J Korean Orthop Assoc.
2017 Apr;52(2):125-137. 10.4055/jkoa.2017.52.2.125.
Distal Radioulnar Joint Arthritis
- Affiliations
-
- 1Department of Orthopedic Surgery, Chungnam National University School of Medicine, Regional Rheumatoid and Degenerative Arthritis Center, Chungnam National University Hospital, Daejeon, Korea. hyunsd@cnu.ac.kr
- KMID: 2438977
- DOI: http://doi.org/10.4055/jkoa.2017.52.2.125
Abstract
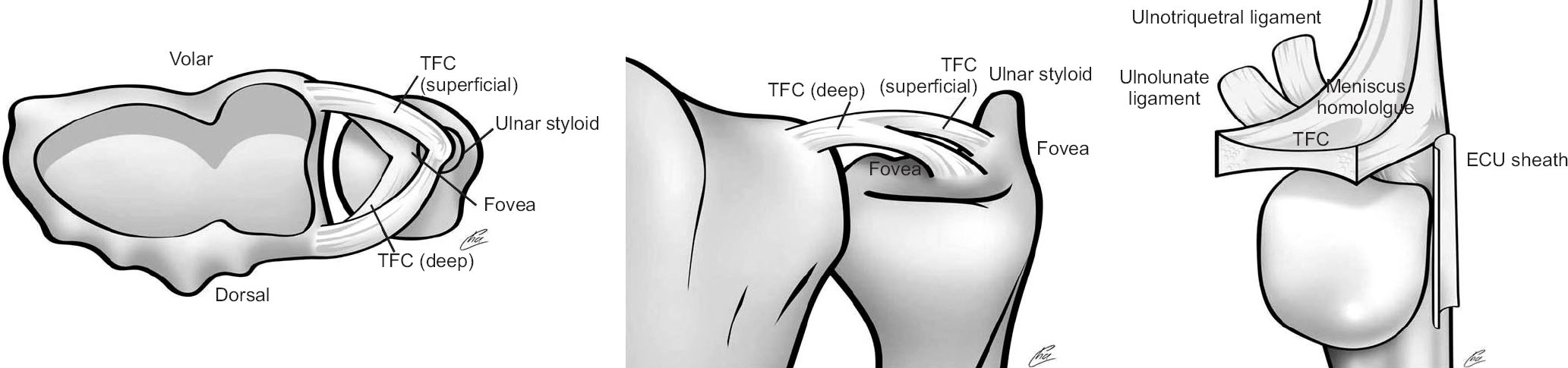
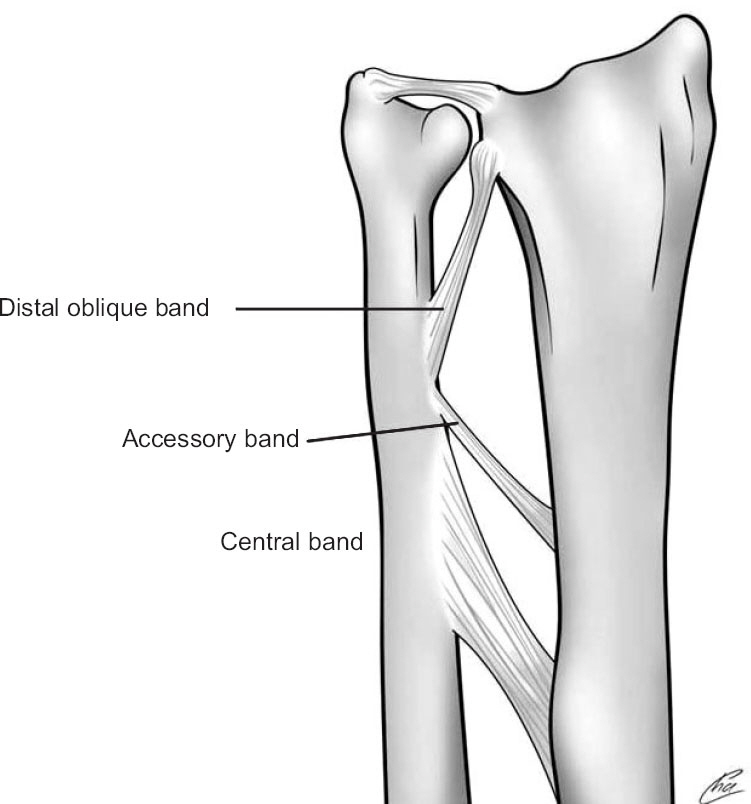
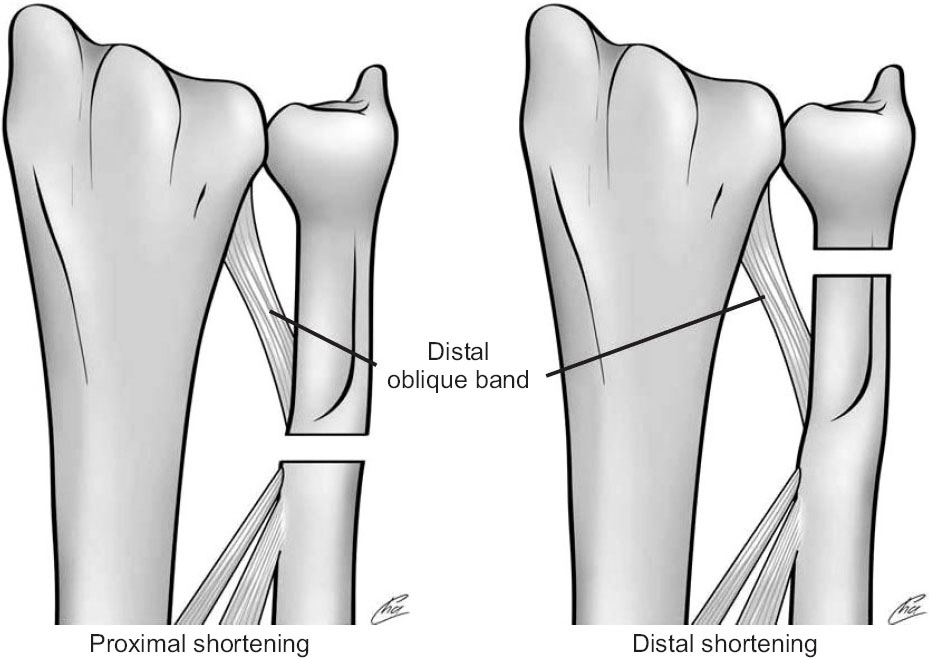
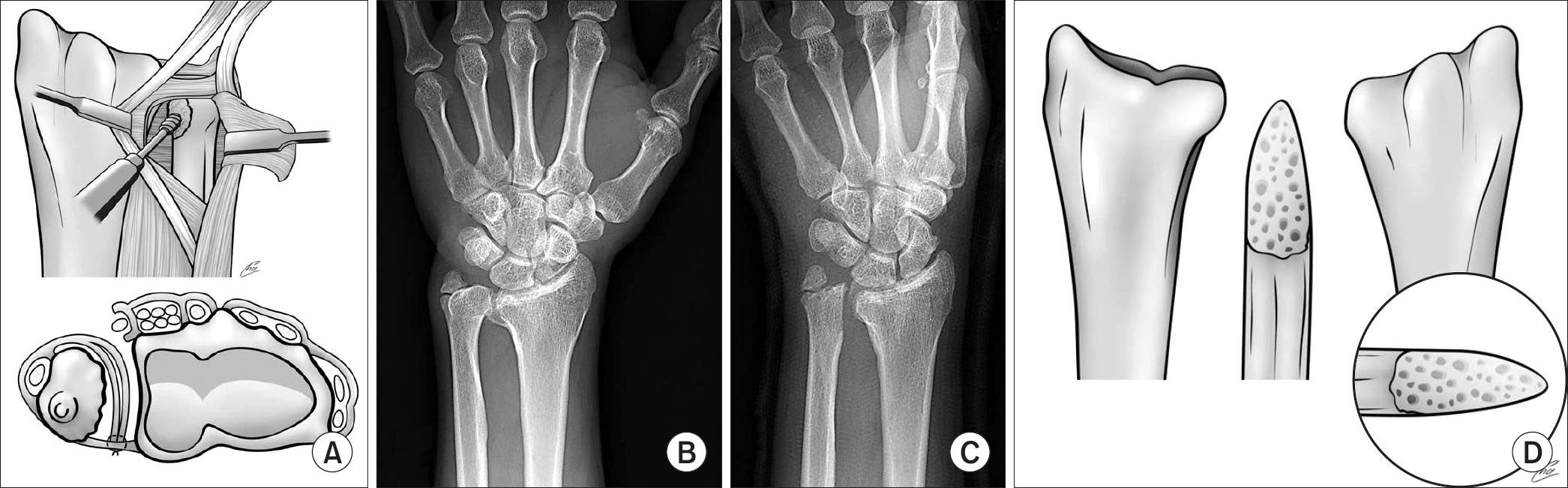
- The distal radioulnar joint (DRUJ) is a complex structure that enables sufficient, painless forearm rotation and provides weight-bearing capabilities of the upper extremity. Arthritis of DRUJ is multifactorial; the most common causes are trauma, congenital anomalies, as well as degenerative and inflammatory diseases. Congenital etiologies, as well as degenerative and inflammatory causes of arthritis are more common in women. Conventionally, initial management of symptomatic DRUJ arthritis is nonsurgical; surgery is generally reserved for patients with refractory pain. Moreover, advanced arthritis arising from trauma can be prevented by early interventions in the form of corrective osteotomy for malunited distal radius