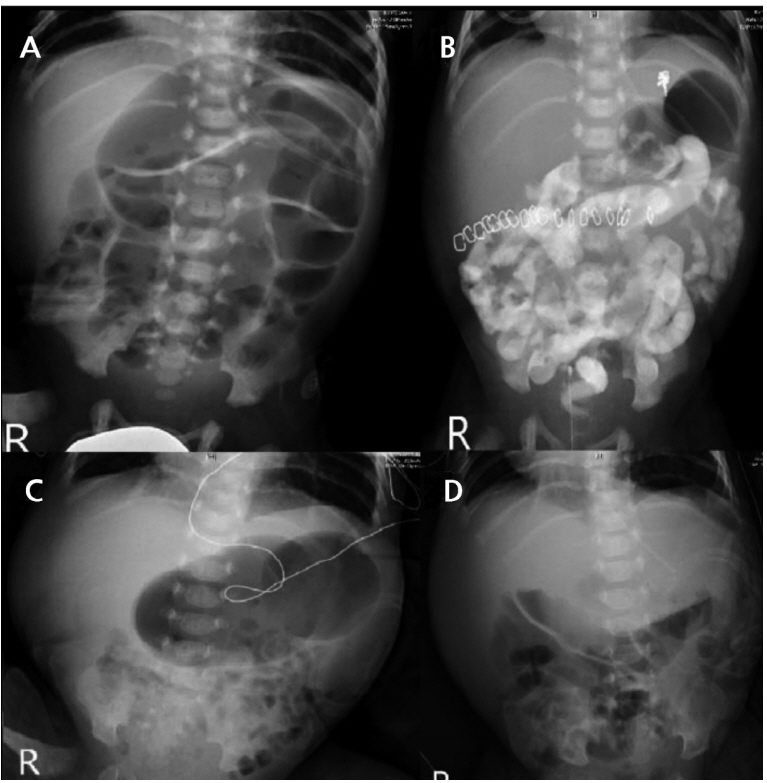
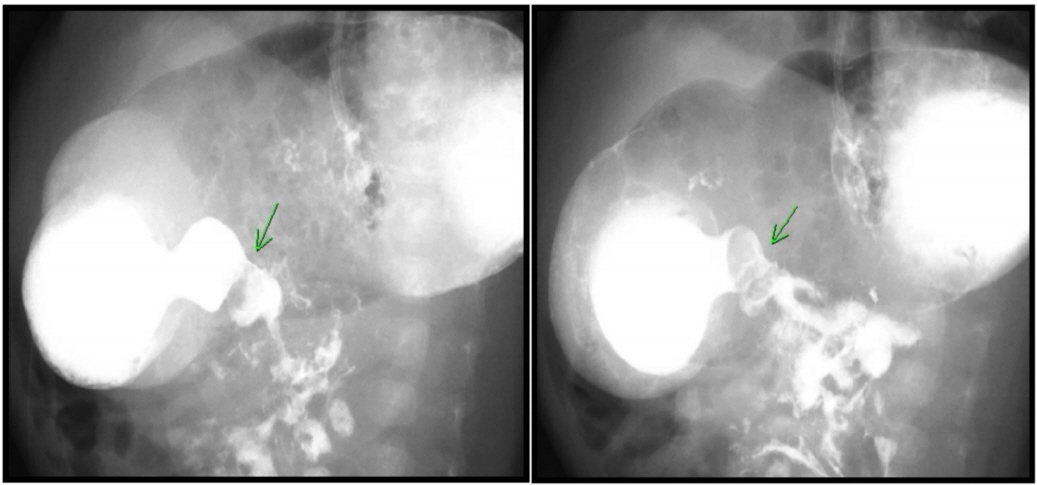
Successful Treatment of Neonatal Pylorospasm with Intravenous Atropine
- Affiliations
-
- 1Division of Neonatology, Severance Children's Hospital, Yonsei University College of Medicine, Seoul, Korea. hseun@yuhs.ac
- 2Department of Pediatrics, Yonsei University College of Medicine, Seoul, Korea.
- 3Department of Pediatrics, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2440703
- DOI: http://doi.org/10.5385/nm.2019.26.1.67
Abstract
- Pylorospasm is a cause of delayed gastric emptying in young infants. As in patients with hypertrophic pyloric stenosis, most pylorospasm patients present with projectile vomiting. However, unlike that in case of hypertrophic pyloric stenosis, no persistent pyloric stenotic lesions are present. As such, follow-up using serial gastrointestinal fluoroscopy or ultrasonography can be helpful in diagnosing patients with clinical signs of gastroparesis. Most cases can be treated conservatively, but some patients require pharmacologic treatment. Antispasmodics have been proposed as a treatment for pylorospasm, but their use in neonates and infants has rarely been reported. Herein, we present a case of pylorospasm diagnosed in the neonatal period and successfully treated with intravenous atropine.
MeSH Terms
Figure
Reference
-
1. Gilet AG, Dunkin J, Cohen HL. Pylorospasm (simulating hypertrophic pyloric stenosis) with secondary gastroesophageal reflux. Ultrasound Q. 2008; 24:93–6.2. Cohen HL, Zinn HL, Haller JO, Homel PJ, Stoane JM. Ultrasonography of pylorospasm: findings may simulate hypertrophic pyloric stenosis. J Ultrasound Med. 1998; 17:705–11.3. Cohen HL, Blumer SL, Zucconi WB. The sonographic doubletrack sign: not pathognomonic for hypertrophic pyloric stenosis; can be seen in pylorospasm. J Ultrasound Med. 2004; 23:641–6.4. Islam S. Gastroparesis in children. Curr Opin Pediatr. 2015; 27:377–82.5. Tillman EM, Smetana KS, Bantu L, Buckley MG. Pharmacologic treatment for pediatric gastroparesis: a review of the literature. J Pediatr Pharmacol Ther. 2016; 21:120–32.6. Heidelbaugh JJ. Gastrointestinal diseases: a multidisciplinary approach. Philadelphia: Elsevier Health Science;2015. p. 309.7. Hilas O. Management of gastroparesis. US Pharm. 2011; 36:HS15–8.8. Lauriti G, Cascini V, Chiesa PL, Pierro A, Zani A. Atropine treatment for hypertrophic pyloric stenosis: a systematic review and meta-analysis. Eur J Pediatr Surg. 2018; 28:393–9.9. Wu SF, Lin HY, Huang FK, Chen AC, Su BH, Li CI, et al. Efficacy of medical treatment for infantile hypertrophic pyloric stenosis: a meta-analysis. Pediatr Neonatol. 2016; 57:515–21.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intravenous Atropine Sulfate Therapy for Infantile Hypertrophic Pyloric Stenosis
- Infantile Hypertrophic Pyloric Stenosis Treated with Intravenous Atropine Sulfate
- Usefulness of serum lactate as a predictor of successful discontinuation of continuous atropine infusion in patients with severe acute organophosphate poisoning
- Two Cases of Successful Treatment with Atropine Sulfate in Persistent Vomiting beyond Pyloromyotomy of Infantile Hypertrophic Pyrolic Stenosis
- Effect of Intraventricular Atropine on the Heart Rate of the Rabbit