J Periodontal Implant Sci.
2012 Dec;42(6):196-203.
Subepithelial connective tissue graft with and without the use of plasma rich in growth factors for treating root exposure
- Affiliations
-
- 1Department of Periodontics, Shahid Beheshti University of Medical Sciences Faculty of Dentistry, Tehran, Iran.
- 2Department of Periodontics, Dental and Periodontal Research Center, Tabriz University of Medical Sciences Faculty of Dentistry, Tabriz, Iran. faramarzie@hotmail.com
- 3Department of Orthodontics, Tabriz University of Medical Sciences Faculty of Dentistry, Tabriz, Iran.
- 4Department of Periodontics, Tabriz University of Medical Sciences Faculty of Dentistry, Tabriz, Iran.
- 5Department of Periodontics, Urmia University of Medical Sciences Faculty of Dentisty, Urmia, Iran.
Abstract
- PURPOSE
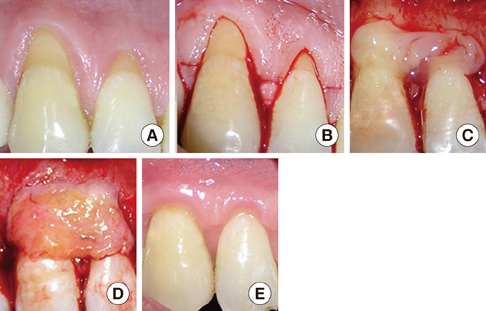
The aim of this study was to evaluate the clinical efficiency of the subepithelial connective tissue graft (SCTG) with and without plasma rich in growth factor (PRGF) in the treatment of gingival recessions.
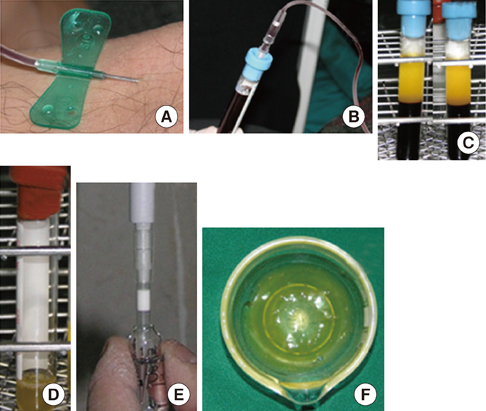
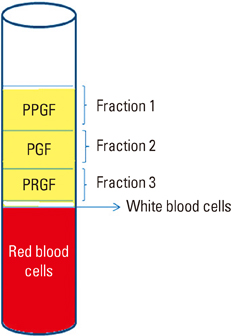
METHODS
Twenty bilateral buccal gingival Miller's Class I and II recessions were selected. Ten of the recessions were treated with SCTG and PRGF (test group). The rest ten of the recessions were treated with SCTG (control group). The clinical parameters including recession depth (RD), percentage of root coverage (RC), mucogingival junction (MGJ) position, clinical attachment level (CAL), and probing depth (PD) were measured at the baseline, and 1 and 3 months later. The data were analyzed using the Wilcoxon signed rank and Mann-Whitney U tests.
RESULTS
After 3 months, both groups showed a significant improvement in all of the mentioned criteria except PD. Although the amount of improvement was better in the SCTG+PRGF group than the SCTG only group, this difference was not statistically significant. The mean RC was 70.85+/-12.57 in the test group and 75.83+/-24.68 in the control group.
CONCLUSIONS
Both SCTG+PRGF and SCTG only result in favorable clinical outcomes, but the added benefit of PRGF is not evident.
Keyword
MeSH Terms
Figure
Reference
-
1. Keceli HG, Sengun D, Berberoglu A, Karabulut E. Use of platelet gel with connective tissue grafts for root coverage: a randomized-controlled trial. J Clin Periodontol. 2008. 35:255–262.
Article2. Kassab MM, Cohen RE. The etiology and prevalence of gingival recession. J Am Dent Assoc. 2003. 134:220–225.
Article3. Lindhe J, karring T, Lang NP. Clinical periodontology and implant dentistry. 2003. 4rd ed. Oxford: Blackwell.4. Rees JS, Addy M. A cross-sectional study of dentine hypersensitivity. J Clin Periodontol. 2002. 29:997–1003.
Article5. Oliver RC, Brown LJ, Loe H. Periodontal diseases in the United States population. J Periodontol. 1998. 69:269–278.
Article6. Grupe HE, Warren RF. Repair of gingival defects by a sliding flap operation. J Periodontol. 1956. 27:92–95.
Article7. Harvey PM. Management of advanced periodontitis. I. Preliminary report of a method of surgical reconstruction. N Z Dent J. 1965. 61:180–187.8. Sullivan HC, Atkins JH. Free autogenous gingival grafts. 3. Utilization of grafts in the treatment of gingival recession. Periodontics. 1968. 6:152–160.9. Miller PD Jr. Root coverage using a free soft tissue autograft following citric acid application. Part 1: Technique. Int J Periodontics Restorative Dent. 1982. 2:65–70.10. Langer B, Langer L. Subepithelial connective tissue graft technique for root coverage. J Periodontol. 1985. 56:715–720.
Article11. Wennström JL, Zucchelli G. Increased gingival dimensions. A significant factor for successful outcome of root coverage procedures? A 2-year prospective clinical study. J Clin Periodontol. 1996. 23:770–777.
Article12. Paolantonio M. Treatment of gingival recessions by combined periodontal regenerative technique, guided tissue regeneration, and subpedicle connective tissue graft. A comparative clinical study. J Periodontol. 2002. 73:53–62.
Article13. Tozum TF, Keceli HG, Guncu GN, Hatipoglu H, Sengun D. Treatment of gingival recession: comparison of two techniques of subepithelial connective tissue graft. J Periodontol. 2005. 76:1842–1848.