and distal ulna fractures, repair/reconstruction of the triangular fibrocartilage complex, and ulnar shortening osteotomy. Although the outcomes are typically positive following excision of the distal ulna in definitive arthritis, postoperative complications, such as instability and impingement of the residual distal ulna stump, can be serious. Procedures managing unstable residual ulna include soft tissue stabilization techniques and DRUJ implant arthroplasty.
MeSH Terms
Figure
Cited by 1 articles
-
Ulnar impaction syndrome: how to diagnose and treat?
Hyun Sik Seok, Jong Woong Park, Jong Woo Kang
Arch Hand Microsurg. 2022;27(2):105-118. doi: 10.12790/ahm.21.0149.
Reference
-
1. Dingman PV. Resection of the distal end of the ulna (Darrach operation); an end result study of twenty four cases. J Bone Joint Surg Am. 1952; 34:893–900.2. Leslie BM, Carlson G, Ruby LK. Results of extensor carpi ulnaris tenodesis in the rheumatoid wrist undergoing a distal ulnar excision. J Hand Surg Am. 1990; 15:547–51.
Article3. Ruby LK, Ferenz CC, Dell PC. The pronator quadratus interposition transfer: an adjunct to resection arthroplasty of the distal radioulnar joint. J Hand Surg Am. 1996; 21:60–5.
Article4. Sotereanos DG, Göbel F, Vardakas DG, Sarris I. An allograft salvage technique for failure of the Darrach procedure: a report of four cases. J Hand Surg Br. 2002; 27:317–21.
Article5. af Ekenstam F. Anatomy of the distal radioulnar joint. Clin Orthop Relat Res. 1992; 275:14–8.6. Stuart PR, Berger RA, Linscheid RL, An KN. The dorsopal-mar stability of the distal radioulnar joint. J Hand Surg Am. 2000; 25:689–99.
Article7. Nygaard M, Nielsen NS, Bojsen-Møller F. A biomechanical evaluation of the relative load change in the joints of the wrist with ulnar shortening: a ‘handbag’ model. J Hand Surg Eur Vol. 2009; 34:724–9.
Article8. Nishiwaki M, Nakamura T, Nagura T, Toyama Y, Ikegami H. Ulnar-shortening effect on distal radioulnar joint pressure: a biomechanical study. J Hand Surg Am. 2008; 33:198–205.
Article9. Nishiwaki M, Nakamura T, Nakao Y, Nagura T, Toyama Y. Ulnar shortening effect on distal radioulnar joint stability: a biomechanical study. J Hand Surg Am. 2005; 30:719–26.
Article10. Jupiter JB, Ring D. A comparison of early and late reconstruction of malunited fractures of the distal end of the radius. J Bone Joint Surg Am. 1996; 78:739–48.
Article11. Murray PM. Current concepts in the treatment of rheumatoid arthritis of the distal radioulnar joint. Hand Clin. 2011; 27:49–55.
Article12. Szabo RM. Distal radioulnar joint instability. J Bone Joint Surg Am. 2006; 88:884–94.