Article14. Lekovic V, Camargo PM, Weinlaender M, Vasilic N, Kenney EB. Comparison of platelet-rich plasma, bovine porous bone mineral, and guided tissue regeneration versus platelet-rich plasma and bovine porous bone mineral in the treatment of intrabony defects: a reentry study. J Periodontol. 2002. 73:198–205.
Article15. Maloney JP, Silliman CC, Ambruso DR, Wang J, Tuder RM, Voelkel NF. In vitro release of vascular endothelial growth factor during platelet aggregation. Am J Physiol. 1998. 275(3 Pt 2):H1054–H1061.
Article16. Anitua E, Andia I. PRGF (platelet rich in growth factors). Dent Dialog. 2004. 3:31–39.17. Wartiovaara U, Salven P, Mikkola H, Lassila R, Kaukonen J, Joukov V, et al. Peripheral blood platelets express VEGF-C and VEGF which are released during platelet activation. Thromb Haemost. 1998. 80:171–175.
Article18. Marx RE, Carlson ER, Eichstaedt RM, Schimmele SR, Strauss JE, Georgeff KR. Platelet-rich plasma: Growth factor enhancement for bone grafts. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998. 85:638–646.19. Anitua E. Plasma rich in growth factors: preliminary results of use in the preparation of future sites for implants. Int J Oral Maxillofac Implants. 1999. 14:529–535.20. Kassolis JD, Rosen PS, Reynolds MA. Alveolar ridge and sinus augmentation utilizing platelet-rich plasma in combination with freeze-dried bone allograft: case series. J Periodontol. 2000. 71:1654–1661.
Article21. Zechner W, Tangl S, Tepper G, Furst G, Bernhart T, Haas R, et al. Influence of platelet-rich plasma on osseous healing of dental implants: a histologic and histomorphometric study in minipigs. Int J Oral Maxillofac Implants. 2003. 18:15–22.22. Huang LH, Neiva RE, Soehren SE, Giannobile WV, Wang HL. The effect of platelet-rich plasma on the coronally advanced flap root coverage procedure: a pilot human trial. J Periodontol. 2005. 76:1768–1777.
Article23. Lafzi A, Chitsazi MT, Farahani RM, Faramarzi M. Comparative clinical study of coronally advanced flap with and without use of plasma rich in growth factors in the treatment of gingival recession. Am J Dent. 2011. 24:143–147.24. Miller PD Jr. A classification of marginal tissue recession. Int J Periodontics Restorative Dent. 1985. 5:8–13.25. Tarnow DP. Semilunar coronally repositioned flap. J Clin Periodontol. 1986. 13:182–185.
Article26. Löe H. The Gingival Index, the Plaque Index and the Retention Index Systems. J Periodontol. 1967. 38:Suppl:610–Suppl:616.
Article27. Silness J, Loe H. Periodontal disease in pregnancy. II. Correlation between oral hygiene and periodontal condtion. Acta Odontol Scand. 1964. 22:121–135.
Article28. Anitua E, Andia I. Preparation technique for PRGF. A new approach for bone regeneration. 2001. Vitoria-Gasteiz: Puesta Al Dia Publicaciones.29. Jankovic SM, Zoran AM, Vojislav LM, Bozidar DS, Kenney BE. The use of platelet-rich plasma in combination with connective tissue grafts following treatment of gingival recessions. Periodontal Pract Today. 2007. 4:63–71.30. Ando K, Ito K, Murai S. Improvement of multiple facial gingival recession by non-surgical and supportive periodontal therapy: a case report. J Periodontol. 1999. 70:909–913.
Article31. Pini Prato G, Pagliaro U, Baldi C, Nieri M, Saletta D, Cairo F, et al. Coronally advanced flap procedure for root coverage. Flap with tension versus flap without tension: a randomized controlled clinical study. J Periodontol. 2000. 71:188–201.
Article32. Zucchelli G, Clauser C, De Sanctis M, Calandriello M. Mucogingival versus guided tissue regeneration procedures in the treatment of deep recession type defects. J Periodontol. 1998. 69:138–145.
Article33. Caffesse RG, De LaRosa M, Garza M, Munne-Travers A, Mondragon JC, Weltman R. Citric acid demineralization and subepithelial connective tissue grafts. J Periodontol. 2000. 71:568–572.
Article34. Cheung WS, Griffin TJ. A comparative study of root coverage with connective tissue and platelet concentrate grafts: 8-month results. J Periodontol. 2004. 75:1678–1687.
Article35. Karring T, Cumming BR, Oliver RC, Loe H. The origin of granulation tissue and its impact on postoperative results of mucogingival surgery. J Periodontol. 1975. 46:577–585.
Article36. Lundberg M, Wennstrom JL. Development of gingiva following surgical exposure of a facially positioned unerupted incisor. J Periodontol. 1988. 59:652–655.
Article37. Del Fabbro M, Bortolin M, Taschieri S, Weinstein R. Is platelet concentrate advantageous for the surgical treatment of periodontal diseases? A systematic review and meta-analysis. J Periodontol. 2011. 82:1100–1111.
Article38. Griffin TJ, Cheung WS. Guided tissue regeneration-based root coverage with a platelet concentrate graft: a 3-year follow-up case series. J Periodontol. 2009. 80:1192–1199.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Clinical Results of Subepithelial Connective Tissue Graft for Root Coverage
- Root coverage with subeptithelial connective tissue grafts
- Laterally positioned flap using subepithelial connective tissue graft for iatrogenic gingival recession treatment
- Periodontal Wound Healing of the Experimental Subepithelial Connective Tissue Graft in Dogs
- The Clinical Study on the Root Coverage Effects with Free Standing Connective tissue Graft