Article13. Lester B, Halbrecht J, Levy IM, Gaudinez R. "Press test" for office diagnosis of triangular fibrocartilage complex tears of the wrist. Ann Plast Surg. 1995; 35:41–5.
Article14. Tsai PC, Paksima N. The distal radioulnar joint. Bull NYU Hosp Jt Dis. 2009; 67:90–6.15. Tolat AR, Sanderson PL, De Smet L, Stanley JK. The gymnast's wrist: acquired positive ulnar variance following chronic epiphyseal injury. J Hand Surg Br. 1992; 17:678–81.
Article16. Mino DE, Palmer AK, Levinsohn EM. Radiography and computerized tomography in the diagnosis of incongruity of the distal radio-ulnar joint. A prospective study. J Bone Joint Surg Am. 1985; 67:247–52.
Article17. Wechsler RJ, Wehbe MA, Rifkin MD, Edeiken J, Branch HM. Computed tomography diagnosis of distal radioulnar subluxation. Skeletal Radiol. 1987; 16:1–5.
Article18. Lo IK, MacDermid JC, Bennett JD, Bogoch E, King GJ. The radioulnar ratio: a new method of quantifying distal radioulnar joint subluxation. J Hand Surg Am. 2001; 26:236–43.
Article19. Amrami KK, Moran SL, Berger RA, Ehman EC, Felmlee JP. Imaging the distal radioulnar joint. Hand Clin. 2010; 26:467–75.
Article20. Darrach W. Habitual forward dislocation of the neck of the ulna. Ann Surg. 1913; 57:928–30.21. Tulipan DJ, Eaton RG, Eberhart RE. The Darrach procedure defended: technique redefined and long-term follow-up. J Hand Surg Am. 1991; 16:438–44.
Article22. Bowers WH. Distal radioulnar joint arthroplasty: the hemire-section-interposition technique. J Hand Surg Am. 1985; 10:169–78.
Article23. Watson HK, Gabuzda GM. Matched distal ulna resection for posttraumatic disorders of the distal radioulnar joint. J Hand Surg Am. 1992; 17:724–30.24. Fujita S, Masada K, Takeuchi E, Yasuda M, Komatsubara Y, Hashimoto H. Modified Sauvé-Kapandji procedure for disorders of the distal radioulnar joint in patients with rheumatoid arthritis. J Bone Joint Surg Am. 2005; 87:134–9.
Article25. Gordon KD, Dunning CE, Johnson JA, King GJ. Kinematics of ulnar head arthroplasty. J Hand Surg Br. 2003; 28:551–8.
Article26. Zimmermann R, Gschwentner M, Arora R, Harpf C, Gabl M, Pechlaner S. Treatment of distal radioulnar joint disorders with a modified Sauvé-Kapandji procedure: long-term outcome with special attention to the DASH Questionnaire. Arch Orthop Trauma Surg. 2003; 123:293–8.
Article27. Minami A, Iwasaki N, Ishikawa J, Suenaga N, Yasuda K, Kato H. Treatments of osteoarthritis of the distal radioulnar joint: long-term results of three procedures. Hand Surg. 2005; 10:243–8.
Article28. O'Donovan TM, Ruby LK. The distal radioulnar joint in rheumatoid arthritis. Hand Clin. 1989; 5:249–56.29. Webber JB, Maser SA. Stabilization of the distal ulna. Hand Clin. 1991; 7:345–53.
Article30. Spinner M, Kaplan EB. Extensor carpi ulnaris. Its relationship to the stability of the distal radio-ulnar joint. Clin Orthop Relat Res. 1970; 68:124–9.31. Breen TF, Jupiter JB. Extensor carpi ulnaris and flexor carpi ulnaris tenodesis of the unstable distal ulna. J Hand Surg Am. 1989; 4:612–7.
Article32. Tsai TM, Shimizu H, Adkins P.A modified extensor carpi ulnaris tenodesis with the Darrach procedure. J Hand Surg Am. 1993; 18:697–702.
Article33. Tsai TM, Stilwell JH. Repair of chronic subluxation of the distal radioulnar joint (ulnar dorsal) using flexor carpi ulnaris tendon. J Hand Surg Br. 1984; 9:289–94.
Article34. Hunter JM, Kirkpatrick WH. Dacron stabilization of the distal ulna. Hand Clin. 1991; 7:365–71.
Article35. Watson HK, Brown RE. Ulnar impingement syndrome after Darrach procedure: treatment by advancement lengthening osteotomy of the ulna. J Hand Surg Am. 1989; 14:302–6.36. Johnson RK. Stabilization of the distal ulna by transfer of the pronator quadratus origin. Clin Orthop Relat Res. 1992; 275:130–2.
Article37. Blatt G, Ashworth CR.Volar capsule transfer for stabilisation following resection of the distal end of the ulna. Orthop Trans. 1979; 3:13–14.38. Kleinman WB, Greenberg JA.Salvage of the failed Darrach procedure. J Hand Surg Am. 1995; 20:951–8.
Article39. Wolfe SW, Mih AD, Hotchkiss RN, Culp RW, Keifhaber TR, Nagle DJ. Wide excision of the distal ulna: a multicenter case study. J Hand Surg Am. 1998; 23:222–8.
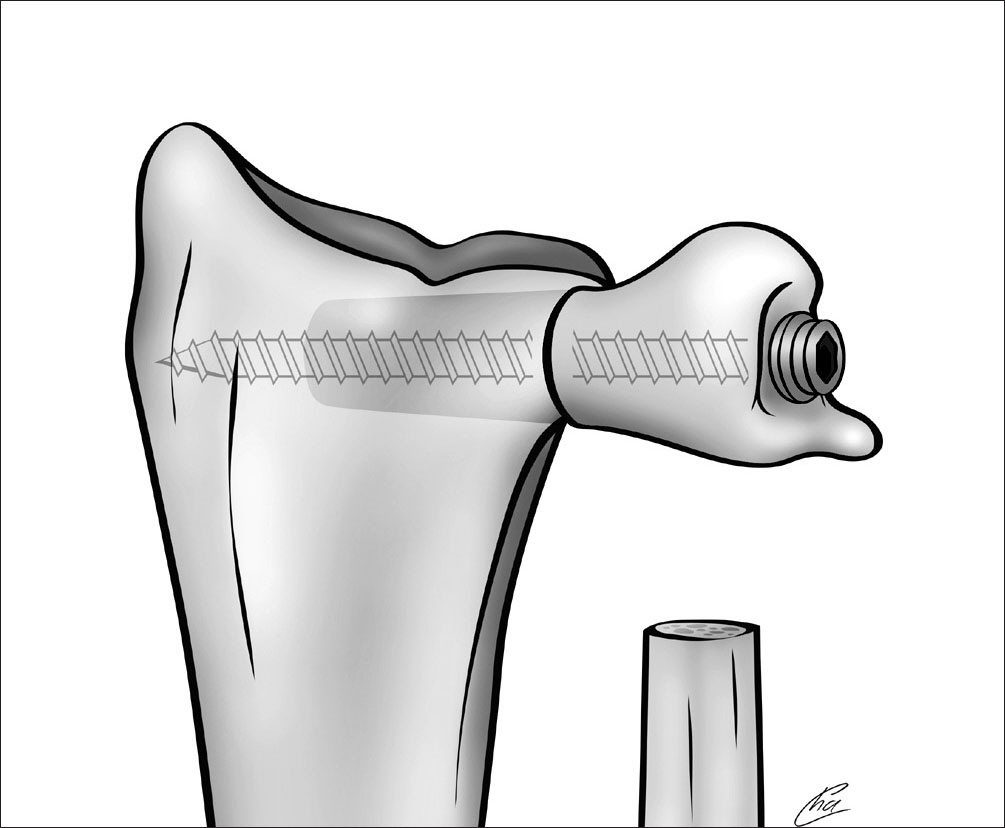
Article40. Swanson AB.Implant arthroplasty for disabilities of the distal radioulnar joint. Use of a silicone rubber capping implant following resection of the ulnar head. Orthop Clin North Am. 1973; 4:373–82.
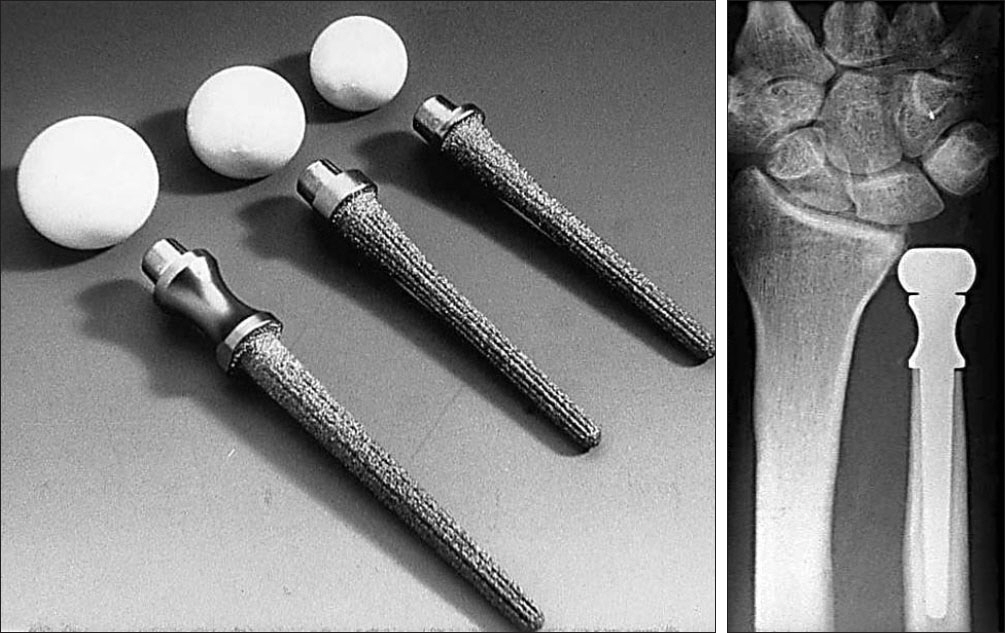
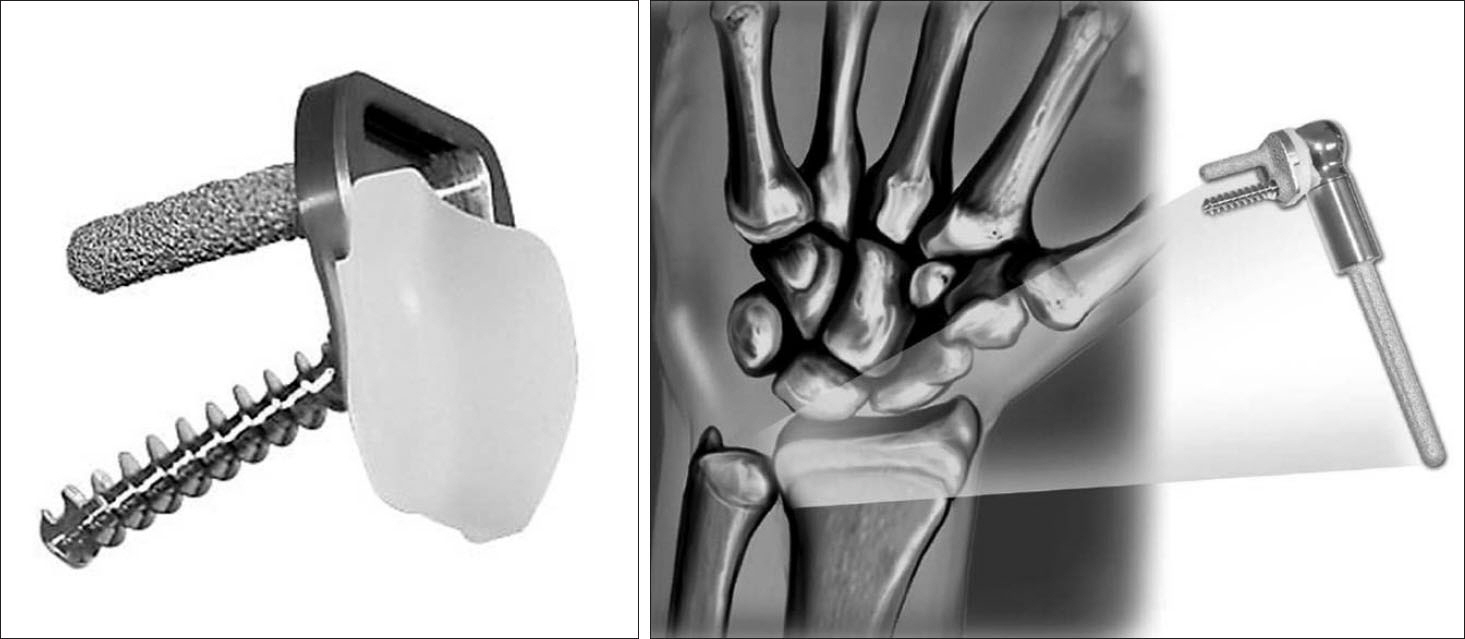
Article41. Garcia-Elias M.; Eclypse. Partial ulnar head replacement for the isolated distal radio-ulnar joint arthrosis. Tech Hand Up Extrem Surg. 2007; 11:121–8.42. van Schoonhoven J, Fernandez DL, Bowers WH, Herbert TJ.Salvage of failed resection arthroplasties of the distal radioulnar joint using a new ulnar head prosthesis. J Hand Surg Am. 2000; 25:438–46.
Article43. Burke CS, Gupta A, Buecker P.Distal ulna giant cell tumor resection with reconstruction using distal ulna prosthesis and brachioradialis wrap soft tissue stabilization. Hand (N Y). 2009; 4:410–4.
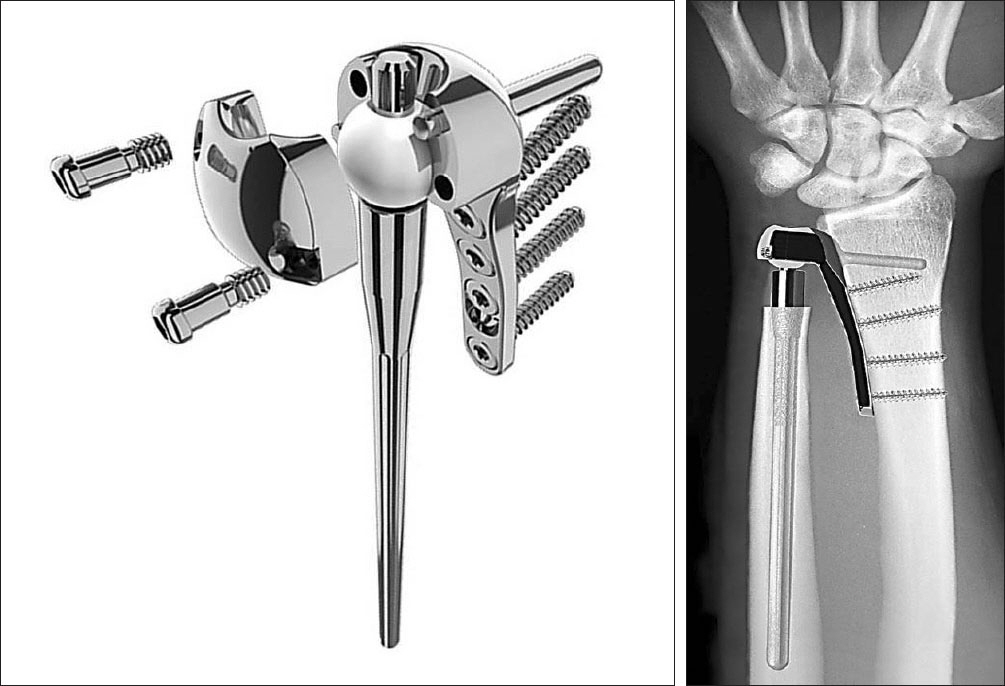
Article44. Scheker LR, Babb BA, Killion PE.Distal ulnar prosthetic replacement. Orthop Clin North Am. 2001; 32:365–76.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of Old Distal Radioulnar Dislocation: A Preliminary Report
- Treatment of Dislocation of distal Radio - ulnar Joint: Comparison of Long - term follow - up Results between the Reconstruction and Darrach Operation Group
- The significance of distal radioulnar joint injury in distal radius fracture
- Delayed Rupture of Flexor Tendons due to a Malunion of Distal Radius Fracture
- Transscaphoidal Dorsal Perilunar Dislocation Associated with Dislocation of Distal Radioulnar Joint: A Case Report